Abstract
In the last decade, historical archaeologists in the American West have begun conducting biochemical analyses of contents in bottles recovered from archaeological sites dating to the late nineteenth and early twentieth centuries. Archaeological excavations conducted at the Alameda-Stone Cemetery Site provided a large amount of data about the residents of a Tucson, Arizona neighborhood that existed between 1889 and the 1950s. This was a transformative period in the pharmaceutical industry when university-trained pharmacists advanced their field and advocated against the use of mass-produced patent and proprietary medicines. The discovery of two sealed medicine bottles with intact contents provided an opportunity to examine medicinal products from bygone days. This analysis centered on the main question: What can archaeologists discover about the contents of historical bottles that were discarded and have been subjected to environmental conditions for decades? The bottle contents from Tucson were analyzed by gas chromatograph/mass spectrometry (GC/MS) to reveal the ingredients of the medicines and were compared with biochemical medicine analysis conducted at other sites in the American West. These results, in conjunction with historical and archaeological data, demonstrate archaeologically recovered medicines can provide insight into pharmacy and medicine ingredients used in the American West during the late nineteenth and early twentieth centuries.
Similar content being viewed by others
Introduction
By the early twentieth century, patent and proprietary medicine manufacture and sales was a huge industry in the United States. The Collier’s Weekly writer Samuel Hopkins Adams (1905-06) reported that Americans spent $75 million on patent medicines in 1905 alone. Inadequate municipal sanitation systems and growing cities meant illness was commonplace in the United States at that time, which provided a ripe population of willing medicine customers seeking relief. The patent and proprietary medicine industry grew through sustained and widespread marketing campaigns that included both print materials, testimonials, both true and fabricated, and live-action sales shows. During the nineteenth century, transportation networks brought mass-manufactured goods to all corners of the country. Medicine advertisements proceeded the products across the country. Unfortunately, not all medicines were effective, despite believable advertising claims boasting the efficacy of patent and proprietary medicines’ abilities to remedy, even cure, almost any ailment.
The growing community of medical professionals in the United States was aware of the negative impact patent and proprietary medicines were having on the reputation of the pharmaceutical industry. United States government officials were also aware that many of these medicines were negatively impacting citizens, but did not have a clear pathway toward resolving the problem because both university-trained pharmacists and entrepreneurial hucksters were selling medicines. The dividing line between professional pharmaceuticals and proprietary medicines was unclear:
It should be understood that in many cases there is no clear line of demarcation between what are commonly known as “patent medicines” and the “ethical proprietaries.” As has been shown time and again, it is not unusual for a nostrum first to be exploited only to the medical profession—as an “ethical proprietary.” After a sufficient number of testimonials have been received from unthinking physicians the promoters of the nostrum advertise their wares direct to the public—as a “patent medicine.” (American Medical Association 1912).
By the early twentieth century, newspapers led the charge against the patent and proprietary medicine industry in hope of creating reforms. The American Medical Association joined the crusade. Adams’s (1905-06) series in Collier’s, “The Great American Fraud,” is considered influential in bringing forth the Pure Food and Drug Act of 1906. The 1906 Food and Drug Act called for “dangerous” or “addictive” ingredients like alcohol, opioids, and cannabis to be listed on the label. The Act also recognized the United States Pharmacopoeia, which was produced by university-trained pharmacists and physicians, as the standard for drugs. Most importantly, the law established penalties for violating these regulations. The 1906 Act and subsequent legislation were detrimental to the patent and proprietary medicine industry because medicine manufacturers had to use known medicinal substances and limit or omit addictive ingredients. The patent and proprietary medicine industry started a long decline; whereas, the larger pharmaceutical industry continued to grow, the into a modern industry dominated by university-trained medicinal chemists and pharmacists. Today, medicines must also pass clinical trials before they can be sold or marketed to the public. A line had been drawn between medical professionals and medicine marketers.
Medicine bottles are commonly found at archaeological sites in the United States. Sometimes, these bottles contain residues of their former contents. Historical medicine formularies provide a wealth of information on how medicines were compounded by pharmacists, but they provide little information about patent and proprietary medicines because the formulas for these medicines were trade secrets. These formularies are also of little use for medicine residues in unmarked bottles or bottles where the contents are clearly not the same, for example pills placed in a bottle embossed with the advertisement for a liquid medicine. The formularies demonstrate late nineteenth- and early twentieth-century pharmacists and physicians were compounding medicines using a variety of ingredients with known beneficial effects. For example, terpenes like camphor had antibacterial properties that had been known for centuries (Claus et al. 1970: 160-164, 195-196). Formularies recommend the use of camphor in a number of different internal and topical remedies. Biochemical analyses provide a way for archaeologists to determine the composition of residues found in medicine bottles, which can provide insights into the ingredients and possible use of this medicine, and the sort of ailments it was designed to heal. Historical archaeological analysis of medicine residues conducted since 2007 can also provide insight into medical practices of the late nineteenth and early twentieth centuries and the strategies pharmacists took towards healing their patents. These analyses also provide insight into the contents of patent and proprietary medicines of that time period. Biochemical analyses, specifically mass spectrometry, are a way archaeologists can “ground truth” historical medicines, providing information on the contents and efficacy of these chemical artifacts.
Statistical Research, Inc. conducted an archaeological data recovery project from 2006 to 2010 in downtown Tucson for the Pima County Cultural Resources and Historic Preservation Office at the Historic Alameda-Stone Cemetery (AZ BB:13:682 [ASM]), which was a multicomponent site composed of prehistoric and historical archaeological features. Data recovery at this site included extensive archaeological excavations, documentation, archival research, and reporting. The cemetery was in use from the 1860s until the 1880s and the land was redeveloped as a mixed-use residential neighborhood between 1889 and the 1950s. It became part of the downtown commercial district after the 1950s. Excavation of the post-cemetery component at this 4.3-ac (1.7 ha) site encompassed approximately three city blocks of residences and businesses. During data recovery excavations 1,083 grave features and three prehistoric features were removed for analysis along with a total of 39 historical features were analyzed that included artifact scatters, trash pits, trash deposits, stairwells, privy pits, cesspits, and basements. A three-volume series completed in November 2010 was produced for the final reporting for the Alameda-Stone Cemetery Site Archaeological Project (Gray and Swope 2010; Heilen and Gray 2010; Heilen et al. 2010).
Post-cemetery archaeological work focused on the former residents of the Alameda-Stone Cemetery project area. Historical documents indicate these residents were primarily working- and middle-class people, primarily European Americans that had come to Tucson from across the United States and a number of foreign countries. They were part of a population surge that followed the arrival of the Southern Pacific Railroad in 1880 that changed Tucson’s physical, economic, and sociocultural landscape (Gray et al. 2010). With the arrival of the Southern Pacific, Tucson began the transformation from a remote outpost to an urban place integrated into the greater American economic, cultural, and transportation network (Sheridan 1986:55–56). The railroad that brought these new Tucsonans also brought new ideas and attitudes toward health and medicine. Archaeological evidence collected from medicinal bottles at this site indicates residents made health decisions in alignment with prevailing attitudes regarding medicine use.
Patent and Proprietary Medicines in the United States, 1880–1930
Residents of the Alameda-Stone Cemetery Site lived during a transitional period within the medical and pharmacological fields in the greater United States that resulted in profound changes and, ultimately, the creation of modern medicine. Prior to the early twentieth century, medicines of varying efficacy were manufactured and sold by physicians, pharmacists, and drug manufacturing companies. Before continuing, we must clarify the difference between patent and proprietary medicines. The term “patent medicine” has become colloquially applied to all products created by large companies and those made by individual physicians or pharmacists, especially for nineteenth-century medicines; however, there are differences between patent and proprietary medicines. Patent medicines, that is proprietary medicines made and marketed under a patent, are legally different than proprietary medicines, which is a preparation owned or controlled by an individual, group of individuals, company, or other entity. In the United States today, most new medicines use patents filed with the United States Patent and Trademark Office to protect their unique product from market competition or infringement by another entity. Patents are a property right that provides rights to the manufacturer for 20 years. Drug patent law is now complex but most new patented medicines can enjoy an exclusivity period of anywhere from three to seven years, which delays the production of competitor drugs. While drug patents had existed since the late seventeenth century in Europe, exclusivity could only be guaranteed through secrecy. Patents for chemical medicines were first created in the United States in 1925 (Bingham 1994; Young 1961). Proprietary medicines were sometimes patented but their affiliation with known physicists, pharmacists, or drug manufacturers was used as a demonstration of their efficacy and purity. Affiliations with proprietors was also used to increase sales. The fact that many nineteenth-century patent and proprietary medicines were not effective and, frequently, dangerous is what has tarnished their reputation, but many of these medicines contained at least some ingredients that were effective against pathogens and disease.
Patent and proprietary medicines dominated the pharmaceutical market in the American West during the late nineteenth century. Sales were fueled by convincing advertisement and the use of a range of ingredients like narcotics and alcohol. The print advertising industry fed from the rapidly growing profits of corporations and large businesses and influencing the way that everyday Americans lived and felt about their lives (Laird 1998; Young 1961). Very few medicines formally received a patent. University-trained pharmacists created proprietary medicines at this time, including some that were patented. While there were tens of thousands of proprietary medicines for sale during the late nineteenth century, only a small proportion of these were evaluated in a framework of medical knowledge along the lines of a modern clinical trial. It should also be noted that proprietary and patent medicines were oftentimes developed by trained pharmacists and physicians and, thus, were “professionally compounded” even though they had not undergone clinical trials. In addition to medicines made by individual pharmacists or physicians, large pharmaceutical supply houses compounded their own proprietary medicines that were, sometimes, patented with the United States Patent Office.
Medicine manufacturers promoted their products’ efficacy, although many made exaggerated claims. Patent medicine hucksterism hit a peak during the 1880s and 1890s– proliferating at this time through outlandish claims and exaggerated healing capabilities that were rarely delivered. Oftentime, patent medicines contained heavy doses of alcohol or opiates that made users feel as if the medicines were affecting illness. Print advertisements, sometimes accompanied by live presentations from salespersons, also exaggerated the efficacy of these medicines. Some were even reported to cure illnesses such as cancer, alcoholism, and drug addiction. Despite large sales and effective advertising, most patent and proprietary medicines did not contain ingredients that could achieve the claims reported in their advertisements. By the twentieth century, government agencies, investigative journalists, and physicians started speaking out against the most popular patent and proprietary medicines (American Medical Association 1912; Boyle 2013; Holbrook 1959). Patent and proprietary medicines were linked to thousands of drug addictions, overdoses, and poisonings across the United States. Despite the enactment of the Pure Food and Drug Act in 1906, patent medicines remained available and affordable and were used into the 1930s (Hodgson 2001:103–121: Linn 2008:356). The medicines with harmful ingredients and boastful advertising were not completely extinguished until the 1980s (Bingham 1994).
Pharmaceuticals created by a compounding pharmacist were an alternative to patent medicines, but pharmacists did not all have the same level of professional experience, were typically more expensive than patent medicines, and were rare in the American West. Rapid development in pharmaceutical medicine took place between 1880 and 1920, with a growing number of pharmaceutical professionals using scientific testing and chemistry to develop effective medicines to treat the wide range of diseases (Duffy 1978:135–136). Prior to the Civil War, much of a pharmacist’s time was used distilling the ingredients for medicines from raw materials. Pharmacists and drug supply houses of the time saw a need for large facilities that would distill and prepare medicine ingredients and sell them wholesale to pharmacists. Several large firms started producing basic pharmaceutical ingredients using profits gained by supplying the Civil War armies and sold these ingredients to pharmacists at wholesale rates. This decreased the workload of pharmacists and allowed them to focus on compounding medicines instead of extracting ingredients (Sonnedecker et al. 2002:66).
After the Civil War, medical professionals began reforming their trade and advocating that well-trained physicians and pharmacists should guide the field of medicine in the United States instead of patent medicine proprietors. These reforms resulted in the professionalization of medical practitioners and pharmacists, who increasingly used medicines that had undergone scientific testing. For most of the nineteenth century, qualifications for physicians and medical schools in the United States were not well defined and state government licensure was practically nonexistent. An amalgam of applied research institutions, including medical colleges with pharmacology departments, proliferated as more universities were founded (Hudson 1978; Swann 1990:76). In the last decades of the nineteenth century the practice of medicine became increasingly more professional and science-based in the United States, formalized with the incorporation of the American Medical Association in 1897. Clinical trials also became the basis for testing the efficacy of medicine (Duffy 1978; Hudson 1978). By 1900, medical practitioners widely accepted the validity of germ theory and applied sanitary medical practices, making their treatments more successful. Quality training institutions, scientific methods, and increasingly successful results, along with highly publicized patent medicine deaths, poisonings, and addictions, eventually convinced the American public that medical professionals provided a safe and effective service. By the early twentieth century, well-trained doctors and pharmacists were at the forefront of medical knowledge in the United States (Duffy 1978:136; Hodgson 2001).
Academic pharmacological research remained separate from commercial medicine in the United States until the 1920s primarily because university-trained pharmacists did not want to be associated with the proprietors of profiteering and unsavory patent medicine companies (Parascandola 1990; Swann 1990). While cooperation between university biomedical and pharmacology researchers and the pharmaceutical industry had been long established in Europe, particularly in Germany, collaboration in the United States was slower to evolve (Swann 1990; Tansey and Milligan 1990). Ethics were at the core of prohibitions against academic and industry collaborations in medicine. The medicine industry in the United States was seen as a vehicle of capitalism used to achieve profit above all else, while academic pharmacology was perceived as an avenue of pure research (Swann 1990:73-78). This changed between the 1920s and the 1940s when large pharmaceutical companies in the United States began following the European model and started extending research funding to universities. Commercial pharmacology research departments also expanded and improved at this time, profiting from university-trained medicinal chemists and accelerating the development of effective medicines in the United States (Swann 1990:79-85). Nevertheless, for the local pharmacist in the American West at the turn-of-the-twentieth century, prescribed medicines remained a combination of knowledge gleaned from centuries of folk medicines, personal experience, and scientific data. The best folk medicines were time-tested and well known by the public. The properties of useful compounds, such as volatile oils, were well understood by pharmacists and the recipes that employed these ingredients were varied and learned by heart. For a compounding pharmacist, the toolkit and recipe book for medicines remained the same because scientific medical data had not yet superseded traditional knowledge and synthetic chemicals had not yet been developed. Large pharmaceutical companies did not completely take over the research, development, and production of medicines in the United States until the 1940s (Sonnedecker et al. 2002).
To convince the American public that physicians and pharmacists were the authorities of medicine in the United States, however, the field had to overcome its checkered past. The painful and often unsuccessful methods employed by doctors and pharmacists prior to the Civil War caused most Americans to avoid medical professionals, preferring to rely on folk knowledge and remedies. Medically prescribed bloodletting, emetics (medicines that induce vomiting), and cathartics (agents that induce bowel evacuation) had decreased by the 1860s. Leeches, cupping (a treatment designed to draw blood to the surface using an empty cup), and blistering (using a heated rod to raise a blister on the skin surface) remained popular throughout the nineteenth century. Pharmacists at this time were seen as a better, but more expensive, source for wellness; prescribing medicines was commonplace and expected. Prescription medicine was frequently compounded at a local pharmacy or by a pharmacist, sometimes self-trained, who followed formulas or recipes from formularies or other medical literature. Pharmacists compounded medicines for patients based on a doctor’s prescription or the patient’s instruction. Pharmacists sometimes compounded medicines based on their knowledge of the effect of certain ingredients and the patient’s complaints. Medicines contained a mixture of herbs, spices, and distilled oils, resins, and tinctures that fought illness as much as produced a feeling that something was happening. Often, prescription medication ingredients were the same as those in patent and proprietary medicines (Sonnedecker et al. 2002). Americans viewed strong, professionally compounded drugs as the only reason to consult a doctor. For physicians, drug taking was therapeutically important and patients expected prescribed medicines to be administered; sometimes they were taken alongside the patent medicines they were already using. Doctors frequently recommended more than one medicine per visit. Private practitioners recommended even more (Rosenberg 1978:63–65).
Chemical Analysis of Medicines from Archaeological Contexts
Pharmacy historians and archaeologists have analyzed the ingredients of a small number of historical medicines from private collections and archaeological sites. While it is difficult to determine the efficacy of many of these medicines as they have undoubtedly deteriorated over the years, analysis suggests some of them did contain effective ingredients. Analysis of historical proprietary medicines show botanical ingredients such as fennel, cinnamon, and fenugreek were combined with alcohol. Some of these herbs had medicinal properties that would have been known in the United States. One example is the recent analysis of patented recipes for Lydia E. Pinkham’s Vegetable Compound (Tyler 1995). Lydia Estes Pinkham was born in Lynn, Massachusetts, in 1819 and was the tenth of a dozen children. A believer in abolitionism and temperance, Lydia married an entrepreneurial husband in 1843 and translated a book of family medicinal recipes during the 1850s. The Panic of 1873 wiped away most of Pinkham’s husband’s fortunes, so she decided to start selling different medicinal recipes in the Lynn area. By 1875, Lydia had expanded production of her Vegetable Compound—a treatment for women based on several spices, herbs and alcohol. The Vegetable Compound was among the Lydia Pinkham Company’s most popular product, even after Lydia’s death in 1883. The company remained in operation until it was purchased in 1968 by Cooper Laboratories, who moved production of Vegetable Compound from Lynn to Puerto Rico. Long-time customers continued to swear of the efficacy of Vegetable Compound as late as 2002 (Danna 2015).
Historical documents show that the popular nineteenth-century herbal compound Lydia E. Pinkham’s Vegetable Compound contained Unicorn Root (Aletris farinosa L.), Life Root (Senecio aureus L.), Black Cohosh (Cimicifuga racemosa [L.] Nutt.], Pleurisy Root (Asclepias tuberosa L.), Fenugreek Seed (Trigonella foenum-graecum L.), and 18% alcohol. The Vegetable Compound may also have contained false unicorn root (Chamaelirium luteum [L.]) (Tyler 1995:25). The recipe for this medicine may have changed over time as more than one recipe has been identified. Twentieth-century analysis of this recipe has proven that only black cohosh has properties that coincide with those reported by Pinkham. The compound was advertised as a remedy for female ailments like prolapsed uterus, irregular and painful menstruation, and inflammation of the womb. Düker et al. (1991) found that black cohosh (Cimicifuga racemose) was proven to aid with menopausal by relieving hot flashes. This eight-week clinical trial also showed black cohosh reduced the secretion of luteinizing hormone (LH) in women and ovariectomized rats. The reduced ovarian activity associated with menopause is associated with reduced estrogen production and an increase in LH, endocrine changes connected to hot flashes, depression, and insomnia. This research suggests black cohosh is an effective alternative treatment for women who do not respond to hormone replacement therapies (Düker et al. 1991). Black cohosh is still used in the United States to treat “menopause, premenstrual syndrome, menstrual cramping, preparation for childbirth, and, to a lesser extent, in products for rheumatoid arthritis and mild depression” (Betz et al. 2009:155). While the high level of alcohol in historical bottles of Vegetable Compound are unlikely to heal uterine ailments, at least one of its herbal ingredients has been proven to be effective treatment for menopause and, possibly, other female-specific ailments.
Another popular proprietary medicine, Lash’s Bitters, has also been subjected to chemical analysis in the hope of identifying the efficacy of the medicine’s ingredients. Chemical analysis of a bottle of Lash’s Bitters revealed that this proprietary medicine contained a range of chemicals including ethanol and lead, but did not contain therapeutic traces of the active ingredients purported on the label. In 1875, pharmacist John Speiker moved to Sacramento, California, entering into business partnerships that would result in the manufacture of several proprietary medicines, some of which were actually patented. By 1884, Speiker was manufacturing Lash’s Kidney and Liver Bitters along with several other medicines. Sales of Lash’s grew and Speiker’s company expanded throughout the remainder of the nineteenth century, with offices opening in Chicago (1901) and New York (1904). The company started by Speiker maintained its presence nationwide until 1929–1934 when all three corporate offices closed in quick succession (Torbenson et al. 2000b). Lash’s Bitters was advertised as a laxative made from an extract of the buckthorn tree (Rhammus purshiana), which contained the principal active ingredients anthraquinone and Danthron (Torbenson et al. 2000a, b:57–58). Mass spectrometry analysis of an unopened bottle of Lash’s in 2000 revealed the medicine contained ethanol, methanol, and a potentially toxic level of lead. The medicine contained over 19% ethanol, which is as much as sherry, and each tablespoon had 44 mg of lead, which would have been dangerous to pregnant women and children if taken for a long periods. This analysis did not reveal traces of anthraquinone or Danthron (Torbenson et al. 2000a, b). The alcohol in this product would have produced physiological feelings but it is unlikely this would have had a therapeutic effect.
The analysis of Lydia Pinkham’s and Lash’s Bitters show that proprietary and patent medicines were a mixed bag. Some, like Pinkham’s, did contain effective substances but also contained high levels of alcohol. Medicines like Lash’s had alcohol and potentially hazardous contents like methanol and lead, ingredients that did not fight illness. It is these inactive, ineffective, and potentially poisonous ingredients that soiled the reputation of proprietary and patent medicines.
Spectrographic Chemical Analysis of Historical Archaeological Medicines
The recovery of medicine bottles with traces of their former contents is not uncommon in historical archaeology, but it is rare for the archaeologists to subject these contents for biochemical analyses using spectrographic techniques. In addition to proprietary medicines like Pinkham’s and Lash’s, archaeologists have conducted analyses of contents from unsealed bottles recovered from archaeological sites. Since 2007, historical archaeologists in the United States have analyzed historical medicine bottle contents using at least four spectrographic chemical analyses techniques. This article covers medicines analyzed by the four methods listed in Table 1. In the case of historical medicines, spectrographic methods include biochemical analysis techniques based on measuring the light spectrum of substances as in an excited state (i.e., fluorescence) or as refracted light. Gas chromatograph/mass spectrometry (GC/MS) is considered the most detailed and accurate spectrographic analysis technique, but it is comparatively expensive and is typically only available to archaeologists working with a university’s medicinal chemistry department. The other techniques, fluorescence spectrometry, spectrophotometry, and ion chromatography, can be done with less intensive instruments available at most university chemistry departments.
Of these four spectrographic analysis techniques, gas chromatograph/mass spectrometry (GC/MS) is a combination of spectrometry and chromatography and is widely recognized as an accurate way to detect very specific substances. GC/MS is a type of analysis that can be used to analyze historical substances at the atomic level, measuring the mass-to-charge ratio of charged particles and is useful in identifying unknown compounds. Mass spectrometry measures chemical ions present in a vaporized chemical sample as they appear during a scan. As the vaporized chemical fluoresces, it gives off a light spectrum that is measured by the spectrometer. Each known chemical has a unique signature, or “fingerprint,” that can be identified based on the time it fluoresces during the scan and the light spectrum that is produced. For unknown compounds, such as historical-period medicines, the light spectrum “fingerprint” for each sample can be compared against known chemicals to establish the identity of an unknown substance. GC/MS analysis of archaeological materials is important because it provides a method to identify the constituents of organic artifacts that have been recovered and provides an opportunity to learn what substances were available and used in the past.
While the measurement of chemicals and unidentified substances with a GC/MS is reliable and valuable for archaeologists, the technique does have some limitations that have implications for archaeological analogy. One limitation is created by the weathering of archaeological materials that have been exposed to erosion, which accelerates the deterioration of bottle contents. Temperature change and air and water infiltration have the potential to degrade bottle contents. Identifying water-soluble substances or substances subject to evaporation, such as opiates and alcohols, are particularly difficult because erosion deteriorates them quickly (Schablitsky 2006:15). Other limitations of GC/MS are related to the operation of mass spectrometry machinery and software. Chemicals in a mass spectrometry comparison database, which is used to identify the organic compounds in the bottles, have not been calibrated to account for the natural decomposition of chemicals and artifacts over time. The database can only identify the presence or absence of a content but cannot detect its purity. Also, samples of the historical substance must be manufactured in the laboratory in order for the spectrometer to have something to detect. These samples are created by extracting the historical bottle contents and mixing them with a solvent of some type, usually an organic compound such as dichloromethane (CH2Cl2), a process that is particularly useful for volatile compounds, or methanol (MeOH) for water soluble substances. The nature of GC/MS, which essentially burns part of the sample in order to create a spectrum, favors the identification of volatile compounds that fluoresce during the scan while extracted by a solvent. This means that volatile substances are easily identified while the detection of other less volatile or degraded chemicals is more difficult. Fluorescence is also an issue for residual chemicals because GC/MS does not always detect chemicals that may be present at a lower density and may not be concentrated enough to fluoresce (Somogyi, pers. comm. 2009).
Ray von Wandruzka, Mark Warner, and other scholars affiliated with the University of Idaho, have led the way in biochemical analysis of archaeological bottle contents, having analyzed dozens of historical substances since 2010. This research has demonstrated the efficacy of spectrographic analysis on historical bottle contents and has opened avenues for investigating turn-of-the-twentieth-century pharmacy in the American West. Thus far, most of their published data comes from two specific sites in Idaho—a historical commercial district in Sandpoint and a former garbage dump in Nampa. Between 2005 and 2008, a project conducted by archaeologists from the University of Idaho and sponsored by the Idaho Transportation Department (ITD) during the Sand Creek Byway project in Sandpoint, Idaho, led to the recovery of between 30 and 40 bottles with traces of their former contents (Warner 2014; Weaver 2014). Conducted from 2006 until 2013, the project centered on a historical industrial and commercial district on the Sandpoint waterfront. Thousands of artifacts from features created between the 1890s and early 1900s were recovered and analyzed. The medicine bottles submitted for chemical analysis dated from the late nineteenth to early twentieth centuries and had undergone changes due to exposure to air and water since deposition (Spinner et al. 2011:30; Warner 2014:276–281). The contents of twelve bottles and the filling of an adult human molar were analyzed using fluorescence spectrometry, spectrophotometry, and ion chromatography (Spinner et al. 2011:31). From these several types of analyses, scholars were able to determine the contents of a dandruff treatment, a hematinic, wood tar, zinc ointment, hair dye, facial cream, perfume, dentifrice, jam, paint, rodent poison, mechanical grease, and the materials used in the human tooth’s filling (Spinner et al. 2011; Warner 2014). Salvage excavations conducted in 2009 at a former dump in Nampa, Idaho, led to the analysis of 11 additional historical bottle contents dating to the turn-of-the-twentieth century (Von Wandruszka et al. 2016). These substances were subjected to analysis similar to those recovered from Sandpoint, which revealed the bottles contained medicines and grooming products including an antacid, laxative, Mentholatum, activated carbon, and a lotion (Von Wandruszka et al. 2016). Biochemical analysis has also been conducted on smaller archaeological collections of bottles from other sites to identify their ingredients, including bottles containing medicine and lotion residues recovered from a Chinatown in San Jose, California (Voss et al. 2015).
Each of these studies demonstrates the efficacy of spectrographic biochemical analyses in identifying residues in historical bottles. Based on their experience using spectrometry to analyze historical bottle contents, von Wandruszka and Warner (2018) have summarized practical approaches to the chemical analysis of historical bottle contents and have outlined a “best practices” guide. They explain that the contents of sealed bottles are excellent candidates for biochemical analysis. Von Wandruszka and Warner also state that liquids often contain water soluble ingredients and tend to evaporate over time. In addition to natural dissolution, bottle contents can react with elements in the glass bottles and metal container closures, further complicating the analysis results. Nevertheless, these experiments show spectrographic analyses can still yield fruitful results from the undissolved remains of bottles that formerly held liquid medicines.
In addition to research conducted by archaeologists in Idaho, the author of this article has also subjected bottle contents recovered from sites in Washington State to mass spectrometry in the hope of identifying medicinal contents from medicine bottles. In 2007, archaeological data recovery was conducted at the Japanese Gulch Site in Mukilteo, Washington. The site dated to the late nineteenth/early twentieth century and excavations focused on deposits created by a community of Japanese mill workers employed at the now extant Crown Company Lumber Mill. A bottle marked “Poison” was recovered along with medicine and toiletry bottles and bottle fragments, including the remains of bottles formerly containing Mentholatum, Vaseline, and lotion made by the Melba Manufacturing Company (White et al. 2008a). The Poison bottle was analyzed using mass spectrometry at the University of Washington’s Department of Medicinal Chemistry to reveal that it contained degraded mercuric chloride—a potentially hazardous substance that was once used to treat syphilis (Howald, pers. comm. 2007; Merck & Company 1940:1127). Despite being buried for decades, the bottle contents were out-gassing chlorine gas that was released as the bottle’s cork dried after excavation. The bottle contents were properly disposed of at the University of Washington (White 2012).
A second assemblage of bottle contents recovered from the Teager/Weimer Site in Arlington, Washington, was submitted for analysis at the University of Washington in 2008. The bottles were recovered from a privy associated with a house occupied by Dr. Calvin and Mertella Teager from 1892 until 1911, before this property was bought by Joe and Hilda Weimer in 1917. Mertella Teager was a licensed pharmacist, the proprietor of a drug store, and the town’s first schoolteacher (Stillaguamish Valley Genealogical Society 2003). Medicine bottles included the remains of proprietary and pharmacy bottles, including one from the Arlington Drug Company of Arlington, Washington (White et al. 2008b). Nine, sealed, unmarked medicine bottles with traces of their former contents were analyzed by mass spectrometry. This analysis yielded information on the contents on only seven of these bottles. The contents of one bottle (Catalog No. 1304) had separated into a biphasic liquid. Both layers of this medicine were tested separately. As shown in Table 2, they contained ingredients for medicines made from a range of aromatic oils, fatty acids, sugars, sugar alcohols, and petrochemicals. While water soluble ingredients like alcohol had mostly leached from the bottles, the detectable ingredients suggest these bottles contained medicines to treat gastrointestinal ailments or serve as skin moisturizers or skin treatments (White et al. 2008b).
The mass spectrometry analysis identified a number of compounds typically used in nineteenth-century medicines consistent with the occupations of the owners, one of whom was a pharmacist. Profiles were compared using two historical references with sections devoted to medicines: Dr. Chase’s Recipes; or Information for Everybody by A.W. Chase (1864), The Household Cyclopedia of General Information by Henry Hartshorne, M.D. (1881), and other pharmaceutical history articles. These references indicate that pharmacists of the nineteenth century relied heavily on age-old medicinal substances and mixed them based on preferred recipes (Table 3).
Spectrographic chemical analysis of medicines from Arlington and Mukilteo, Washington, had similar contents as those from Sandpoint and Nampa, Idaho. These studies show that turn-of-the-twentieth-century medicines were compounded from a wide range of contents. Aromatic oils that had been used as effective remedies for centuries were among the more effective ingredients. These oils were mixed with fatty esters, sugars, and other agents to give them properties suitable for internal consumption or external use. These studies also show that spectrographic analysis can identify unknown substances remaining in archaeological bottles, including potentially hazardous chemicals like mercuric chloride and lead. While biochemical analysis revealed proprietary medicines from that period, like Lash’s Bitters, contained potentially hazardous ingredients, medicines like Lydia Pinkham’s and medicines created by compounding pharmacists did have ingredients with medicinal properties. The advertised efficacy of patent and proprietary medicines was frequently inflated but analysis show medicines at that time, at least ones compounded by pharmacists, did contain beneficial ingredients. Medicine at this time was inconsistent to say the least; although, the ratio between effective professionally compounded medicines and useless, ineffective patent and proprietary medicines is unknown.
Medicines from the Alameda-Stone Cemetery Site
Established in 1775, Tucson residents have been subjected to the full range of eighteenth-, nineteenth-, and twentieth-century Spanish, Mexican, and American medical practices. Doctors or surgeons are not noted in Tucson during the Spanish and Mexican Periods (1775–1848). Older Spanish, Mexican, and Native American women, who knew native remedies and medicinal plants, were the doctors and pharmacists at this time (Quebbeman 1966:9–17). During the American Period (1848–Present), medical professionals were concentrated on military posts during the 1850s and 1860s, although a few doctors worked out of Tucson. Two doctors were present in the town in 1860 and memoirs suggest a doctor was present as early as 1858 (Quebbeman 1966:23–38, 43). Charles Herman Meyer is an example of the typical doctor in the Arizona Territory during the mid-nineteenth century. Born in Germany in 1821, Meyer arrived in Tucson in 1859 and opened a drug store. While Meyer had no professional training, he practiced as a surgeon, pharmacist, doctor, and judge throughout the 1860s (Quebbeman 1966:85–87). The number of doctors increased during the 1860s as the United States Army expanded their presence in the Arizona Territory and by the 1870s Tucson was large enough to support a small number of medical practitioners. Dr. John C. Handy played a central role in the Tucson medical community. Arriving in 1871, Handy was a prominent doctor and a guardian of ethical medicine in the town—challenging all Arizona Territorial doctors to produce a diploma and enacting a law to “Encourage Scientific Medicine and to Prevent Quackery.” Through advocacy spearheaded by Handy, the Arizona Legislature adopted a law in 1873 that imposed a fine for any unqualified person that practiced medicine or pretended to be a medical professional to the public (Quebbeman 1966:90–92). This law decreased the influx of unsavory medical hucksters into Tucson, but Arizona Territory still had a number of doctors without a certificate or diploma well into the twentieth century. During the 1880s and 1890s, medicines were sold at Arizona Territory drug stores by professional pharmacists, untrained clerks, and store owners with no medical credentials (Quebbeman 1966:229). The formation of the Arizona Medical Association in 1892 did much to legitimize university-educated doctors and pharmacists in the territory, but patent medicine use continued into the twentieth century (Quebbeman 1966:230–234).
During the 1880s, a proliferation of diseases in Tucson was associated with unsanitary urban conditions and population growth. Tucson was the largest town in the Arizona Territory at the close of the nineteenth century and unsanitary conditions prevailed throughout the town. The smelly water piped into the town in 1885 was considered unfit for human consumption. A sanitary sewer system was not established until 1901. Tucsonans lived in close proximity to animal pens and corrals, overflowing privies, and garbage in open spaces that contributed to the spread of communicable diseases such as typhoid, smallpox, tuberculosis, diphtheria, and malaria. Disease epidemics were common throughout the 1870s, 1880s, and 1890s (Quebbeman 1966:150–173). In Tucson, typhoid and smallpox remained annual threats into the twentieth century. Privies and cesspits were the most common way to treat human waste until sewers were installed in the Alameda-Stone Cemetery area in 1902–1903. Medicine bottles from the site suggest gastrointestinal distress from common milk-borne and waterborne ailments were common in Tucson at this time (Heilen and Gray 2010:377–379). Sanitation-related mortality in Tucson mirrored trends in other cities in the United States. Prior to 1920, urban mortality in the United States was higher than it was in rural areas (Haines 2001). The relationship between disease and sanitation conditions was not well known during the late nineteenth century in the United States. Public works, specifically water systems, were frequently contaminated with sewage from privies and cesspits. Untreated effluent was routinely discharged into watercourses. Sanitation developments were motivated by the better understanding of germ theory, urban growth, progressive groups who pressured lawmakers to use sanitation experts to solve the problem of increasing waste, and responsive municipal governments who attacked the problem (Melosi 2000:103). As a result, wastewater and sewer treatment in urban areas of the United States rose from 50% of the 1870 urban population to 87% by 1920 (Melosi 2000:152). While progress was not uniform for all classes and races, urban death rates declined steadily well into the twentieth century (Haines 2001).
During this time, doctors and pharmacists in Tucson and other Ameriacn cities used effective medicines whenever they were available, but turned to patent medicines when medicinal ingredients could not be obtained. In Tucson, patent medicines proliferated; a number of doctors owned drug stores and sold proprietary medicines along with compounded medicines (Quebbeman 1966:229-230). The Pure Food and Drug Act of 1906 mandated drug manufacturers to list medicine ingredients on packaging, which was detrimental to the patent medicine industry. Arizona was not yet a state, but these regulations still applied. Patent and proprietary medicine usage in Tucson and the rest of the United States drastically decreased, but was not eliminated (Harmon 2003).
Medicine-related artifacts recovered from the Alameda-Stone Cemetery Site provide useful information on medicine use throughout the time period when this location was a residential neighborhood (1889–ca.1950) and the types of ailments that were being treated. These artifacts indicate site residents purchased both patent and professionally compounded medicines to treat their illnesses. A total of 1,405 medicine-related artifacts representing at least 840 items were recovered from post-cemetery archaeological features. For archaeological analysis, the medicine-related artifacts category focused on medicine bottles, bottle closures, tins, and medical paraphernalia like dose cups, syringe barrels and plungers, and ampoules. Medicine-related artifacts were separated from personal hygiene products, which were primarily health and beauty aids (e.g., razors and cold cream containers) and personal sanitation equipment (e.g., douche paraphernalia and urethral irrigators). Medicine containers (MNI = 816) were overwhelmingly glass fragments from patent medicine bottles. Patent medicine bottles represented nationally distributed products such as Pitcher’s Castoria, Bromo-Seltzer, California Fig Syrup, Dr. King’s New Discovery, Chamberlain's Cholic and Cholera Remedy, Perunia, and Lydia Pinkham's Vegetable Compound. Most patent medicines at this site were advertised to treat gastrointestinal or respiratory ailments (Fike 2006; Gray et al. 2010:367–371).
A small number of prescription bottles in this assemblage provided information on the pharmacists that filled prescriptions for site residents. Only 2% (MNI = 17) of medicinal artifacts were the remains of bottles made for pharmacies or drug stores. About 47% of these prescription bottles (MNI = 8) could be traced to two Tucson pharmacies: the Arcadian and the Fleishman Pharmacies. The Arcadian Pharmacy is listed at 22 E. Congress Street between 1897 until 1907 in Tucson City Directories (Gray et al. 2010:370; Gray and Swope 2010:96). The Fleishman Pharmacy opened in the 1880s at 179 W. Congress Street and later moved to 21 E. Congress in 1901. Fred Fleishman started as an employee at the drug store owned by early Tucson medical practitioner Charles Meyer. Fleishman eventually became president of the Arizona State Board of Pharmacy (Gray and Swope 2010:130). Both of these locations are less than 0.5 mi (0.8 km) east of the Alameda-Stone Cemetery Site. Arcadian Pharmacy bottles were obtained from archaeological strata of privies and cesspits that had median manufacture dates (MMD) ranging between 1898 and 1908. These strata are associated with European American families (i.e., household members of European descent born in the United States) that lived at the site between 1899 and 1924 (Gray and Swope 2010:94–100,113–123,138–141). The Fleishman Pharmacy bottle artifacts came from privies and cesspit strata that had MMDs between 1902 and 1910; a period when a number of different European American families lived at these addresses (Gray and Swope 2010:113–123,222–237).
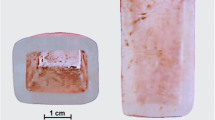
Two prescription bottles contained the remains of their former contents, which provided a unique opportunity to test professionally compounded historical-period medicines with modern technology. Neither bottle was embossed; the exterior of one bottle had some illegible paper label fragments. These two particular bottles could not be traced either to a pharmacy or patent medicine manufacturer. One prescription bottle (artifact number 08000D1355) was found in Stratum I of privy pit 10214 and contained the remains of a liquid medicine (Fig. 1). This artifact was recovered from a feature containing artifacts made between 1888 and 1904 deposited by a number of European American families that rented the dwelling at this address between 1896 and 1937 (Gray and Swope 2010:278–280). Another prescription bottle (artifact number 08000308F) contained a number of hand-rolled pills (Fig. 2). This artifact was recovered from Stratum IV of cesspit 3042, which has a MMD of 1906 and has been attributed to a rental dwelling constructed around 1896 and occupied until 1938. All known residents of this dwelling were European Americans (Gray and Swope 2010:309–310, 324–334). The historical-period medicines in these two bottles were subjected to gas chromatograph/mass spectrometry analysis to determine their ingredients.
Mass Spectrometry Analysis Methods and Results
The two medicine bottle contents recovered during the Alameda-Stone Cemetery Project were considered intact enough to be subjected to mass spectrometry analysis, which was conducted by Dr. Arpad Somogyi, formerly the Director of the Mass Spectrometry Facility in the Department of Chemistry at the University of Arizona, now at Ohio State University. All of the two bottle’s contents were subjected to rigorous testing that included analyzing the samples with four separate instruments: a liquid chromatograph quadrupole (LCQ) electrospray ionization (ESI) mass spectrometer, a high-performance liquid chromatograph (HPLC) mass spectrometer with ESI, a Fourier Transform Ion Cyclotron Resonance (FTIC) mass spectrometer, and a gas chromatograph mass spectrometer with electron ionization (EI). Two different extracts were used on each of these four instruments—one in CH2Cl2 (dichloromethane) and MeOH:H2O (methanol, monohydrate) (Somogyi, pers. comm. 2009). Each of these instruments is designed to detect ionized compounds using different variations on mass spectrometry and have different resolutions and accuracy ratings. Since GC/MS provided limited information only on volatile components, electrospray ionization in both positive and negative ion modes were also performed. These scans revealed these samples were complex.
One of the tested bottles had the remains of an unknown, liquid medicine that had separated into a liquid that overlaid a brown solid substance (see Fig. 1). Both the solid and liquid phases of the contents were subjected to analysis by all four mass spectrometry instruments. Three compounds were detected on all four instruments in the sample from this bottle: camphor, phenol, and palmitic acid (Somogyi, pers. comm. 2009). Camphor is a ketone volatile oil that is known for its effervescent, cooling effect on the skin (Tyler et al. 1988:124). Phenol is another volatile oil used medicinally for its antiseptic and anesthetic properties (Tyler et al. 1988:127). Palmitic acid is between 35 and 45% palm oil and is used in rubber and latex manufacturing, plastics, greases, lubricants, food additives, cosmetics, and toiletries. It is also a plasticizer used in pharmaceuticals (Claus et al. 1970:151).
The compounds identified in the liquid medicine are suggestive of an internal antibacterial antiseptic or a topical liniment. Volatile oils in the terpenoid group, such as camphor and phenol, were valued not only for their aromatic qualities, but also known as an effective antibacterial medicine (Claus et al. 1970:160-164). At the close of the nineteenth century, terpenoids were typically used in topical liniments, salves, and ointments, and internally as an antiseptic and vermifuge after being mixed with sweeteners (Chase 1864; Hartshorne 1881). Vermifuges were medicines used to kill gastrointestinal parasites. Recipes for liniments and vermifuges in nineteenth-century pharmacy books frequently utilized terpenoids.
The other artifact, a small amber pill bottle, contained at least 30 hand-rolled pills that were sampled and submitted for mass spectrometry analysis (see Fig. 2). Prior to mechanized pill production of the twentieth century, pills were split into a measured dose with a pill machine or pill press and were rounded into a pellet by hand (Sonnedecker et al. 2002:39). The bottle was made for the Parke Davis Company between 1875 and 1930 (Griffenhagen and Bogard 1999:86-87; Whitten 2019). Parke Davis is a large pharmaceutical company founded in 1871 in Detroit, Michigan. During the late nineteenth century, Parke Davis designed and developed specific bottles for their medicines that were made for the company by larger glassworks. The color of this bottle was designed to protect medicines from deterioration by sunlight (Griffenhagen and Bogard 1999:86-87). By the early twentieth century, Parke Davis was at the forefront of scientific pharmacology in the United States and operated a commercial laboratory (Parascandola 1990:33). Despite the fact that this bottle was designed for use by Parke Davis, it is unknown if the vessel was reused by a compounding pharmacist outside the company.
Mass spectrometry revealed a large number of chemical compounds in the pills and a vastly more complex chromatogram than the liquid medicine. Because of the extreme precision of FTMS, over 1,500 compounds were detected in this medicine; essentially, the FTMS detected chemicals throughout the entire scan and when the chromatograph is analyzed closely each peak appears to indicate a group of compounds instead of a single substance. These are mostly a homologous series of saturated and unsaturated hydrocarbons. A complete interpretation of this scan is beyond the scope of this article, but the scan revealed a large number of fatty acids, unsaturated fatty acids, and mono- and triple-oxygenated compounds and their derivatives. These compounds are indicative of a large number of naturally occurring fats and esters. The analysis also indicated the presence of natural oil components trapped either in the pellet matrix or on the surface of it (Somogyi, pers. comm. 2009). A few of these compounds appear to be substances detected in other medicine bottle contents analyzed by mass spectrometry, compounds widely found in a large number of naturally occurring oils and fats. However, it is unknown if they are medicinal ingredients, decayed remnants of these ingredients, or chemicals absorbed after the pills were deposited. The pharmacological properties of this medicine could not be determined.
In previous archaeological research, the author has submitted the contents of 14 historical-period medicines for mass spectrometry analysis; a total of 16 medicines including those from the Alameda-Stone Cemetery Site (see Tables 2 and 3) (White 2007, 2012; White et al. 2008a, b). All of these medicines came from subsurface features at six different historical archaeological sites that date to the same time as the post-cemetery period at Alameda-Stone. Except for the pills, all of these medicines were liquids. A range of volatile oils and fatty esters were identified in mass spectrometry of the liquid medicines but the GC/MS never revealed that these liquids had more than eight compounds. It is interesting to note that the pills from contained more than 1,500 compounds. These results may suggest solid medicines decay differently than liquid medicines after their deposition in archaeological deposits. The reasons for this differential decay are unknown but several causes can be speculated upon. First, liquids dissipate into the surrounding sediments more readily than solids. Most liquid medicines were recovered from bottles with simple cork closures or decayed metal screw tops and these seals had usually been compromised by the time they were recovered. It is very likely that water soluble organic compounds in the liquids dissipated through natural processes after deposition while volatile organic oils, which are not water soluble, were identified in liquids during mass spectrometry. The fatty esters and naturally occurring fats used to form the pill may have prevented the medicine’s ingredients from dissipating as easily into surrounding sediments. Also, the decayed traces of the original ingredients in the solid pills may also have been detected as different compounds because, as they decayed, the complex structure of these compounds may have degraded into more basic compounds. These factors would result in a situation where liquids appear to have few ingredients and solids actually appear to have more ingredients.
Another explanation for the high number of detected substances in the pills involves the absorption of modern chemicals by the pills after they entered the archaeological record. Chemical scientists have developed an impressive number of compounds during the twentieth century after the pills were deposited, many of which may have been absorbed by the pills. While water-soluble, organic compounds appear to escape from liquid medicines, but the fatty esters in the pills may have acted as sponges that absorbed and trapped additional, modern chemical compounds after deposition. A third explanation involves pharmaceutical practices during the turn-of-the-twentieth century. If the pharmacist that rolled these pills failed to properly clean the pill press used, the mass spectrometer would have detected residues from the ingredients in all of the medicines he compounded with that tool. Essentially, the mass spectrometer may have detected all the medicinal substances used at this pharmacy. This is a plausible explanation for the large number of naturally occurring fats and esters that were detected, which were historically used as binding agents for the active ingredients in pills.
The most likely reason for the vast number of compounds detected during the GC/MS scan of the pills is a combination of any, all, or even more of the factors mentioned above. The author remains perplexed by the reason why the solid medicine (i.e., hand-rolled pill) had such a dramatically different result when subjected to mass spectrometry analysis. It is possible that there would have been different results had the pills been tested at different layers (i.e., splitting a pill in half and testing millimeter-thick layers or testing the cortex material then the inner core of the pill). Additional analysis of other solid medicines is necessary to shed more light on this anomaly.
Conclusion
A large artifact collection deposited between 1889 and the 1950s by the residents of a Tucson neighborhood was collected during archaeological data recovery conducted for the Alameda-Stone Cemetery Site. Data collected from post-cemetery archaeological features provide insight into the lives of those who came to town during a transformative period in Tucson history. These new Tucsonans had been and continued to be influenced by the social, technological, and economic trends that were taking place across the country at that time. One of those trends was the scientific and technological advancement in the medical and pharmaceutical fields. The post-Civil War pharmaceutical field was dominated by patent medicines and the companies that made, distributed, and advertised them. Medicines were unregulated and contained alcohol, opiates, and other hazardous substances. Most doctors at this time were self-taught or, frequently, imposters working to sell medicines. Beginning in the 1860s and accelerating after the 1880s, university-trained, science-oriented doctors and pharmacists proliferated and worked to change the public perception of medical practitioners. Medicinal chemistry departments at universities began forging links with large medicine manufacturers through their alumni and industry-funded research. The result of these changes was more effective medicines, well-trained pharmacists, and general acceptance from the American public. Medicine-related artifacts from Tucson were the product of this transitional period.
Data from the Alameda-Stone Cemetery Site reveals that while medical professionals were working to decrease the proliferation of patent medicines, Tucson residents continued to prefer the affordable and readily available patent medicines. Tucson pharmacists sold patent and proprietary medicines, but Tucsonans of the late nineteenth and early twentieth centuries appear to have rarely used professionally compounded medicines to cure their illnesses. Compounded medicine remains sampled by mass spectrometry indicate pharmacists in Tucson used effective ingredients such as volatile oils that were time tested cures. Other organic substances, such as fatty acids and esters, were used as binding agents that probably suspended the medicine’s active ingredients. The solid pill suggests water soluble organic compounds in medicines seem to dissipate after deposition unless they are kept together with a bonding agent like naturally occurring fats or are not water soluble. Solid medicines also appear to contain a vast number of compounds when compared with liquid medicines.
The biochemical analysis of medicine bottle contents collected from archaeological sites is a growing research domain with large potential. Analysis of liquid bottle contents shows professionally compounded medicines contained ingredients with proven antibacterial, antimicrobial, and anti-inflammatory properties. Camphor and phenol, aromatic oils found in the samples from Tucson, were valued not only for their aromatic qualities but also have been known by healers for thousands of years. In the nineteenth century, these aromatic oils were typically used in topical lineaments, salves, and ointments, and internally as an antiseptic and vermifuge. It is unknown if this was an internal or external medicine but sweeteners were commonly added to oral medicines to make them more palatable because medicines relying on these oils and other alkaloids would have tasted bitter, sour, or astringent (Chase 1864; Hartshorne 1881). While sweeteners were not found in the Tucson samples, spectrometry on other medicines from Washington State contain substances like propanoic acid, fructose, and phosphoric acid that might have been residues from these sweeteners. In addition to aromatic oils, the samples from Tucson also contained fatty acids and esters that were probably used to keep medicinal ingredients in suspension until they could be consumed and absorbed in the stomach. This is consistent with analysis from Washington State where several different naturally occurring fatty acids, glycerides, and cholesterol were probably used to keep the medicinal contents in suspension until they were consumed or used.
Biochemical and medicine bottle analysis from other sites also shows some proprietary medicines may have contained effective ingredients used in medicines compounded by pharmacists, like aromatic oils. For example, von Wandruzka et al. (2016:220) analyzed a bottle containing Mentholatum using fluorescence spectrometry, revealing it had traces of menthol and petroleum jelly. Other non-biochemical research shows aromatic substances were used to treat illness in other contexts. Meredith Linn (2008) describes how aromatic balsams and sap were mixed with alcohol and other medicinal herbs in common remedies for respiratory ailments among Irish immigrants in New York City during the nineteenth century. However, caution must be maintained as it is unknown if the balsams from New York actually contained aromatic oils noted in their advertisements. Infusions of alcohol and plant materials were common among Irish folk remedies, so proprietary medicines advertising these ingredients were widely purchased upon arrival to the United States. When mixed with aromatic oils, these proprietary medicines may have given a convincing tingling sensation and familiar olfactory response that assured customers of the medicine’s efficacy even though its properties remain specious (Linn 2014). These medicines may have relieved some symptoms but are unlikely to have cured respiratory diseases like tuberculosis. It is this inability to trust proprietary medicines that motivated some Americans to choose professionally compounded medicines whenever possible. Jean Howson’s (1993) analysis of medicine bottles from the Sullivan Street Site in New York City shows, during the late nineteenth century, proprietary medicines were commonly used by all site residents, but working-class tenants consumed more proprietary medicines than prescribed medicines. The working-class also used more proprietary medicines than affluent neighbors. The house of a doctor yielded the most medicine bottles but contained very few proprietary medicine bottles; whereas, working class neighbors consumed both proprietary and professionally compounded medicines, preferring patent medicines until after the turn-of-the-century. This work suggests urban Americans recognized the superiority of pharmacist’s work but still used proprietary medicines. The formulas of some of these proprietary medicines contained aromatic oils like camphor and eucalyptus in combination with other botanicals like anise, chinchona, and castor oil in suspension with alcohol (Howson 1993); nowever, none of these have been subjected to biochemical analysis to confirm the presence or absence of these ingredients.
In a larger archaeological context, medicine bottles from the Alameda-Stone Cemetery Site suggest European Americans of the American West had a strong preference for patent medicines even when compounded medicines were readily available. Some historical archaeologists have attempted to make a correlation between ethnicity and patent medicine use. Brighton (2005) and Linn (2008, 2014) have noted that urban archaeological sites associated with Irish immigrants have larger percentages of patent medicine-related artifacts versus compounded medicines. Archaeological sites attributed to overseas Chinese communities have noted the continued use of Chinese medicines as seen through artifact assemblages (Voss et al. 2015); however, Chinese immigrant sites also include patent medicine-related artifacts (Stapp 1990; Wegars 1991). Archaeological sites associated with overseas Japanese workers also appear to have used patent medicines in conjunction with Japanese medicines whenever they were available (Ross 2009). The known residents who created the features where these medicines were recovered at the Alameda-Stone Site were European Americans, either first or second-generation Americans living in a US territory. Data from Alameda-Stone corroborate that Americans, including residents of middle-class European American communities, preferred patent medicines into the twentieth century even though they had access to medicines compounded by a pharmacist.
Spectrographic biochemical analysis conducted on medicines at the Alameda-Stone Cemetery Site indicates turn-of-the-twentieth-century pharmacists compounded medicines from a reliable toolkit of time-tested ingredients. Volatile oils detected in both medicines have valued for their medicinal properties for thousands of years and continue to be used today. The results from the liquid recovered from this site mirror that of other archaeologists (von Wandruszka and Warner 2018), but the mass spectrometry results for the pill differ from what has been previously found. Mass spectrometry can be employed to address a range of research questions that can provide insights into the effectiveness and ingredients in historical-period medicines, tools available to pharmacists, and the way organic substances decay after deposition. The way solid pills absorb environmental chemicals also provides an avenue to investigate how urban pollution can impact historical archaeological deposits. Comparisons between medicines in curated collections and those collected from archaeological contexts is also recommended. Few historical-period medicines have been analyzed by mass spectrometry, and archaeologist and medicinal chemists do not have enough information to answer these questions. More medicines need to be analyzed in order to improve our understanding the development of modern medicine, pharmacy, and how effective medicines were at treating disease.
References
Adams, S. H. (1905–1906). The Great American Fraud. Kindle. Accessed December, 2019.
American Medical Association (1912). Nostrums and Quackery. 2nd ed. American Medical Association Press, Chicago.
Badal, S. and Delgoda, R. (eds.) (2017). Pharmacognosy: Fundamentals, Applications, Strategies. Elsevier, Amsterdam.
Betz, J. M., Anderson, L., Avigan, M. I., Barnes, J., Farnsworth, N, F., Gerdén, B., Henderson, L., Kennelly, E. J., Koetter, U., Lessard, S., Low Dog, T., McLaughlin, M., Naser, B., Osmers, R. G. W., Pellicore, L. S., Senior, J. R., van Breemen, R. B., Wutte, W., and Cardellina III, J.H. (2009) Black Cohosh: Considerations for Safety and Benefit. Nutrition Today, 44(4):155–162.
Bingham, A. W. (1994). The Snake-Oil Syndrome: Patent Medicine Advertising. Christopher Publishing House, Hanover, MA.
Boyle, E. W. (2013). Quack Medicine: A History of Combatting Health Fraud in Twentieth-Century America. Praeger/ABC-CLIO, LLC, Santa Barbara. CA.
Brighton, S. (2005). A Historical Archaeology of the Irish Proletarian Diaspora: The Material Manifestations of Irish Identity in America, 1850–1910. Doctoral dissertation, Boston University, Boston.
Chase, A. W. (1864). Dr. Chase’s Recipes; or Information for Everybody: An Invaluable Collection of about Eight Hundred Practical Recipes. A.W. Chase, Ann Arbor, MI.
Claus, E. P., Tyler, V. E., and Brady, L. R. (1970). Pharmacognosy, 6th ed. Lea and Febiger, Philadelphia.
Danna, S. R. (2015) Lydia Pinkham: The Face that Launched a Thousand Ads. Roman and Littlefield, Lanham, MD.
Duffy, J. (1978). “The changing image of the American physician.” In Leavitt, J. W. and Numbers, R. L. (eds.), Sickness and Health in America: Readings in the History of Medicine and Public Health. University of Wisconsin Press, Madison, pp. 131–137.
Düker, E-M., Kopanski, L., Jarry, H., and Wuttke, W. (1991). Effects of extracts from Cimicifuga racemose on Gonadotropin release in menopausal women and ovariectomized rats. Planta Medica 57(5):420–424.
Fike, R. E. (2006). The Bottle Book: A Comprehensive Guide to Historic, Embossed Medicine Bottles. Blackburn, Caldwell, NJ.
Foye, W. O. (1974). Principles of Medicinal Chemistry. Lea and Febiger, Philadelphia.
Gad, S. C. (2014). Proprionic acid. Encyclopedia of Toxicology, 3rd ed. Elsevier, Amsterdam.
Graham, P. R. (1973) Phthalate ester plasticizers-why and how they are used. Environmental Health Perspectives 3:3–12.
Gray, M. A. and Swope, K. K. (eds.) (2010). Deathways and Lifeways in the American Southwest: Tucson’s Historic Alameda-Stone Cemetery and the Transformation of a Remote Outpost into an Urban City. Volume 3: History and Archaeology of the Joint Courts Complex Postcemetery Period, 1875-2006. Statistical Research, Tucson, AZ.
Gray, M. A., Plumlee, R. S., Griffitts, J. L., White III, W. A., Morton, A. M., Lev-Tov, J. E., Ohman, D. M., Tiedens, S. L., Gregory, C. J., and Swope, K. K. (2010). Evolution of a Tucson Neighborhood, 1875-2006. In Deathways and Lifeways in the American Southwest: Tucson’s Historic Alameda-Stone Cemetery and the Transformation of a Remote Outpost into an Urban City. Volume 1: Context and Synthesis from the Joint Courts Complex Archaeological Project, Tucson, Arizona. Statistical Research, Tucson, AZ.
Griffenhagen, G. and Bogard, M. (1999). History of Drug Containers and their Labels. American Institute of the History of Pharmacy, Madison, WI.
Gurtler, J. B. and Mai, T. L. (2014). Traditional preservatives–organic acids. Encyclopedia of Food Microbiology (2nd ed.), Elsevier, Amsterdam.
Haines, M. R. (2001). The urban mortality transition in the United States, 1800–1940. Annales de Démographie Histoirque 1:33–64.
Harmon, K. (2003). A Period of Deceit: The Patent Medicine Business between 1865 and 1906. Senior thesis, University of North Carolina, Asheville, NC.
Hartshorne, H. (1881). The Household Cyclopedia of General Information. Thomas Kelly, New York.
Heilen, M. and Gray, M. A. (eds.) (2010). Deathways and Lifeways in the American Southwest Tucson’s Historic Alameda-Stone Cemetery and The Transformation of a Remote Outpost into an Urban City. Volume 1: Context and Synthesis from the Joint Courts Complex Archaeological Project, Tucson, Arizona. Statistical Research, Tucson, AZ.
Heilen, M., Hefner, J. T., and Keur, M. A. (eds.) (2010). Deathways and Lifeways in the American Southwest Tucson’s Historic Alameda-Stone Cemetery and The Transformation of a Remote Outpost into an Urban City: Volume 2 The History, Archaeology, and Skeletal Biology of the Alameda-Stone Cemetery. Statistical Research, Tucson, AZ.
Hodgson, B. (2001). In the Arms of Morpheus: The Tragic History of Laudanum, Morphine, and Patent Medicines. Firefly, Buffalo, NY.
Holbrook, S. H. (1959). The Golden Age of Quackery. Macmillan, New York.
Howson, J. E. (1993). The archaeology of 19th-century health and hygiene at the Sullivan Street Site, New York City. Northeast Historical Archaeology 22(10):137–160.
Hudson, R. P. (1978). Abraham Flexner in perspective: American Medical Education, 1865-1910. In Leavitt, J. W. and Numbers, R. L. (eds.), Sickness and Health in America: Readings in the History of Medicine and Public Health. University of Wisconsin Press, Madison, pp. 105–115.
Kuhar, M. J. and Pasternak, G. W. (1984). Analgesics: Neurochemical, Behavioral, and Clinical Perspectives. Raven Press, Internet Archive.
Laird, P. W. (1998). Advertising Progress: American Business and the Rise of Consumer Marketing. Johns Hopkins University Press, Baltimore, MD.
Linn, M. B. (2008). From Typhus to Tuberculosis and Fractures in Between: A Visceral Historical Archaeology of Irish Immigrant Life in New York City 1845-1870. Doctoral dissertation, Columbia University, New York.
Linn, M. B. (2014). Irish immigrant healing magic in nineteenth-century New York City. Historical Archaeology 48(3):144–165.
Lovekamp-Swan, T. and Davis, B. J. (2003). Mechanisms of phthalate ester toxicity in the female reproductive system. Environmental Health Perspectives 111(2):139–145.
Melosi, M. V. (2000). The Sanitary City: Urban Infrastructure in America from Colonial Times to the Present. Johns Hopkins University Press, Baltimore, MD.
Merck & Company. (1940). The Merck Manual of Therapeutics and Materia Medica. Merck & Company, Rahway, NJ.
Parascandola, J. (1990). The “preposterous provision”: the American Society for Pharmacology and Experimental Therapeutics’ ban on industrial pharmacologists, 1908–1941. In Liebenau, J., Higby, G. J., and Stroud, E. C. (eds.), Peddlers: Essays on the History of the Pharmaceutical Industry. American Institute of the History of Pharmacy, Madison, WI, pp. 29–49.
Pengelly, A. (2004). Constituents of Medicinal Plants: An Introduction to the Chemistry and Therapeutics of Herbal Medicine. Oxon, Wallingford.
Plowden, C. (2004). The ethnobotany of Copaíba (Copaifera) Oleoresin in the Amazon. Economic Botany 58(4):729–733.
Quebbeman, F. E. (1966). Medicine in Territorial Arizona. Arizona Historical Foundation, Phoenix.
Rosenberg, C. E. (1978). The practice of medicine in New York a century ago. In Leavitt, J. W. and Numbers, R. L. (eds.), Sickness and Health in America: Readings in the History of Medicine and Public Health. University of Wisconsin Press, Madison, pp. 55–75.
Ross, D. E. (2009). Material Life and Socio-Cultural Transformation among Asian Immigrants at a Frasier River Salmon Cannery. Doctoral dissertation, Simon Frasier University, Vancouver, BC.
Schablitsky, J. (2006). Genetic archaeology: the recovery and interpretation of nuclear DNA from a nineteenth-century hypodermic syringe. Historical Archaeology 40(3):8–19.
Scientific American. (1883). Naphthaline for agricultural and therapeutical uses. Scientific American 48(15):228.
Sheridan, T. E. (1986). Los Tucsonenses: The Mexican Community in Tucson, 1854-1941. University of Arizona Press, Tucson.
Sonnedecker, G., Cowen, D. L., and Higby, G. J. (2002). Drugstore Memories: American Pharmacists Recall Life behind the Counter, 18241933. American Institute of the History of Pharmacy, Madison, WI.
Spainhour, C. B. (2014). Phosphoric acid. Encyclopedia of Toxicology, 3rd ed. Elsevier, Amsterdam.
Spinner, M. A., Lustig, A. M., Warner, M., and von Wandruszka, R. (2011). Chemical identification of materials recovered in an archaeological excavations at Sandpoint, Idaho. Journal of the Idaho Academy of Science 47(1):29–53.
Stapp, D. C. (1990). The Historic Ethnography of a Chinese Mining Community in Idaho. Doctoral dissertation, University of Pennsylvania, Philadelphia.
Stillaguamish Valley Genealogical Society. (2003). Arlington Centennial Pictorial History, 1903–2003. Stillaguamish Valley Genealogical Society, Arlington, WA.
Swann, J. P. (1990). Universities, industry, and the rise of biomedical collaboration in America. In Liebenau, J., Higby, G. J., and Stroud, E. C. (eds.), Pill Peddlers: Essays on the History of the Pharmaceutical Industry. American Institute of the History of Pharmacy, Madison, WI, pp. 73–90.
Tansey, E. M. and Milligan, R. C. E. (1990). The early history of the Wellcome Research Laboratories, 1894–1914. In Liebenau, J., Higby, G. J., and Stroud, E. C. (eds.), Pill Peddlers: Essays on the History of the Pharmaceutical Industry, American Institute of the History of Pharmacy, Madison, WI, pp. 91–106.
Torbenson, B. C., Erlon, J., and Torbenson, M. S. (2000a). Lash’s Bitters: from the bathroom to the barroom. Pharmacy in History, 43(1):14–22.
Torbenson, M., Kelley, R. H., Erlen, J., Cropcho, L., Moraca, M., Beiler, B., Rao, K. N., and Virj, M. (2000b). Lash’s: a bitter medicine: biochemical analysis of an historical proprietary medicine. Historical Archaeology 34(2):56–64.
Tyler, V. E. (1995). Was Lydia Pinkham’s Vegetable Compound an effective remedy? Pharmacy in History 37(1):24–28.
Tyler, V. E., Bradley, L. R., and Robbers, J. E. (1988). Pharmacognosy. 9th ed. Lea and Febiger, Philadelphia.
Von Wandruszka, R. and Warner, M. (2018). A practical approach to the chemical analysis of historical materials. Historical Archaeology 52:741–752.
Von Wandruszka, R., Valentine, D., Warner, M., Kimball, V., Summer, T., Fink, A., and Hunter, S. (2016). Chemical analysis of pharmaceutical materials recovered from a historical dump in Nampa, Idaho. Journal of Northwest Anthropology 50(2):212–227.
Voss, B. L., von Wandruszka, R., Fink, A., Summer, T., Harman, S. E., Shapovalov, A., Kane, M. S., DeLoney, M., and Acebo, N. (2015). Stone drugs and calamine lotion: chemical analysis of residue in nineteenth-century glass bottles, Market Street Chinatown, San Jose, California. California Archaeology 7(1): 93–118.
Warner, M. (ed.) (2014). The Other Side of Sandpoint: Early History and Archaeology beside the Track: The Sandpoint Archaeology Project, 2006–2013. Volume 2: Material Culutre of Everyday Life. SWCA Environmental Consultants, Portland, OR.
Weaver, R. (ed.) (2014). The Other Side of Sandpoint: Early History and Archaeology beside the Track: The Sandpoint Archaeology Project, 2006—2013. Volume 1: Sandpoint Stories. SWCA Environmental Consultants, Portland, OR.
Wegars, P. S. (1991). The History and Archaeology of the Chinese in Northern Idaho, 1880 through 1910. Doctoral dissertation, University of Idaho, Moscow.
Wernke, M. J. (2014). Glycerol. Encyclopedia of Toxicology, Volume 2. Elsevier, Amsterdam, pp. 754–756.
White, III, W. A. (2007). Try Dr. Davidson’s Headache Powders: people and medicine in 19th century Tacoma, Washington. Paper presented at the 2007 Society for Historical Archaeology Conference, Williamsburg, VA.
White, III, W. A. (2012). The legacy of industrialization: archaeology at contaminated sites with potentially hazardous artifacts. SHA Newsletter, Spring.
White, III, W. A., Boswell, S. A., and Miss, C. J. (2008a). Results of Data Recovery and Site Evaluation Excavations at the Japanese Gulch Site, 45SN398, Mukilteo, Washington. Northwest Archaeological Associates, Inc., Seattle.
White, III, W. A., Valentino, A. B., and Smith, R. (2008b). Data Recovery at 45SN409, the Teager/Weimer Site, Arlington, Snohomish County, Washington. Report for the City of Arlington, Washington. Northwest Archaeological Associates, Inc., Seattle.
Whitten, D. (2019). Glass factory marks on bottles. < http://www.glassbottlemarks.com/bottlemarks/ > accessed December, 2019.
Young, J. H. (1961). The Toadstool Millionaires: A Social History of Patent Medicines in America before Federal Regulation. Princeton University Press, Princeton, NJ.
Acknowledgments
A number of individuals helped make this research possible. I also owe a debt of gratitude to Roger Anyon of the Pima County Cultural Resources and Historic Preservation Office for allowing me to publish these interesting results. The Alameda-Stone Cemetery Site archaeological excavation project was funded in its entirety by Pima County contract number 07-73-S-138479-0806. I would like to thank Dr. Arpad Somogyi and the staff at the Mass Spectrometry Facility of the Department of Chemistry at the University of Arizona for their work processing the contents of these bottles and trying to help me figure out what compounds were in them. I would like to thank Marlesa Gray and Teresita Majewski for enabling me to conduct mass spectrometry tests on these medicines. I would also like to thank Christian Miss and Lorelea Hudson for their support with the earlier mass spectrometry work conducted in Washington State that formed the foundation of this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
White, W.A. Just What the Doctor Ordered: Biochemical Analysis of Historical Medicines from Downtown Tucson, Arizona. Int J Histor Archaeol 25, 515–543 (2021). https://doi.org/10.1007/s10761-020-00571-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10761-020-00571-7