Abstract
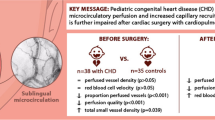
A prospective, observational single-center study was carried out. Pediatric patients undergoing congenital heart defect surgery were evaluated before, during, and after surgery. At each time point, sublingual microcirculation and clinical parameters were assessed, along with analytical variables. Twenty-four patients were included. All microcirculatory parameters worsened during cardiopulmonary bypass and returned to baseline values after surgery (p ≤ 0.001). In the intraoperative evaluation, body temperature correlated with perfused small vessel density (p = 0.014), proportion of perfused small vessels (p < 0.001), small vessel microvascular flow index (p = 0.003), and small vessel heterogeneity index (p < 0.002). Patients with cyanotic disease exhibited higher small vessel density (p < 0.008) and higher density of perfused small vessels (p < 0.022) at baseline, and a lower microvascular flow index (p = 0.022) and higher heterogeneity (p = 0.026) in the intraoperative phase. Children with congenital heart disease exhibited decreased vascular density and microvascular blood flow and increased heterogeneity during cardiopulmonary bypass. All these parameters returned to baseline values after surgery.
Graphical abstract




Similar content being viewed by others
Abbreviations
- CHD:
-
Congenital heart defects
- CI95%:
-
95% confidence interval
- DB:
-
De Backer score
- FiO2 :
-
Fraction of inspired oxygen
- HI:
-
Heterogeneity index
- IQR:
-
Interquartile range
- MFI:
-
Microcirculatory flow index
- NIRS:
-
Near infrared photospectrometry
- PEEP:
-
Positive end expiratory pressure
- PICU:
-
Pediatric intensive care unit
- PIP:
-
Peak inspiratory pressure
- PPV:
-
Proportion of perfused vessels
- PVD:
-
Perfused vessel density
- SDF:
-
Sidestream dark-field imaging
- SV:
-
Small vessels
- TVD:
-
Total vessel density
- VIS:
-
Vasoactive inotropic score
References
Vellinga, N. A. R., Boerma, E. C., Koopmans, M., Donati, A., Dubin, A., Shapiro, N. I., et al. (2017). Mildly elevated lactate levels are associated with microcirculatory flow abnormalities and increased mortality: A microSOAP post hoc analysis. Critical Care, 21(1), 255. https://doi.org/10.1186/s13054-017-1842-7.
Trzeciak, S., Dellinger, R. P., Parrillo, J. E., Guglielmi, M., Bajaj, J., Abate, N. L., et al. (2007). Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: Relationship to hemodynamics, oxygen transport, and survival. Annals of Emergency Medicine, 49(1), 88–98.e2. https://doi.org/10.1016/j.annemergmed.2006.08.021.
De Backer, D., Donadello, K., Sakr, Y., Ospina-Tascon, G., Salgado, D., Scolletta, S., & Vincent, J.-L. (2013). Microcirculatory alterations in patients with severe sepsis: Impact of time of assessment and relationship with outcome. Critical Care Medicine, 41(3), 791–799. https://doi.org/10.1097/CCM.0b013e3182742e8b.
Bauer, A., Kofler, S., Thiel, M., Eifert, S., & Christ, F. (2007). Monitoring of the sublingual microcirculation in cardiac surgery using orthogonal polarization spectral imaging: preliminary results. Anesthesiology, 107(6), 939–945. https://doi.org/10.1097/01.anes.0000291442.69337.c9.
Maier, S., Hasibeder, W. R., Hengl, C., Pajk, W., Schwarz, B., Margreiter, J., et al. (2009). Effects of phenylephrine on the sublingual microcirculation during cardiopulmonary bypass. British Journal of Anaesthesia, 102(4), 485–491. https://doi.org/10.1093/bja/aep018.
De Backer, D., Dubois, M.-J., Schmartz, D., Koch, M., Ducart, A., Barvais, L., & Vincent, J.-L. (2009). Microcirculatory alterations in cardiac surgery: Effects of cardiopulmonary bypass and anesthesia. The Annals of Thoracic Surgery, 88(5), 1396–1403. https://doi.org/10.1016/j.athoracsur.2009.07.002.
Elbers, P. W. G., Wijbenga, J., Solinger, F., Yilmaz, A., van Iterson, M., van Dongen, E. P. A., & Ince, C. (2011). Direct observation of the human microcirculation during cardiopulmonary bypass: Effects of pulsatile perfusion. Journal of Cardiothoracic and Vascular Anesthesia, 25(2), 250–255. https://doi.org/10.1053/j.jvca.2010.06.014.
Yuruk, K., Almac, E., Bezemer, R., Goedhart, P., de Mol, B., & Ince, C. (2011). Blood transfusions recruit the microcirculation during cardiac surgery. Transfusion, 51(5), 961–967. https://doi.org/10.1111/j.1537-2995.2010.02971.x.
O’Neil, M. P., Alie, R., Guo, L. R., Myers, M.-L., Murkin, J. M., & Ellis, C. G. (2018). Microvascular responsiveness to pulsatile and nonpulsatile flow during cardiopulmonary bypass. The Annals of Thoracic Surgery, 105(6), 1745–1753. https://doi.org/10.1016/j.athoracsur.2018.01.007.
Koning, N. J., Vonk, A. B. A., Vink, H., & Boer, C. (2016). Side-by-side alterations in glycocalyx thickness and perfused microvascular density during acute microcirculatory alterations in cardiac surgery. Microcirculation, 23(1), 69–74. https://doi.org/10.1111/micc.12260.
Dekker, N. A. M., Veerhoek, D., Koning, N. J., van Leeuwen, A. L. I., Elbers, P. W. G., van den Brom, C. E., et al. (2019). Postoperative microcirculatory perfusion and endothelial glycocalyx shedding following cardiac surgery with cardiopulmonary bypass. Anaesthesia, 74(5), 609–618. https://doi.org/10.1111/anae.14577.
den Uil, C. A., Lagrand, W. K., Spronk, P. E., van Domburg, R. T., Hofland, J., Lüthen, C., et al. (2008). Impaired sublingual microvascular perfusion during surgery with cardiopulmonary bypass: A pilot study. The Journal of Thoracic and Cardiovascular Surgery, 136(1), 129–134. https://doi.org/10.1016/j.jtcvs.2007.10.046.
Nussbaum, C., Haberer, A., Tiefenthaller, A., Januszewska, K., Chappell, D., Brettner, F., et al. (2015). Perturbation of the microvascular glycocalyx and perfusion in infants after cardiopulmonary bypass. The Journal of Thoracic and Cardiovascular Surgery, 150(6), 1474–1481.e1. https://doi.org/10.1016/j.jtcvs.2015.08.050.
Scolletta, S., Marianello, D., Isgrò, G., Dapoto, A., Terranova, V., Franchi, F., et al. (2016). Microcirculatory changes in children undergoing cardiac surgery: A prospective observational study. British Journal of Anaesthesia, 117(2), 206–213. https://doi.org/10.1093/bja/aew187.
Ugenti, V., Romano, A. C., & Tibirica, E. (2018). Microvascular endothelial dysfunction during cardiopulmonary bypass in surgery for correction of cyanotic and acyanotic congenital heart disease. Microvascular Research, 120, 55–58. https://doi.org/10.1016/j.mvr.2018.06.004.
De Backer, D., Hollenberg, S., Boerma, C., Goedhart, P., Büchele, G., Ospina-Tascon, G., et al. (2007). How to evaluate the microcirculation: Report of a round table conference. Critical Care, 11(5), R101. https://doi.org/10.1186/cc6118.
Ince, C., Boerma, E. C., Cecconi, M., De Backer, D., Shapiro, N. I., Duranteau, J., et al. (2018). Second consensus on the assessment of sublingual microcirculation in critically ill patients: Results from a task force of the European Society of Intensive Care Medicine. Intensive Care Medicine, 44(3), 281–299. https://doi.org/10.1007/s00134-018-5070-7.
Gaies, M. G., Gurney, J. G., Yen, A. H., Napoli, M. L., Gajarski, R. J., Ohye, R. G., et al. (2010). Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatric Critical Care Medicine, 11(2), 234–238. https://doi.org/10.1097/PCC.0b013e3181b806fc.
Vellinga, N. A. R., Boerma, E. C., Koopmans, M., Donati, A., Dubin, A., Shapiro, N. I., et al. (2015). International study on microcirculatory shock occurrence in acutely ill patients. Critical Care Medicine, 43(1), 48–56. https://doi.org/10.1097/CCM.0000000000000553.
den Os, M. M., van den Brom, C. E., van Leeuwen, A. L. I., & Dekker, N. A. M. (2020). Microcirculatory perfusion disturbances following cardiopulmonary bypass: A systematic review. Critical Care, 24(1), 218. https://doi.org/10.1186/s13054-020-02948-w.
De Blasi, R. A., Palmisani, S., Boezi, M., Arcioni, R., Collini, S., Troisi, F., & Pinto, G. (2008). Effects of remifentanil-based general anaesthesia with propofol or sevoflurane on muscle microcirculation as assessed by near-infrared spectroscopy. British Journal of Anaesthesia, 101(2), 171–177. https://doi.org/10.1093/bja/aen136.
Koch, M., De Backer, D., Vincent, J. L., Barvais, L., Hennart, D., & Schmartz, D. (2008). Effects of propofol on human microcirculation. British Journal of Anaesthesia, 101(4), 473–478. https://doi.org/10.1093/bja/aen210.
Liu, X., Zhang, K., Wang, W., Xie, G., Cheng, B., Wang, Y., et al. (2016). Dexmedetomidine versus propofol sedation improves sublingual microcirculation after cardiac surgery: A randomized controlled trial. Journal of Cardiothoracic and Vascular Anesthesia, 30(6), 1509–1515. https://doi.org/10.1053/j.jvca.2016.05.038.
Riedijk, M. A., & Milstein, D. M. J. (2018). Imaging sublingual microcirculatory perfusion in pediatric patients receiving procedural sedation with propofol: A pilot study. Microcirculation, e12484. https://doi.org/10.1111/micc.12484
Özarslan, N. G., Ayhan, B., Kanbak, M., Çelebioğlu, B., Demircin, M., Ince, C., & Aypar, Ü. (2012). Comparison of the effects of sevoflurane, isoflurane, and desflurane on microcirculation in coronary artery bypass graft surgery. Journal of Cardiothoracic and Vascular Anesthesia, 26(5), 791–798. https://doi.org/10.1053/j.jvca.2012.03.019.
Maar, S. P. (2008). Searching for the Holy Grail: A review of markers of tissue perfusion in pediatric critical care. Pediatric Emergency Care, 24(12), 883–887. https://doi.org/10.1097/PEC.0b013e31819112b7.
Englehart, M. S., & Schreiber, M. A. (2006). Measurement of acid-base resuscitation endpoints: Lactate, base deficit, bicarbonate or what? Current Opinion in Critical Care, 12(6), 569–574. https://doi.org/10.1097/MCC.0b013e328010ba4f.
Holley, A., Lukin, W., Paratz, J., Hawkins, T., Boots, R., & Lipman, J. (2012). Review article: Part two: Goal-directed resuscitation--Which goals? Perfusion targets. Emergency Medicine Australasia, 24(2), 127–135. https://doi.org/10.1111/j.1742-6723.2011.01515.x.
González, R., Urbano, J., Solana, M. J., Hervías, M., Pita, A., Pérez, R., et al. (2019). Microcirculatory differences in children with congenital heart disease according to cyanosis and age. Frontiers in Pediatrics, 7, 264. https://doi.org/10.3389/fped.2019.00264.
Boerma, E. C., & Ince, C. (2010). The role of vasoactive agents in the resuscitation of microvascular perfusion and tissue oxygenation in critically ill patients. Intensive Care Medicine, 36(12), 2004–2018. https://doi.org/10.1007/s00134-010-1970-x.
Buijs, E. A. B., Verboom, E. M., Top, A. P. C., Andrinopoulou, E.-R., Buysse, C. M. P., Ince, C., & Tibboel, D. (2014). Early microcirculatory impairment during therapeutic hypothermia is associated with poor outcome in post-cardiac arrest children: A prospective observational cohort study. Resuscitation, 85(3), 397–404. https://doi.org/10.1016/j.resuscitation.2013.10.024.
Ergenekon, E., Hirfanoğlu, I., Beken, S., Turan, O., Kulali, F., Koç, E., & Gücüyener, K. (2013). Peripheral microcirculation is affected during therapeutic hypothermia in newborns. Archives of Disease in Childhood. Fetal and Neonatal Edition, 98(2), F155–F157. https://doi.org/10.1136/archdischild-2012-301647.
González, R., Urbano, J., López, J., Solana, M. J., Botrán, M., García, A., et al. (2016). Microcirculatory alterations during haemorrhagic shock and after resuscitation in a paediatric animal model. Injury, 47(2), 335–341. https://doi.org/10.1016/j.injury.2015.10.075.
González, R., López, J., Urbano, J., Solana, M. J., Fernández, S. N., Santiago, M. J., & López-Herce, J. (2017). Evaluation of sublingual microcirculation in a paediatric intensive care unit: Prospective observational study about its feasibility and utility. BMC Pediatrics, 17(1), 75. https://doi.org/10.1186/s12887-017-0837-5.
Acknowledgements
The authors would like to acknowledge the contribution to the study of all members of the infant heart area of Gregorio Marañón General University Hospital. The authors would like to specially acknowledge the patients and their families who decided to collaborate with our study.
Funding
This study was partially funded by the Mutua Madrileña Foundation (grant FMM 14/02), by the Spanish Society of Paediatric Intensive Care (Francisco Ruza’s grant 2017), and by the Carlos III Health Institute Subdirectorate General for Research Assessment and Promotion, and the European Regional Development Fund (ERDF) (grant PI17/01319).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human Subjects/Informed Consent Statement
The study was approved by Gregorio Marañón General University Hospital Institutional Review Board. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients or their legal representatives for being included in the study
Conflict of Interest
The authors declare no competing interests.
Additional information
Associate Editor Junjie Xiao oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
González Cortés, R., Urbano Villaescusa, J., Solana García, M.J. et al. Microcirculatory Changes in Pediatric Patients During Congenital Heart Defect Corrective Surgery. J. of Cardiovasc. Trans. Res. 14, 1173–1185 (2021). https://doi.org/10.1007/s12265-021-10132-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-021-10132-w