Abstract
Background
Oral anticoagulation (OAC) is recommended to reduce the risk of stroke or systemic thromboembolism (TE) in atrial fibrillation (AF). In this study, we applied novel joint latent class mixed models to identify heterogeneous patterns of trajectories of OAC use and determined how these trajectories are associated with risks of thromboembolic outcomes.
Methods and Results
We used 2013–2016 claims data from a 5% random sample of Medicare beneficiaries, obtained from the Centers for Medicare and Medicaid Services. Our study sample included 16,399 patients newly diagnosed with AF in 2014–2015 who were followed for 12 months after the first AF diagnosis and filled at least one OAC prescription in this time period. OAC use was defined as the number of days covered with OACs every 30-day interval after the first AF diagnosis. We used a joint latent class mixed model to simultaneously evaluate the longitudinal patterns of OAC use and time to stroke or TE, while adjusting for age, race, CHAD2S2-VASc score and HAS-BLED score.
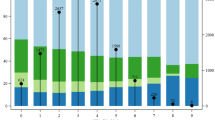
Five classes of OAC use patterns were identified: late users (17.8%); late initiators (12.5%); early discontinuers (18.6%); late discontinuers (15.4%); and continuous users (35.6%). Compared with continuous users, the risk of stroke or TE was higher for participants in the late initiators (hazard ratio [HR] 1.73, 95% confidence interval [CI] 1.49–2.01) and late discontinuers (HR 1.23, 95% CI 1.04–1.45) classes.
Conclusion
Late initiators and late discontinuers had a higher risk of stroke or TE than continuous users. Early initiation and continuous OAC use is important in preventing stroke and TE among patients diagnosed with AF.



Similar content being viewed by others
References
Freedman B, Potpara TS, Lip GYH. Stroke prevention in atrial fibrillation. Lancet. 2016;388(10046):806–17.
Lip GYH, Banerjee A, Boriani G, Chiang CE, Fargo R, Freedman B, et al. Antithrombotic therapy for atrial fibrillation: CHEST Guideline and Expert Panel Report. Chest. 2018;154(5):1121–201.
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019;140(2):e125–51.
Hernandez I, He M, Brooks MM, Saba S, Gellad WF. Adherence to anticoagulation and risk of stroke among medicare beneficiaries newly diagnosed with atrial fibrillation. Am J Cardiovasc Drugs. 2020;20(2):199–207.
Hernandez I, He M, Chen N, Brooks MM, Saba S, Gellad WF. Trajectories of oral anticoagulation adherence among medicare beneficiaries newly diagnosed with atrial fibrillation. J Am Heart Assoc. 2019;8(12):e011427.
Hernandez I, Zhang Y, Saba S. Comparison of the effectiveness and safety of apixaban, dabigatran, rivaroxaban, and warfarin in newly diagnosed atrial fibrillation. Am J Cardiol. 2017;120(10):1813–9.
Hart RG, Pearce LA, Aguilar MI. Meta analysis antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857–67.
Clemens A, Haertter S, Friedman J, Brueckmann M, Stangier J, van Ryn J, et al. Twice daily dosing of dabigatran for stroke prevention in atrial fibrillation: a pharmacokinetic justification. Curr Med Res Opin. 2012;28(2):195–201.
Clemens A, Noack H, Brueckmann M, Lip GY. Twice- or once-daily dosing of novel oral anticoagulants for stroke prevention: a fixed-effects meta-analysis with predefined heterogeneity quality criteria. PLoS ONE. 2014;9(6):e99276.
Lang K, Bozkaya D, Patel AA, Macomson B, Nelson W, Owens G, et al. Anticoagulant use for the prevention of stroke in patients with atrial fibrillation: findings from a multi-payer analysis. BMC Health Serv Res. 2014;14(1):329.
CMS Chronic Conditions Data Warehouse (CCW). CCW condition algorithms. 2019. https://www2.ccwdata.org/web/guest/condition-categories. Accessed 8 Apr 2021.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1-76.
Sokal RR, Rohlf FJ. Statistical tables. 3rd ed. New York, NY, USA: MacMillan; 1995.
Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350–9.
Duncan O, Duncan B. A methodological analysis of segregation indexes. Am Sociol Rev. 1955;20(2):210–7.
Massey D, Denton N. The dimensions of residential segregation. Soc Forces. 1988;67(2):281–315.
Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–72.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100.
Proust-Lima C, Séne M, Taylor JMG, Jacqmin-Gadda H. Joint latent class models for longitudinal and time-to-event data: a review. Stat Methods Med Res. 2012;23(1):74–90.
Proust C, Jacqmin-Gadda H. Estimation of linear mixed models with a mixture of distribution for the random effects. Comput Methods Programs Biomed. 2005;78(2):165–73.
Proust-Lima C, Philipps V, Liquet B. Estimation of extended mixed models using latent classes and latent processes: the R Package lcmm. J Stat Softw. 2017. https://doi.org/10.18637/jss.v078.i02
Chen N, Brooks MM, Hernandez I. Latent classes of adherence to oral anticoagulation therapy among patients with a new diagnosis of atrial fibrillation. JAMA Netw Open. 2020;3(2):e1921357.
Yao X, Abraham NS, Alexander GC, Crown W, Montori VM, Sangaralingham LR, et al. Effect of adherence to oral anticoagulants on risk of stroke and major bleeding among patients with atrial fibrillation. J Am Heart Assoc. 2016;5(2):e003074.
Borne RT, O’Donnell C, Turakhia MP, Varosy PD, Jackevicius CA, Marzec LN, et al. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: findings from the veterans health administration. BMC Cardiovasc Disord. 2017;17(1):236.
Beunckens C, Molenberghs G, Verbeke G, Mallinckrodt C. A latent-class mixture model for incomplete longitudinal Gaussian data. Biometrics. 2008;64(1):96–105.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the National Institutes of Health (Grant Number UL1TR001857), and the National Heart, Lung and Blood Institute (Grant Number K01HL142847).
Conflict of interest
Inmaculada Hernandez has received consulting fees from Bristol Myers Squibb and Pfizer. Nemin Chen, Nico Gabriel, and Maria M. Brooks have no conflicts of interest to declare.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The authors are unable to share the data since the data were obtained under a data user agreement that does not allow data sharing.
Code availability
Code can be made available upon request to the corresponding author.
Author contributions
IH and NC designed the study; NG undertook the statistical analysis; NC wrote the manuscript; and IH, NG, and MMB undertook critical revision of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, N., Gabriel, N., Brooks, M.M. et al. Joint Latent Class Analysis of Oral Anticoagulation Use and Risk of Stroke or Systemic Thromboembolism in Patients with Atrial Fibrillation. Am J Cardiovasc Drugs 21, 573–580 (2021). https://doi.org/10.1007/s40256-021-00476-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-021-00476-8