Abstract
At least 1 in 10 patients develop intraoperative pressure ulcers (PUs). The specific rigid (bio)mechanical constraints that apply in the operation room (OR) and which are unique to this clinical environment, including the inability to periodically reposition patients during surgery and the need to use a ‘stable’ support surface with relatively stiff padding materials lead to soft tissue exposure to extreme conditions of sustained tissue deformations and stress concentrations due to bodyweight forces. Accordingly, the risk of intraoperative PUs, which are triggered and driven by a sustained cell and tissue deformation/stress exposure, is especially high on the operating table (OT). Importantly, the basic OT and OT pad designs are simple and have changed very little over at least a century. The available OT pads, in particular, did not evolve despite the well-known and documented risk for PUs among surgical patients. This article reviews the relevant biomechanical studies published by the author and his research group with respect to the extents of tissue deformations expected on the OT at the body regions which are most susceptible to intraoperative PUs, namely the sacral region and the posterior aspects of the heels. These are the body sites which transfer considerable bodyweight forces in a supine position and contain relatively ‘sharp’ bony prominences compressing relatively thin soft tissue structures, as evident by the magnetic resonance imaging (MRI) studies conducted by the author and his team, as reviewed here. The results reported in this article further highlight the roles of OT pad and positioner materials in reducing localized tissue deformations and thereby, in lowering the risk of intraoperative PUs.


Similar content being viewed by others
References
Aronovitch, S.A.: Intraoperatively acquired pressure ulcers: are there common risk factors? Ostomy/wound Manage., 53, 57–69 (2007)
Call, E., Tanner, L., Cheney, A., Rappl, L., Santamaria, N., Gefen, A., Oberg, C.: Results of laboratory testing for immersion, envelopment, and horizontal stiffness on turn and position devices to manage pressure injury. Adv. Skin Wound Care 33(10S Suppl 1), S11–S22 (2020 Oct)
Ceelen, K.K., Stekelenburg, A., Loerakker, S., Strijkers, G.J., Bader, D.L., Nicolay, K., Baaijens, F.P., Oomens, C.W.: Compression-induced damage and internal tissue strains are related. J. Biomech. 41(16), 3399–3404 (2008 Dec 5).
Chen, H.L., Jiang, A.G., Zhu, B., Cai, J.Y., Song, Y.P.: The risk factors of postoperative pressure ulcer after liver resection with long surgical duration: a retrospective study. Wounds 31(9), 242–245 (2019 Sep)
De Backer, D., Foulon, P.: Minimizing catecholamines and optimizing perfusion. J. Crit. Care 23(Suppl 1), 149 (2019 Jun 14)
de Oliveira K.F., Nascimento, K.G., Nicolussi, A.C., Chavaglia, S.S.R., de Araújo, C.A., Barbosa, M.H: Support surfaces in the prevention of pressure ulcers in surgical patients: an integrative review. Int. J. Nurs. Pract. 23(4) (2017 Aug). https://doi.org/10.1111/ijn.12553
Engels, D., Austin, M., McNichol, L., Fencl, J., Gupta, S., Kazi, H.: Pressure ulcers: factors contributing to their development in the OR. AORN J. 103(3), 271–281 (2016)
Fife, C.E., Gkotsoulias, E.: On the origin of intraoperative pressure injury: an angiosomal theory of pressure injury formation. Adv. Wound Care (New Rochelle) 8(11), 580–584 (2019 Nov 1)
Fred, C., Ford, S., Wagner, D., Vanbrackle, L.: Intraoperatively acquired pressure ulcers and perioperative normothermia: a look at relationships. AORN J. 96(3), 251–260 (2012 Sep)
Galivanche, A.R., Kebaish, K.J., Adrados, M., Ottesen, T.D., Varthi, A.G., Rubin, L.E., Grauer, J.N.: Postoperative pressure ulcers after geriatric hip fracture surgery are predicted by defined preoperative comorbidities and postoperative complications. J. Am. Acad. Orthop. Surg. 28(8), 342–351 (2020 Apr 15).
Gefen, A., van Nierop, B., Bader, D.L., Oomens, C.W.: Strain-time cell-death threshold for skeletal muscle in a tissue-engineered model system for deep tissue injury. J. Biomech. 41(9), 2003–2012 (2008)
Gefen, A., Brienza, D., Edsberg, L., Milton, W., Murphy, C., Oomens, C.W.J., Perry, L., Sari, Y.: The etiology of pressure injuries. In: Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel (NPIAP) and the Pan Pacific Pressure Injury Alliance (PPPIA), third edn. (2019)
Gefen, A.: How medical engineering has changed our understanding of chronic wounds and future prospects. Med. Eng. Phys. 72, 13–18 (2019 Oct)
Gefen, A.: Minimising the risk for pressure ulcers in the operating room using a specialised low-profile alternating pressure overlay. Wounds Int. 11(2), 10–16 (2020)
Gefen, A., Creehan, S., Black, J.: Critical biomechanical and clinical insights concerning tissue protection when positioning patients in the operating room: a scoping review. Int. Wound J. 17(5), 1405–1423 (2020 Oct)
Haex, B.: Back and Bed: Ergonomic Aspects of Sleeping, first edn. CRC Press, Boca Raton (2004)
Hayes, R.M., Spear, M.E., Lee, S.I., Krauser Lupear, B.E., Benoit, R.A., Valerio, R., Dmochowski, R.R.: Relationship between time in the operating room and incident pressure ulcers: a matched case-control study. Am. J. Med. Qual. 30(6), 591–597 (2015 Nov-Dec)
Katzengold, R., Gefen, A.: Modelling an adult human head on a donut-shaped gel head support for pressure ulcer prevention. Int. Wound J. 16(6), 1398–1407 (2019 Dec)
Karg, P., Ranganathan, V.K., Churilla, M., Brienza, D.: Sacral skin blood flow response to alternating pressure operating room overlay. J. Tissue Viab. 28(2), 75–80 (2019)
Linder-Ganz, E., Engelberg, S., Scheinowitz, M., Gefen, A.: Pressure-time cell death threshold for albino rat skeletal muscles as related to pressure sore biomechanics. J. Biomech. 39(14), 2725–2732 (2006)
Linder-Ganz, E., Shabshin, N., Itzchak, Y., Gefen, A.: Assessment of mechanical conditions in sub-dermal tissues during sitting: a combined experimental-MRI and finite element approach. J. Biomech. 40(7), 1443–1454 (2007)
Linder-Ganz, E., Shabshin, N., Itzchak, Y., Yizhar, Z., Siev-Ner I., Gefen, A.: Strains and stresses in sub-dermal tissues of the buttocks are greater in paraplegics than in healthy during sitting. J. Biomech. 41(3), 567–580 (2008)
Lustig, M., Wiggermann, N., How, G.A.: Patient migration in bed affects the sacral soft tissue loading and thereby the risk for a hospital-acquired pressure injury. Int. Wound J. 17(3), 631–640 (2020 Jun)
Lustig, A., Margi, R., Orlov, A., Orlova, D., Azaria, L., Gefen, A.: The mechanobiology theory of the development of medical device-related pressure ulcers revealed through a cell-scale computational modeling framework. Biomech. Model. Mechanobiol. 19, 1–10 (2021 Feb)
Oliveira, K.F., Pires, P.D.S., De-Mattia, A.L., et al.: Influence of support surfaces on the distribution of body interface pressure in surgical positioning. Rev. Latino-Am. Enfermagem 26, e3083 (2018)
Palevski, A., Glaich, I., Portnoy, S., Linder-Ganz, E., Gefen, A.: Stress relaxation of porcine gluteus muscle subjected to sudden transverse deformation as related to pressure sore modeling. J. Biomech. Eng. 128(5), 782–787 (2006 Oct)
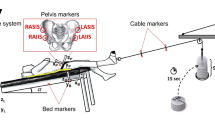
Peko Cohen, L., Levy, A., Shabshin, N., Neeman, Z., Gefen, A.: Sacral soft tissue deformations when using a prophylactic multilayer dressing and positioning system: MRI studies. J. Wound Ostomy Cont. Nurs. 45(5), 432–437 (2018 Sep/Oct).
Peters, M.G., Berger, A.C., Schwartz, G.F., Yeo, C.J., Cowan, S.W.: John Chalmers DaCosta (1863–1933): restoration of the old operating table. Am Surg. 79(3), 232–234 (2013)
Petty, W.C.: The operating table: a historical perspective. Todays Surg Nurse 18(4), 30–34 (1996)
Price, M.C., Whitney, J.D., King, C.A., Doughty, D.: Development of a risk assessment tool for intraoperative pressure ulcers. J. Wound Ostomy Cont. Nurs. 32(1), 19–30 (2005 Jan-Feb)
Pokorny, M., Koldjeski, D., Swanson, M.: Skin care intervention for patients having cardiac surgery. American journal of critical care: an official publication. AACN Crit. Care Nurs. 12, 535–544 (2003)
Power, H.: Patient positioning outcomes for women undergoing gynaecological surgeries. Can. Oper. Room Nurs. J. 20(3), 7–10 (2002 Sep). 27–30
Rogan, J.: Pressure ulcer risk during the perioperative period focusing on surgery duration and hypothermia. Wounds UK 3(4), 66–74 (2007)
Schoonhoven, L., Defloor, T., van der Tweel, I., Buskens, E., Grypdonck, M.H.: Risk indicators for pressure ulcers during surgery. Appl. Nurs. Res. 15(3), 163–173 (2002)
Scott, E.M., Leaper, D.J., Clark, M., Kelly, P.J.: Effects of warming therapy on pressure ulcers - a randomized trial. AORN J. 73(5), 921–927 (2001 May). 929-33, 936-8
Scott, S.M.: Progress and challenges in perioperative pressure ulcer prevention. J. Wound Ostomy Cont. Nurs. 42(5), 480–485 (2015 Sep-Oct)
Scott, S.M.: Perioperative pressure injuries: protocols and evidence-based programs for reducing risk. Patient Safety Qual. Healthcare 13(4), 21–28 (2016 July-Aug).
Shabshin, N., Zoizner, G., Herman, A., Ougortsin, V., Gefen, A.: Use of weight-bearing MRI for evaluating wheelchair cushions based on internal soft-tissue deformations under ischial tuberosities. J. Rehabil. Res. Dev. 47(1), 31–42 (2010)
Solis, L.R., Liggins, A.B., Seres, P., Uwiera, R.R., Poppe, N.R., Pehowich, E., Thompson, R.B., Mushahwar, V.K.: Distribution of internal strains around bony prominences in pigs. Ann. Biomed. Eng. 40(8), 1721–1739 (2012 Aug)
Sopher, R., Nixon, J., Gorecki, C., Gefen, A.: Exposure to internal muscle tissue loads under the ischial tuberosities during sitting is elevated at abnormally high or low body mass indices. J. Biomech. 43(2), 280–286 (2010, Jan 19)
Tenenbaum, S., Shabshin, N., Levy, A., Herman, A., Gefen, A.: Effects of foot posture and heel padding devices on soft tissue deformations under the heel in supine position in males: MRI studies. J. Rehabil. Res. Dev. 50(8), 1149–1156 (2013)
Toussaint, R.J., Abousayed, M.M., Kwon, J.Y.: Preventing falls in the operating room: a technique tip for safely tilting the operating table. Foot Ankle Spec. 6(5), 372–375 (2013 Oct)
Yarnitzky, G., Yizhar, Z., Gefen, A.: Real-time subject-specific monitoring of internal deformations and stresses in the soft tissues of the foot: a new approach in gait analysis. J. Biomech. 39(14), 2673–2689 (2006)
Yoshimura, M., Nakagami, G., Iizaka, S., Yoshida, M., Uehata, Y., Kohno, M., Kasuya, Y., Mae, T., Yamasaki, T., Sanada, H.: Microclimate is an independent risk factor for the development of intraoperatively acquired pressure ulcers in the park-bench position: a prospective observational study. Wound Repair Regen. 23(6), 939–947 (2015 Nov-Dec)
Yoshimura, M., Ohura, N., Santamaria, N., Watanabe, Y., Akizuki, T., Gefen, A.: High body mass index is a strong predictor of intraoperative acquired pressure injury in spinal surgery patients when prophylactic film dressings are applied: a retrospective analysis prior to the BOSS Trial. Int. Wound J. 17(3), 660–669 (2020). https://doi.org/10.1111/iwj.13287
Zeevi, T., Levy, A., Brauner, N., Gefen, A.: Effects of ambient conditions on the risk of pressure injuries in bedridden patients-multi-physics modelling of microclimate. Int. Wound J. 15(3), 402–416 (2018)
Acknowledgements
This work was supported by the Israeli Ministry of Science & Technology (Medical Devices Program Grant no. 3-17421, awarded to Professor Amit Gefen in 2020).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Invited contribution for the Special Volume to mark the 60th birthday of Professor Gerhard Holzapfel
Rights and permissions
About this article
Cite this article
Gefen, A. Gravity Is Our Best Friend Yet Can Also Be Our Worst Enemy: Tissue Deformations and Pressure Ulcer Risk on the Operating Table. J Elast 145, 153–162 (2021). https://doi.org/10.1007/s10659-021-09824-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10659-021-09824-w