Abstract
Frontotemporal dementia is a heterogeneous spectrum of neurodegenerative disorders. The neuropathological inclusions are tau proteins, TAR DNA binding protein 43 kDa-TDP-43, or fused in sarcoma-ubiquitinated inclusions. Genetically, several autosomal mutations account for the heritability of the disorder. Phenotypically, frontotemporal dementia can present with a behavioral variant or a language variant called primary progressive aphasia. To date, there are no approved symptomatic or disease-modifying treatments for frontotemporal dementia. Currently used therapies are supported by low-level of evidence (mostly uncontrolled) studies. The off-label use of drugs is also limited by their side-effect profile including an increased risk of confusion, parkinsonian symptoms, and risk of mortality. Emerging disease-modifying treatments currently target the progranulin and the expansion on chromosome 9 open reading frame 72 genes as well as tau deposits. Advancing our understanding of the pathophysiology of the disease and improving the design of future clinical trials are much needed to optimize the chances to obtain positive outcomes.
Similar content being viewed by others
Frontotemporal dementia is a heterogeneous spectrum of neurodegenerative disorders with no approved treatment |
Currently used drugs have limited efficacy on the subgroup of clinical symptoms they target; they involve antidepressants, antipsychotics, mood regulators, lithium, oxytocin, dopamine agonists, stimulants, and anti-dementia medications |
Improving the design of future clinical trials is needed, notably enlarging the sample size, refining inclusion criteria based on objective biomarkers of the disease, as well as developing specific and reliable assessment tools of the outcomes |
1 Introduction
Frontotemporal dementia (FTD) is the second most common form of early-onset dementia after Alzheimer’s disease (AD) [1], with a prevalence of 0.8/100,000 among all dementias [2]. These numbers are thought to be an underestimation of the true epidemiology of the disorder; the diagnosis is often missed because of the similarities between the behavioral clinical features and other psychiatric disorders [3].
Recent advances in the understanding of the pathophysiology of FTD lead one to believe that FTD is a heterogeneous spectrum of neurodegenerative disorders. Neuropathologically, FTD belongs to a class of neurodegenerative disorders called tauopathies when the cellular inclusion bodies comprise tau proteins (FTD-tau) [4]. When these inclusions comprise TAR DNA binding protein 43 kDa-TDP-43, the disorder is categorized as FTD-TDP [5]. Only around 10% of FTD cases are referred to as FTD-fused in sarcoma (FTD-FUS); they involve ubiquitinated inclusions, neuronal intermediate filament inclusions, and basophilic inclusion bodies that are immunoreactive for the FUS [6].
The clinical presentation of FTD is also heterogeneous, with a behavioral variant (bvFTD) [7] and two language variants grouped under the primary progressive aphasia (PPA) subtype [8]. From a genetic perspective, several identified autosomal dominant mutations account for the high heritability of the disorder. The expansion on the chromosome 9 open reading frame 72 (C9orf72) gene is the most common worldwide cause of genetic FTD, followed by the granulin (GRN) gene and then the microtubule-associated protein tau (MAPT) gene [9]. Research has shown variable heritability across the clinical phenotypes: around 50% of patients with bvFTD endorse a strong family history, compared with 10% of patients with PPA [9].
Frontotemporal dementia symptoms include behavioral, language, cognitive, and motor components for which several treatments have been investigated. To date, no disease-modifying treatment for FTD is available. The currently used therapies are symptomatic in nature and have limited clinical efficacy and a wide array of side effects. Given the lack of a US Food and Drug Administration (FDA)-approved treatment for this challenging condition, non-pharmacological behavioral interventions targeting disease-specific behaviors and preserved functions in patients with FTD are often necessary in addition to addressing caregivers’ distress [10].
We first describe the different clinical variants of FTD, then critically review the efficacy, tolerability, and safety profile of drugs currently used off-label for the management of FTD symptoms. We also make clinical recommendations regarding each medication class based on the level of evidence from the Centre for Evidence-Based Medicine, Oxford shown in Table 1 [11]. We then explore emerging treatment options for FTD and discuss gaps in the field of clinical trial development relative to FTD treatment. For this review, we searched the PubMed database for relevant articles using the following keywords: frontotemporal dementia, frontotemporal lobar degeneration, FTD, FTLD, efficacy, tolerability, safety, treatment, antidepressant, cholinesterase inhibitor, memantine, oxytocin, lithium, antipsychotic, antiepileptic, bromocriptine, carbidopa/levodopa, and stimulant.
2 Clinical Variants of FTD
2.1 bvFTD
The most common clinical subtype of FTD is bvFTD, comprising around 50% of all FTD cases in the USA and Europe [3]. The characteristic clinical finding is a significant progressive shift in personality and behavior from the premorbid baseline [12]. Typical behavioral changes include loss of inhibition (making offensive remarks, inappropriate social behavior, and poor judgment), apathy, loss of empathy (often noticed by caregivers as a coldness towards individuals’ feelings) [13, 14], hyperorality (altered food preferences, binge eating, or consumption of inedible foods), and compulsive behaviors such as stereotyped speech, repetitive gestures, or complex rituals such as hoarding or cleaning [15, 16]. As the disease advances, disinhibition and compulsive behaviors will fade while apathy becomes markedly more pronounced, reflecting a progressive degeneration of the medial frontal cortex. Apathy may present in different ways and is commonly mistaken for depression. Affective apathy presents as indifference, whereas motor apathy manifests as a decreased drive to move or reduced overall movement [17].
Parkinsonism may also be associated with late-stage disease. Approximately 20% of patients with bvFTD progress to develop the signs and symptoms of motor neuron disease (MND), including upper motor neuron signs (hyper-reflexia and spasticity) and lower motor neuron signs (muscle atrophy, fasciculations) [18]. The international consensus criteria for bvFTD were published by the International Behavioral Variant FTD Criteria Consortium [7].
2.2 PPA
Primary progressive aphasia is characterized by progressive speech and language impairment (aphasia) presenting as the primary symptoms without significant cognitive, physical, or behavioral components. It manifests as deficits in word finding, usage, comprehension, and sentence construction, which are apparent during everyday conversations and through speech and language evaluations [19]. Activities of daily living are maintained, except for areas pertaining to language (e.g., difficulty using the telephone). Neurodegeneration occurs primarily in the language-dominant (usually left) hemisphere. Depending on the distribution of neuronal loss within the language network, agrammatic, semantic, and logopenic variants are identified. The first two variants have been associated with FTD pathology and are detailed further below, whereas the logopenic variant has been associated with AD pathology. At later stages of the disease, degeneration of other cognitive domains may occur, although language remains the principal domain affected [8].
2.2.1 Agrammatic PPA
Also known as the non-fluent variant PPA (nfvPPA), it is a motor speech deficit concerning the production of linguistic units of sound (phonemes) causing articulatory difficulties. Clinical manifestations include halting speech with speech-sound errors, distortions, and agrammatism in language production [8]. Apraxia of speech, especially in vowel production, is evident with iterative exercises. Such deficits correspond to atrophy of the left inferior frontal gyrus and posterior fronto-insular regions [20]. Speech comprehension is spared for simple sentences or single words but becomes apparent for complex sentence structures with difficult syntax. Object knowledge is also spared [8]. While early disease is restricted to expressive language difficulties, a more global dementia will occur over time, with loss of autonomy in activities of daily living around 6–7 years after the onset of the disease. Certain individuals may develop behavioral changes, MND, or corticobasal degeneration [21].
2.2.2 svPPA
Alternatively known as the “temporal variant FTD”, the semantic variant FTD (svPPA) is characterized by deficits in single-word comprehension and object naming. Fluency, repetition, syntax, and grammar remain intact. Early on, the ability to understand single object words is impaired while comprehension of complete sentences is preserved. Comprehension of low-frequency words (giraffe) is lost before high-frequency words (dog). As the disease progresses, comprehension becomes more globally impaired. Patients may also exhibit dyslexia or dysgraphia as knowledge of semantic details of certain words (characteristics of objects) is lost [22]. Neurodegeneration of the left temporal lobe yields the described language-based symptoms. Right temporal lobe involvement leads to impaired recognition of familiar and famous faces in addition to alteration of eating preferences with food restrictions (compared to binge eating in bvFTD) and bizarre food choices [23]. Patients with the left temporal lobe variant tend to develop enhanced functions of the right side such as visual attention, leading to visual compulsions (repetitive jigsaw puzzle activities and brightly colored objects collection). Those with the right temporal lobe variant develop verbal compulsions involving words and symbols (e.g., writing notes, letters, and telephone numbers) [3]. Spread of the disease from the anterior temporal lobes to mesial temporal and orbitofrontal cortices results in episodic memory decline and behavioral changes, respectively [3, 24].
3 Efficacy of Current Symptomatic Treatments for FTD
Treatment of FTD symptoms is individualized and depends on the array of symptoms presented by the patient [25]. We review clinical trial efficacy data of currently available treatments that are targeted towards addressing neurotransmitter disturbances. The majority of studies in FTD have found a serotoninergic deficit that seems to be more postsynaptic than presynaptic, in addition to basal ganglia dopamine dysregulation, while both the cholinergic and noradrenergic systems seem to remain intact [26].
3.1 Antidepressants
3.1.1 SSRIs
Selective serotonin reuptake inhibitors (SSRIs) including citalopram, sertraline, fluoxetine, paroxetine, and fluvoxamine have been studied for the management of disinhibition, stereotypies, dietary changes, and hypersexual behaviors in patients with FTD, with mixed results stemming mainly from uncontrolled studies. However, SSRIs have been used as first-line off-label treatment.
Fluoxetine, sertraline, and paroxetine were investigated in a 3-month open-label study in 11 patients with FTD, showing improvement in disinhibition, depressive symptoms, carbohydrate craving, and compulsions in at least half of the subjects [27].
Paroxetine (dose of 20 mg daily given for 14 months) led to a statistically significant improvement of behavioral symptoms in eight patients with FTD diagnosed according to the Lund and Manchester criteria, with no specification of subtypes. This positive outcome was assessed using the Behavioral Pathology in the Alzheimer’s Disease BEHAVE-AD rating scale (change of 13.075 points over piracetam 2400 mg/day ; p < 0.01), change in the neuropsychiatric interview (Neuropsychiatric Inventory [NPI]) total scores (by 8.25 points over baseline; p < 0.05; by 13.25 points over piracetam; p < 0.01), and the Cornell Scale for Depression (by 3.15 points over piracetam; p < 0.01) [28]. In a 4-week, placebo-controlled cross-over randomized controlled trial (RCT), paroxetine at the dose of 40 mg daily failed to show a statistically significant difference in the NPI or the Cambridge Behavioral Inventory in ten enrolled participants with bvFTD. On the contrary, it led to a decrease in accuracy on the paired associates learning task, reversal learning, and a delayed pattern recognition task [29].
In another observational trial of 35 patients with FTD (16 bvFTD, 10 nfVPPA, and 9 svPPA), a higher dose of paroxetine (40 mg twice daily) was found to decrease or eliminate repetitive and ritualistic behaviors in 75% of the patients who took it (8 out of 11 patients). Patients were prescribed this treatment by their primary care physicians or neurologists based on subjective criteria reported by caregivers. Reports of improvements were either per caregivers’ reports or clinicians’ observations. No NPI measures pre-treatment and post-treatment were performred [30].
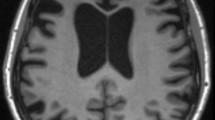
Sertraline (doses between 50 and 100 mg daily) significantly decreased verbal and motor stereotypies as measured by the Abnormal Involuntary Movement Scale in an observational trial in 18 patients with bvFTD [31]. Citalopram (a single dose of 30 mg) was studied for the treatment of disinhibition in a randomized, double-blind, placebo-controlled cross-over study that included 12 right-handed patients with bvFTD. In addition, 20 healthy older adults served as controls. The ability to inhibit inappropriate responses was assessed using the Go/No-Go task. Participants also underwent magnetoencephalography/electroencephalography and brain magnetic resonance imaging. Controls underwent a magnetoencephalography/electroencephalography protocol in one session without citalopram providing normative data for this task. The right inferior frontal gyrus and anterior temporal lobe were identified as cortical sources associated with successful inhibition in controls. This study showed that citalopram increased the No-Go P3 signal (inhibition) when compared with placebo treatment in the patients, in addition to the evoked response in the right inferior frontal gyrus. No impact on patients’ accuracy and reaction time, however, was observed. These findings corroborate the hypothesis of serotonin dysfunction in the prefrontal cortex of patients with FTD and their potential improvement with SSRIs [32].
In another study, citalopram was administered at a dose of 30 mg (single dose/challenge test) followed by a 6-week open-label phase when it was titrated from 10 mg up to 40 mg daily depending on tolerability. Included patients were diagnosed with FTD per the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criteria and had significant behavioral symptoms as demonstrated by a NPI score ≥ 8. A total of 15 patients were divided as follows: 12 bvFTD, 2 nfvPPA, and 1 svPPA, with a mean age of 67.2 ± 8.5 years. A significant decrease in NPI was noted with citalopram treatment for behavioral symptoms (p = 0.004), disinhibition (p = 0.029), irritability (p = 0.003), and depression (p = 0.045) scores over 6 weeks, with no effect on measures of cognition or activities of daily living [33]. At the dose of 20 mg daily administered over the course of a year, citalopram was shown to notably improve obsessive compulsive symptoms with a slight overall improvement in total NPI scores in an 80-year old male patient with bvFTD [34].
In a 12-week open-label trial, fluvoxamine (doses between 50 and 150 mg daily) was explored in 12 patients with FTD (three subtypes) having a mean Mini-Mental State Examination (MMSE) of 13.8 ± 9.5. Compared with baseline, a statistically significant improvement of behavioral disturbances was shown on the NPI total score and the aberrant motor behavior NPI subcomponent (p < 0.05 for both) at week 12. Additionally, stereotyped behaviors significantly improved as reflected by the Stereotypy Rating Inventory total score (p < 0.01) when compared with baseline. It is noteworthy that each component of the Stereotypy Rating Inventory was found to be significantly improved (eating, roaming, speaking, movements, and daily rhythm; p < 0.05). There was no change in cognition as measured by the MMSE [35].
3.1.2 Trazodone
Trazodone is an atypical serotoninergic antidepressant that works as a serotonin (5-HT2) antagonist and reuptake inhibitor. It also blocks the histamine and alpha-1-adrenergic receptors. In a 6-week randomized, double-blind, placebo-controlled cross-over study, 31 patients meeting the Lund and Manchester Group criteria for FTD, with a score of 13 on the Frontal Behavioral Dysfunction Scale and a total score on the NPI >8 were included (no subtypes specified). Trazodone used at doses of 150–300 mg was associated with a significant decrease in the NPI total score (p = 0.028) in 16 out of 31 patients. Based on a multivariate analysis, patients experiencing more severe eating disorders at baseline obtained the greatest behavioral benefit from trazodone (p = 0.04) [36].
A follow-up extension study to this RCT was conducted after the end of the double-blind trial, with regular assessments of the NPI total scores at a dose of 300 mg of trazodone daily. The drop-out rate was 23% during the first 12 months and 15% after 12 months: two patients died because of causes unrelated to the study drug. Two patients were institutionalized and lost to follow-up and two patients dropped out and refused follow-up. The mean duration of follow-up by the remaining 16 patients was 36.7 months (±11.5). In these subjects, the NPI total score was significantly lower at follow-up than at baseline (p < 0.0005). No impact on cognition was observed [37].
Recommendation SSRIs can be used to treat agitation, disinhibition, stereotypies, obsessions/compulsions, eating disturbances, and depression in FTD (grade C; level of evidence 4). Another antidepressant, trazodone, can be used at the doses of 150–300 mg daily to treat neuropsychiatric symptoms (grade B; level of evidence 2b). Robust large RCTs are however needed to confirm these findings, especially that the serotoninergic deficits seen in FTD are postsynaptic, questioning the role/impact of SSRIs.
3.2 Anti-Dementia Therapies
3.2.1 Cholinesterase Inhibitors
In an open-label study involving 40 patients with FTD (unspecified type) followed for a year taking rivastigmine 3–9 mg/day, there was a statistically significant reduction of 15.1 ± 4.2 points on the NPI (p < 0.001 vs baseline and control) and 4.4 ± 3.3 points on the BEHAVE-AD (p < 0.001 vs baseline and control). Rivastigmine also reduced caregiver burnout at 12 months of treatment reflected by a reduction of 16 ± 7.1 points on the Relatives’ Stress Scale scores (p < 0.001 vs baseline and control). However, no impact on cognitive decline was shown using the MMSE [38]. Both donepezil and rivastigmine were associated with improvements in MMSE and the clock-drawing test in a sample of four male patients with FTD (unspecified subtype) compared with no/minimal improvement in female patients (n = 5). Other variables could have accounted for this sex difference including the age of the participants according to the investigators [39].
Galantamine (doses 16–24 mg daily) was investigated in an 18-week open-label trial followed by an 8-week, double-blind placebo-controlled trial in 36 patients with FTD (both bvFTD and PPA). The primary efficacy assessments were changes from week 18 to 26 in the Frontal Behavioral Inventory (FBI), the Aphasia Quotient of the Western Aphasia Battery, and the Clinical Global Impressions of Improvement (CGI-I) and of Severity (CGI-S). Only 18 patients (eight bvFTD and ten PPA) completed the entire trial including the RCT phase. Galantamine was not shown to be effective in the bvFTD group. The CGI-S was in favor of galantamine in the PPA subgroup (p = 0.009) in the placebo-controlled withdrawal phase but this was not significant when the Bonferroni correction was applied for multiple comparisons [40]. It has been discussed that a cholinergic deficit may be present in the language variants of FTD compared to the bvFTD subtype, inciting researchers to further investigate this class of medication in certain phenotypes of the disease such as PPA [41].
In another study, 12 patients with bvFTD taking donepezil (10 mg daily, for 6 months) were compared to 12 controls. The assignment to receiving the drug vs placebo was based on the consent of patients and caregivers and was not random. The assessment included the MMSE scores, the Clinical Dementia Rating (CDR) scale, and the FTD Inventory completed by both physicians and caregivers who were not blind to diagnosis or treatment. Treated subjects did not significantly differ on MMSE or CDR scores at 6 months; however, they had worse FTD Inventory difference scores between baseline and 6 months (p < 0.05). Caregivers noticed increased episodes of socially inappropriate acts or intrusive behaviors (inappropriate comments, approaching strangers) and more stereotypical and repetitive behaviors in this subset of patients [42]. Delirium was also described in a 43-year-old male patientswith bvFTD diagnosis developed 2 weeks after initiation of donepezil (10 mg/day); confusion was reversible upon discontinuation of the medication [43].
3.2.2 NMDA-Receptor Antagonist/Memantine
Two RCTs explored the effect of memantine (dose of 10 mg twice daily) in patients with bvFTD. In the first study, the primary endpoint was the Clinician’s Interview-Based Impression of Change Plus Caregiver Input, and showed no significant differences between the memantine group (n = 23) and placebo (n = 26), 52 weeks after baseline (p = 0.4458). In the qualitative analysis, ten patients had worsened on the Clinician’s Interview-Based Impression of Change Plus Caregiver Inpu scores in the memantine group vs 17 in the placebo group, though the difference did not reach statistical significance (p = 0.142) [44].
The second study was a multicenter 26-week RCT including patients with bvFTD and svPPA. Use of cholinesterase inhibitors was prohibited while use of antidepressants was permitted if the dose had been stable for a month prior to study entry. The primary outcomes were the NPI and the Clinician’s Global Impression of Change. Secondary outcomes included but were not limited to the CDR sum of boxes and the MMSE. Eighty-one patients (64 bvFTD and 17 svPPA) were randomly assigned to memantine (n = 39 of which there were 37 completers) or placebo (n = 42 of which there were 39 completers). There were no statistically significant differences on the NPI or Clinician’s Global Impression of Change (p-values of 0.24 and 0.9, respectively). No positive effect was found on any of the secondary outcome measures. The memantine group displayed worse neuropsychological performance compared with placebo on tests of naming and processing speed [45].
Negative results stemming from these RCTs may have been due to insufficient sample sizes. A recent meta-analysis of these two trials aimed at enlarging the sample size (130 subjects) and increasing power to detect a difference. There were however no significant differences in the CGI, MMSE, NPI, and Zarit Burden Inventory total scores between memantine and placebo treatment groups. However, the CGI scores were trending towards significance (p = 0.06) inciting researchers to conduct further larger trials in this direction [46].
Recommendation: Cholinesterase inhibitors are not recommended to slow cognitive decline in patients with bvFTD (grade C; level of evidence 4). However, galantamine (16–24 mg daily) may be particularly effective in the PPA variant (grade B; level of evidence 2b) and warrants further investigation.
Memantine (20 mg daily) is not recommended in both subtypes of FTD and is even associated with worsening cognitive performance (grade A; level of evidence 1a).
3.3 Oxytocin
Oxytocin is a neuropeptide implicated in human social behavior and cognition. Neuroimaging studies have demonstrated its role in modulating neuronal circuits underlying emotional processing and involving frontal and temporal lobes, particularly the amygdala and insular lobe [47, 48].
In a double-blind, placebo-controlled, randomized cross-over design, 20 patients with bvFTD received one dose of 24 IU of intranasal oxytocin or placebo and then completed emotion recognition tasks. Caregivers also completed behavioral ratings at 8 hours and 1 week following drug administration. A significant improvement in NPI scores was shown at 8 hours but not at 1 week, when compared with placebo and baseline [49].
A more recent dose-finding RCT was conducted testing three doses (24, 48, or 72 IU) administered twice daily for 1 week to 23 patients with bvFTD or svPPA. Non-significant trends for improvement in subscales of the NPI, FBI, and Interpersonal Reactivity Index, which assesses empathy, were observed in the oxytocin group compared with placebo. Improved patient–caregiver interactions were also reported by informants. The higher dose of 72 IU seemed to be the most promising in terms of efficacy on empathy and apathy measures [50].
Recommendation Intranasal oxytocin (24 up to 72 IU) may be effective in improving empathy and patient-caregiver interaction (grade B; level 2b). Larger, sufficiently powered RCTs are needed to confirm this finding.
3.4 Lithium
Lithium is a well-known mood regulator approved for the treatment of bipolar disorder. At low doses, lithium is shown to be neuroprotective in tauopathies such as AD and FTD owing to its inhibitory effects on glycogen synthase kinase-3 and tau phosphorylation [51]. More recently, these effects were found to be significant in subjects carrying specific genetic variations in the UNC13 presynaptic protein, occurring in both FTD and other psychiatric disorders [52]. In a case series of three patients with bvFTD or svPPA, lithium used at doses between 300 and 1200 mg daily improved behavioral disturbances notably agitation with or without psychotic features. Serum lithium concentrations ranged between 0.4 and 0.8 mmol/L [53].
A currently enrolling, phase II, randomized, placebo-controlled, double-blind, 12-week trial (NCT02862210) involves 60 patients with FTD taking 150 mg of lithium titrated progressively to 600 mg daily depending on tolerance. The primary outcome measures are changes in agitation and aggression as measured by theses subscales of the NPI at week 12.
Recommendation Lithium (dose to be adjusted according to serum concentrations) can be recommended to treat agitation in patients with FTD (grade C; level of evidence 4).
3.5 Antipsychotics
Aripiprazole (10 mg/day, administered for 13 months) was found to partially restitute impaired frontal glucose metabolism and improve behavioral disturbances, notably apathy in a 73-year-old male patient with bvFTD [54]. Different doses of aripiprazole (18 and 30 mg/day for 2 weeks) were shown to improve inappropriate sexual behavior and vocalizations in two cases with bvFTD [55, 56].
Olanzapine was studied in a case series of 17 patients with bvFTD with a mean age of 69.5 ± 3.5 years who were followed for 24 months. Stereotypical behavior, perseverations, mood changes, and reduced interest were the dominant symptoms as reflected by NPI and BEHAVE scores; they were closely correlated with caregiver distress (p < 0.01). Behavioral symptoms were shown to be managed with an average daily dose of 3 ± 0.71 mg of olanzapine. There was a statistically significant decrease in delusions (p < 0.01), and other behavioral symptoms as reflected by a decrease in the NPI and BEHAVE scores (p < 0.01 and p < 0.05, respectively). Caregiver stress was also significantly reduced (p < 0.01) when compared to baseline [57]. Double-blind placebo-controlled trials are required to confirm this finding. A case series of three patients with FTD (unspecified subtype) showed that quetiapine at a dose of 250 mg in the morning and 500 mg at bedtime improved subjective reports of agitation without exacerbating parkinsonism [30], while risperidone (6 mg daily) specifically improved psychosis in a 42-year-old woman with bvFTD [58].
Recommendation Antipsychotics can be cautiously used to treat psychosis and extreme cases of agitation in patients with any subtype of FTD (grade C; level of evidence 4). Clinicians should be vigilant about the FDA warning regarding the associated increased risk of mortality with their use in cognitively impaired individuals.
3.6 Antiepileptic Drugs
The literature is scarce on the use of antiepileptic drugs in FTD. A successful response to carbamazepine 800 mg/day (serum concentration of 6 mg/L) was reported in a 78-year-old male patient with Kluver–Bucy syndrome concomitant with bvFTD, and experiencing inappropriate sexual behavior that did not respond to paroxetine 40 mg/day. The treatment effects lasted for 6 months before the patient was lost to follow-up [59].
Topiramate is an antiepileptic drug known for its appetite suppression action. At doses of 100–150 mg administered for 6 weeks, it was shown to reduce stereotypical and compulsive eating behaviors in several FTD cases (bvFTD and PPA) with distinct lobar atrophy involvement, as reflected by the eating behavior questionnaire [60]. Topiramate at a dose of 100 mg daily given for 7 months was shown to reduce alcohol use disorder without affecting other clinical symptoms of bvFTD (including obsessional behavior) in a 53-year-old male patient [61]. Valproic acid has been seldom used, with no proven efficacy [62].
Recommendation: Among antiepileptic drugs, topiramate (100–150 mg daily) can be used to reduce eating disturbances and alcohol use disorder in patients with FTD (grade C; level of evidence 4).
3.7 Anti-Parkinsonian Medications
Bromocriptine is a dopamine agonist used in the treatment of Parkinson’s disease that was shown to improve speech production in non-fluent aphasia after left hemisphere infarctions [63]. In a cross-over RCT, six subjects with nfvPPA and a mean age of 66.8 years received 7.5 mg of bromocriptine three times daily for 7 weeks. Only narrative language assessed via mean utterance length was improved but no statistically significant effect on overall language functions (including naming and word fluency) was found in this small trial [64].
Carbidopa/levodopa 25/250 mg given four times daily was shown to improve parkinsonian symptoms, notably rigidity and bradykinesia in two out of three patients with FTD (unspecified subtypes). In one nfv-PPA case, carbidopa/levodopa was shown to improve both speech and bradykinesia. Furthermore, six out of nine subjects with PPA responded to amantadine (100 mg, three times daily) with respect to their speech fluency and alertness levels, which were also noticed by caregivers [30].
Recommendation: In the language variants of FTD, speech fluency can be improved by using bromocriptine (grade B; level of evidence 2b) or carbidopa/levodopa and amantadine (grade C; level of evidence 4). Carbidopa/levodopa and amantadine may improve parkinsonian symptoms such as bradykinesia and rigidity (grade C; level of evidence 4).
3.8 Stimulants
Both anatomopathological and biological evidence point to a dopaminergic deficit/dysregulation in FTD, challenging the common belief that stimulant medications will aggravate FTD symptoms. In a case series of eight patients with bvFTD, dextroamphetamine 20 mg/day was administered for 3 weeks in a cross-over trial (with quetiapine 150 mg/day). The total NPI score was significantly lower in the dextroamphetamine group when compared with baseline (p = 0.02), but there was no significant difference between baseline and quetiapine, nor between quetiapine and dextroamphetamine [65].
In a 72-year-old male patient with bvFTD, immediate-release methylphenidate (10 mg administered twice daily) was shown to improve mood, affect (apathy), and impulsivity. These positive changes correlated with an improvement of the abnormally slowed cortical activity in the frontotemporal areas of the left cortex demonstrated on quantitative electroencephalography [66]. In a cross-over RCT of eight patients with bvFTD, a single dose of methylphenidate 40 mg did not affect neuropsychological performance including memory and attentional tasks performed 90 minutes after the dose, but significantly reduced betting behaviors (p = 0.0017), which reflect decision making and attenuation of risk-taking behaviors [67].
Recommendation: Stimulants may improve mood, apathy, and impulse-control in patients with bvFTD without exacerbating behavioral disturbances (grade C; level of evidence 4).
4 Tolerability and Safety of Current Treatments for FTD
Antidepressants are among the most well-tolerated symptomatic treatments for FTD. Reported side effects of SSRIs in this population include nausea [32], weight loss, and drowsiness [33] for citalopram.
Diarrhea is another reported gastrointestinal side effect that prompted discontinuation of sertraline in one subject [27]. Three of eight patients (37.5%) taking paroxetine reported transitory nausea during the first days of therapy, which resolved spontaneously within 10 days. No serious adverse events were reported with no cardiac rhythm alteration or blood pressure modification [28]. In another trial of paroxetine, one patient discontinued the drug because of increased anxiety [27]. Headaches were also described with paroxetine [30]. Similarly, fluvoxamine was well tolerated except for nausea/loss of appetite in one subject, leading to treatment discontinuation [35]. Mild adverse events were reported with trazodone compared with placebo: 11/26 patients taking trazodone reported fatigue, dizziness, hypotension, and cold extremities [36]. The longest duration of follow-up of patients with FTD taking trazodone was 2 years and showed that hypotension was the single general side effect, corrected with midodrine in 4 out of 26 patients. No patient discontinued the treatment because of this adverse event [37].
Among cholinesterase inhibitors, donepezil was shown to increase confusion and worsen behavioral symptoms. Cholinesterase inhibitors are also associated with increased oral secretions contributing to aspiration in patients with FTD and associated MND [68].
Memantine was overall well tolerated with no statistically significant difference in all-cause discontinuation in either of the two RCTs with this drug [46]. In one study, it was associated with a numerically higher proportion of cognitive adverse events (confusion, memory loss, language disorders) and worse neurocognitive performance [45].
Intranasal oxytocin was found to be safe and well tolerated in patients with FTD, with all three doses tested (24, 48, and 72 IU twice daily), except for mild increases in hypersexual behaviors (one third of the patients receiving the drug vs 14% of placebo patients) [50].
Lithium was poorly tolerable, and was associated with an increased risk of falls, in addition to sedation and tremor, especially at high doses (around 1200 mg/day) [53].
Antipsychotics should also be used with caution in patients with FTD because of the FDA boxed warning regarding the increased risk of mortality in patients with dementia, and the increased risk of falls. Additionally, patients with FTD are more sensitive to extrapyramidal symptoms (parkinsonism and tardive dyskinesias) after antipsychotic treatment because of pre-treatment nigrostriatal deficits [69]. Patients with FTD and C9orf72 expansion have been shown to have extreme sensitivity to antipsychotics; some adverse events were irreversible in some patients even after drug withdrawal [70]. For all these reasons, lower potency antipsychotics such as quetiapine are preferred, especially in patients with movement disorders. Typical antipsychotics as well as depot formulations should be avoided [69]. In addition, somnolence was the most common adverse event (31%) reported with olanzapine, followed by constipation (23%), dry mouth (11%), and fecal impaction (7%), all decreased with dose reduction. No serious adverse events were reported with olanzapine, no clinical changes in vital signs, weight, or electrocardiographic measures or alteration of glucose metabolism [57].
Sleep disturbances are the most common side effect of stimulants. A general increase in blood pressure is reported with methylphenidate, but the differences in systolic and diastolic blood pressure were not significantly different from placebo (p = 0.075) [67]. One of six participants taking bromocriptine discontinued the treatment because of intolerance to frustration as a side effect [64]. Psychosis and vivid dreams prohibited higher dosing of carbidopa/levodopa in this patient population [30]. Amantadine was associated with livedo reticularis, a reddish blue skin discoloration that was more apparent when doses exceeded 200–300 mg daily [30]. Finally, clinicians should always be vigilant to drug–drug interactions in individuals with FTD, especially as they grow older and become subject to polypharmacy [71].
5 Emerging Treatment Options for FTD
From a disease-modifying perspective, studies are underway to target the three main genetic mutations associated with FTD, summarized in Table 2.
5.1 Targeting the GRN Mutation
The GRN gene mutation leads to haploinsufficiency of corresponding messenger RNA expression leading to decreased plasma and cerebrospinal fluid (CSF) levels of progranulin protein [72, 73]. The exact effects of progranulin are still not well understood; it is theorized that this protein may have neurotrophic and synaptic effects in the central nervous system. Additionally, patients with GRN mutations have been found to have co-existing autoimmune disorders [74]. In mice models, progranulin was found to be involved in the regulation of inflammation via antagonistic effects of tumor necrosis factor-α [75]. Within the same vein of neuroinflammation, Huang et al. demonstrated the role of progranulin in suppressing aberrant microglia activation during aging [76]. Progranulin deficiency was found to be associated with complement activation and microglia-mediated synaptic pruning, leading to endo-lysosomal dysfunction and neurodegeneration [77]. A new therapeutic strategy involves suppressing C1qa and C3 activation to mitigate microglial toxicity and neurodegeneration [76].
Another theorized therapeutic approach aims at increasing or restoring progranulin levels using alkalizing drugs such as chloroquine and amiodarone [78]. A recent pilot study using amiodarone in five patients with FTD, carriers of the GRN mutation, failed to increase progranulin levels or change the disease course [79]. The effects of nimodipine, a central nervous system-penetrant calcium channel blocker, on serum and CSF progranulin levels were studied in an open-label, 8-week, dose-finding, phase I clinical trial. The study included eight GRN mutation carriers but failed to show any significant change in progranulin levels [80]. FRM-0334 (FORUM pharmaceuticals) is a histone deacetylase inhibitor involved in the epigenetic regulation of gene function. It penetrates the central nervous system and was shown to increase progranulin expression by boosting the transcription of the non-mutated copy of the gene [81]. The results of this trial have not been published yet (NCT02149160).
AL001 is a recombinant human anti-human sortilin (SORT1) monoclonal IgG1 developed by Alector in partnership with Abbvie; it was shown to restore plasma and CSF progranulin levels as shown by phase I/II trials with this product (Alector press release on phases Ib and 2 with AL001, 2020). In July 2020, a phase III, double-blind, placebo-controlled study evaluating the efficacy and safety of AL001 in participants at risk for or with FTD due to heterozygous mutations in the progranulin gene was launched. It is expected to be completed in October 2023. Monthly intravenous injections of 60 mg/kg of AL001 will be given to 180 participants with FTD for up to 18 months. The primary outcome is change in a combination of the Clinical Dementia Rating plus the NACC FTLD-Sum of Boxes (NCT04374136).
5.2 Targeting the C9ORF72 Gene
The hexanucleotide GGGGCC repeat expansion in the noncoding region of the C9ORF72 gene seems to be the most frequent form of genetic abnormality in familial and sporadic FTD. It is still unclear which exact mechanism is responsible for neurodegeneration. One of the most likely hypotheses seems to be the gain of function achieved through the production of toxic RNA containing the GGGGCC repeat [82]. The antisense oligonucleotide are synthetic nucleic acids complementary to the C9ORF72 RNA transcript sequence. They are thought to inactivate the RNA foci of a target gene via direct binding or by inducing RNAse-mediated cleavage to decrease neurodegeneration [83, 84]. Biogen partnering with IONIS Pharmaceuticals are currently investigating BIIB080 as a targeted antisense oligonucleotide treatment towards the toxic aggregates of C9ORF72 [85].
5.3 Targeting Tau
Significant efforts are targeting tau, a microtubule-associated protein that forms insoluble filamentous inclusions adversely affecting axonal transport regulation, microtubule formation, and microtubule stabilization [86]. Although tau and progranulin are located on the same chromosome 17, their neurodegenerative mechanisms seem to be different. Tau mutations appear to cause a toxic gain of function with abnormal aggregations of both three and four microtubule-binding repeat pathological tau isoforms in both gray and white matter of various brain regions [87]. Hyper-phosphorylated tau accumulates in the neuronal soma and dendrites, leading to microtubule depolymerization and affecting axonal transport. Consequent mitochondrial impairments increase the production of toxic reactive oxygen species promoting further neurodegeneration [88]. Furthermore, tau has been shown to present with similar characteristics to prions in terms of its capacity to self-propagate from cell to cell [89].
Different therapies directed at inhibiting tau aggregation, reducing tau expression, blocking tau cleavage and spreading, enhancing tau degradation, and stabilizing microtubules are being investigated [90]. Immunotherapy targeting a reduction in endogenous tau levels has been extensively studied: injection of anti-tau antibodies to various tau epitopes in tau transgenic mice models was associated with decreased tau pathology and both cognitive and functional improvement reflecting a delay in disease progression [91,92,93].
Beyond preclinical data, two other monoclonal humanized anti-tau antibodies are being investigated in subjects with FTD/progressive supranuclear palsy: ABBV-8E12 (Abbvie) was studied at doses between 2.5 and 50 mg/kg in 30 patients with progressive supranuclear palsy/FTD and showed a good tolerability and safety profile, moving this product to phase II trials [94]. Ascending doses of BIIB092 (up to 4200 mg) given as a single intravenous dose demonstrated a dose-dependent suppression of unbound N-terminal tau in CSF in a sample of 65 healthy participants [95].
Tau aggregation inhibitors are being investigated in bvFTD. Leuco-methylthioninium (LMT/TRx0237), a stabilized reduced version of methylthioninium chloride, is a potent inhibitor of pathological aggregation of tau and TDP-43 proteins. In 2018, LMT was granted orphan drug designation by the FDA for the treatment of FTD [96]. A 52-week phase III clinical trial involving LMT (100 mg/twice daily) failed to show any clinical benefit on the Addenbrookes Cognitive Examination—Revised or the Functional Activities Questionnaire. It also failed to reduce progression of whole brain atrophy, when compared to placebo. Given that LMT turns urine blue, the placebo group received 4 mg of LMT twice daily to maintain blinding. This small dose was not expected to have any clinical effect based on an earlier phase II AD trial with methylthioninium chloride determining that 138 mg was the minimally effective dose [97]. However, a further pharmacokinetic analysis of exposure-response profiles and clinical and magnetic resonance imaging biomarker outcomes showed that the dose of 8 mg/day led to blood concentrations in the range of 0.3–0.6 ng/mL, associated with clinical Addenbrookes Cognitive Examination—Revised and Functional Activities Questionnaire scales and magnetic resonance imaging volumetric outcomes. Surprisingly, higher plasma concentrations in the range of 7–14 ng/mL for subjects receiving the 200 -mg/day dose were associated with worse outcomes [98]. Failure to meet primary endpoints was similarly found in AD trials when the higher dose was compared to the lower 8-mg/day LMT dose [99].
Other drugs targeting post-translational tau modifications such as acetylation or improving microtubule stabilization are being explored but they are still at earlier phases of clinical development [100].
6 Conclusions
Frontotemporal dementia is both an uncommon and complex disorder with a wide array of clinical symptoms posing important challenges in designing successful clinical trials aimed at developing effective pharmacotherapy for this debilitating disease [100]. Clinical heterogeneity stems from the complex functions of the frontal and temporal lobes and to what extent these functions are affected in various forms of the disease. Unfortunately, currently available evidence on symptomatic treatments stems from small uncontrolled trials (case reports and case series) and low-quality RCTs where subjects are being grouped under the same FTD diagnosis umbrella. Advances in the development of therapies for FTD require developing widespread clinical networks based on multicenter collaborative initiatives to mitigate recruitment challenges and enlarge sample sizes. Another major limitation of the existing trials is the heterogeneity of the tools used to assess behavioral outcomes such as the FBI, Cambridge Behavioral Inventory, NPI, and BEHAVE-AD, some of which were not specifically designed for FTD but were initially developed and validated for other types of dementias such as AD [25]. The FBI for instance was shown to have excellent sensitivity and specificity (97 and 95%, respectively) in discriminating between bvFTD and non-FTD while the NPI score was not found to discriminate FTD from AD [101].
New personalized endpoints that are clinically meaningful to individuals with FTD and their families are much needed [100]. Innovative scales have been recently developed such as the Multidomain Impairment Rating scale that also addresses the clinical heterogeneity of FTD. It involves elements of the FTD-CDR scale in addition to a visuospatial domain, domains for parkinsonism, MND, and other non-cognitive/non-behavioral aspects to more optimally identify the clinical spectrum of the disease [102]. Other scales include DAPHNE that explores six domains: disinhibition, apathy, perseverations, hyperorality, personal neglect, and loss of empathy [103]. Additionally, social cognition emerges as a specific outcome marker of FTD [104]. Instruments such as the Social Cognition and Emotional Assessment [105] and the Revised Self-Monitoring Scale are studied as potential clinical endpoint measures to be incorporated in future FTD clinical trials to assess for socioemotional sensitivity [106].
Whereas in AD, there has been a recent shift from a purely clinically based definition to a biomarker-based definition [107], we are still far from developing a similar biological definition of FTD based on specific biomarkers. A similar shift in defining FTD in the future would help to better confirm the diagnosis in included research subjects and increase the likelihood of detecting signals in clinical trials.
Like in AD research, biomarkers for FTD can be diagnostic and prognostic, assessing staging and therapeutic responses. Ideally, combining measures obtained in biofluids and imaging can yield the best combination of sensitivity, specificity, and accuracy, especially if data stem from large cohorts rather than small pilot studies, as currently [108]. When added to the clinical history, data from positron emission tomography with (18)F-fluorodeoxyglucose may increase the diagnostic accuracy of FTD. With a specificity of 97.6%, a sensitivity of 86%, and a positive likelihood ratio for FTD of 36.5; (18)F-fluorodeoxyglucose positron emission tomography has become increasingly used in clinical and research settings [109]. The development of other imaging and fluid biomarkers and incorporating new wearable technologies in the assessment of clinical endpoints will help improve the ability to efficiently measure treatment effects in future clinical trials [100, 108, 110].
The concept of precision medicine dictates that therapeutic interventions should target certain subtypes of patients or mutation carriers [70]. Currently investigated disease-modifying strategies for FTD-tau include antisense oligonucleotide suppression of MAPT, inhibition of tau phosphorylation and acetylation, stabilization of microtubules, inhibition of tau aggregation, and stimulation of tau aggregate clearance. Therapeutic approaches to the treatment of FTD-TDP include inhibition of TDP43 aggregation, stimulation of TDP43 aggregate clearance, increasing levels of progranulin, activating the autophagy–lysosome system, or modulation of the ubiquitin proteasome system [111]. Despite these advances, the pathophysiology and genetics of FTD spectrum remain obscure. More recently, in addition to known mutations in MAPT, GRN, and C9orf72 genes, new genetic pathways and loci related to immune dysregulation and inflammation were discovered pointing to new potential drug candidates [112]. Additionally, identification of mutation carriers at the asymptomatic/preclinical level will enable researchers to test disease-modifying agents at an early stage when it may still be possible to reverse the cognitive changes [100].
Gaps in knowledge must thus be filled with respect to the pathophysiology and clinical characterization of FTD, in addition to the development of reliable biomarker and specific assessment tools to optimize chances of obtaining positive outcomes in future therapeutic clinical trials. Desmarais and colleagues have thus proposed a set of recommendations to standardize future FTD clinical trials and maximize the chance of obtaining positive signals [113].
References
Vieira RT, Caixeta L, Machado S, et al. Epidemiology of early-onset dementia: a review of the literature. Clin Pract Epidemiol Ment Health. 2013;9:88–95.
Coyle-Gilchrist IT, Dick KM, Patterson K, et al. Prevalence, characteristics, and survival of frontotemporal lobar degeneration syndromes. Neurology. 2016;86(18):1736–43.
Bang J, Spina S, Miller BL. Frontotemporal dementia. Lancet. 2015;386(10004):1672–82.
Irwin DJ. Tauopathies as clinicopathological entities. Parkinsonism Relat Disord. 2016;22 Suppl 1(01):S29-33.
Mackenzie IR, Neumann M, Bigio EH, et al. Nomenclature and nosology for neuropathologic subtypes of frontotemporal lobar degeneration: an update. Acta Neuropathol. 2010;119(1):1–4.
Mackenzie IR, Neumann M, Cairns NJ, et al. Novel types of frontotemporal lobar degeneration: beyond tau and TDP-43. J Mol Neurosci. 2011;45(3):402–8.
Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134(Pt 9):2456–77.
Gorno-Tempini ML, Hillis AE, Weintraub S, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76(11):1006–14.
Greaves CV, Rohrer JD. An update on genetic frontotemporal dementia. J Neurol. 2019;266(8):2075–86.
Shinagawa S, Nakajima S, Plitman E, et al. Non-pharmacological management for patients with frontotemporal dementia: a systematic review. J Alzheimers Dis. 2015;45(1):283–93.
Oxford Centre for Evidence-Based Medicine. Levels of evidence. 2009. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. Accessed 15 Mar 2021.
Johnson JK, Diehl J, Mendez MF, et al. Frontotemporal lobar degeneration: demographic characteristics of 353 patients. Arch Neurol. 2005;62(6):925–30.
Rosen HJ, Allison SC, Schauer GF, et al. Neuroanatomical correlates of behavioural disorders in dementia. Brain. 2005;128(Pt 11):2612–25.
Rankin KP, Gorno-Tempini ML, Allison SC, et al. Structural anatomy of empathy in neurodegenerative disease. Brain. 2006;129(Pt 11):2945–56.
Woolley JD, Gorno-Tempini ML, Seeley WW, et al. Binge eating is associated with right orbitofrontal-insular-striatal atrophy in frontotemporal dementia. Neurology. 2007;69(14):1424–33.
Whitwell JL, Sampson EL, Loy CT, et al. VBM signatures of abnormal eating behaviours in frontotemporal lobar degeneration. Neuroimage. 2007;35(1):207–13.
Chow TW, Binns MA, Cummings JL, et al. Apathy symptom profile and behavioral associations in frontotemporal dementia vs dementia of Alzheimer type. Arch Neurol. 2009;66(7):888–93.
Devenney E, Vucic S, Hodges JR, et al. Motor neuron disease-frontotemporal dementia: a clinical continuum. Expert Rev Neurother. 2015;15(5):509–22.
Mesulam MM. Primary progressive aphasia and the language network: the 2013 H. Houston Merritt Lecture. Neurology. 2013;81(5):456–62.
Gorno-Tempini ML, Dronkers NF, Rankin KP, et al. Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol. 2004;55(3):335–46.
Le Rhun E, Richard F, Pasquier F. Natural history of primary progressive aphasia. Neurology. 2005;65(6):887–91.
Olney NT, Spina S, Miller BL. Frontotemporal dementia. Neurol Clin. 2017;35(2):339–74.
Iaccarino L, Crespi C, Della Rosa PA, et al. The semantic variant of primary progressive aphasia: clinical and neuroimaging evidence in single subjects. PLoS ONE. 2015;10(3):e0120197.
Hodges JR, Patterson K, Ward R, et al. The differentiation of semantic dementia and frontal lobe dementia (temporal and frontal variants of frontotemporal dementia) from early Alzheimer’s disease: a comparative neuropsychological study. Neuropsychology. 1999;13(1):31–40.
Jicha GA, Nelson PT. Management of frontotemporal dementia: targeting symptom management in such a heterogeneous disease requires a wide range of therapeutic options. Neurodegener Dis Manag. 2011;1(2):141–56.
Huey ED, Putnam KT, Grafman J. A systematic review of neurotransmitter deficits and treatments in frontotemporal dementia. Neurology. 2006;66(1):17–22.
Swartz JR, Miller BL, Lesser IM, et al. Frontotemporal dementia: treatment response to serotonin selective reuptake inhibitors. J Clin Psychiatry. 1997;58(5):212–6.
Moretti R, Torre P, Antonello RM, et al. Frontotemporal dementia: paroxetine as a possible treatment of behavior symptoms. Eur Neurol. 2003;49(1):13–9.
Deakin JB, Rahman S, Nestor PJ, et al. Paroxetine does not improve symptoms and impairs cognition in frontotemporal dementia: a double-blind randomized controlled trial. Psychopharmacology. 2004;172(4):400–8.
Chow TW, Mendez MF. Goals in symptomatic pharmacologic management of frontotemporal lobar degeneration. Am J Alzheimers Dis Other Demen. 2002;17(5):267–72.
Mendez MF, Shapira JS, Miller BL. Stereotypical movements and frontotemporal dementia. Move Disord. 2005;20(6):742–5.
Hughes LE, Rittman T, Regenthal R, et al. Improving response inhibition systems in frontotemporal dementia with citalopram. Brain. 2015;138(Pt 7):1961–75.
Herrmann N, Black SE, Chow T, et al. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. Am J Geriatr Psychiatry. 2012;20(9):789–97.
Meyer S, Mueller K, Gruenewald C, et al. Citalopram improves obsessive-compulsive crossword puzzling in frontotemporal dementia. Case Rep Neurol. 2019;11(1):94–105.
Ikeda M, Shigenobu K, Fukuhara R, et al. Efficacy of fluvoxamine as a treatment for behavioral symptoms in frontotemporal lobar degeneration patients. Demen Geriatr Cogn Disord. 2004;17(3):117–21.
Lebert F, Stekke W, Hasenbroekx C, et al. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17(4):355–9.
Lebert F. Behavioral benefits of trazodone are sustained for the long term in frontotemporal dementia. Therapy. 2006;3:93–6.
Moretti R, Torre P, Antonello RM, et al. Rivastigmine in frontotemporal dementia: an open-label study. Drugs Aging. 2004;21(14):931–7.
Lampl Y, Sadeh M, Lorberboym M. Efficacy of acetylcholinesterase inhibitors in frontotemporal dementia. Ann Pharmacother. 2004;38(11):1967–8.
Kertesz A, Morlog D, Light M, et al. Galantamine in frontotemporal dementia and primary progressive aphasia. Dement Geriatr Cogn Disord. 2008;25(2):178–85.
Noufi P, Khoury R, Jeyakumar S, et al. Use of cholinesterase inhibitors in non-Alzheimer’s dementias. Drugs Aging. 2019;36(8):719–31.
Mendez MF, Shapira JS, McMurtray A, et al. Preliminary findings: behavioral worsening on donepezil in patients with frontotemporal dementia. Am J Geriatr Psychiatry. 2007;15(1):84–7.
Arciniegas DB, Anderson CA. Donepezil-induced confusional state in a patient with autopsy-proven behavioral-variant frontotemporal dementia. J Neuropsychiatry Clin Neurosci. 2013;25(3):E25–6.
Vercelletto M, Boutoleau-Bretonnière C, Volteau C, et al. Memantine in behavioral variant frontotemporal dementia: negative results. J Alzheimers Dis. 2011;23(4):749–59.
Boxer AL, Knopman DS, Kaufer DI, et al. Memantine in patients with frontotemporal lobar degeneration: a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2013;12(2):149–56.
Kishi T, Matsunaga S, Iwata N. Memantine for the treatment of frontotemporal dementia: a meta-analysis. Neuropsychiatr Dis Treat. 2015;11:2883–5.
Wigton R, Radua J, Allen P, et al. Neurophysiological effects of acute oxytocin administration: systematic review and meta-analysis of placebo-controlled imaging studies. J Psychiatry Neurosci. 2015;40(1):E1-22.
Grace SA, Rossell SL, Heinrichs M, et al. Oxytocin and brain activity in humans: a systematic review and coordinate-based meta-analysis of functional MRI studies. Psychoneuroendocrinology. 2018;96:6–24.
Jesso S, Morlog D, Ross S, et al. The effects of oxytocin on social cognition and behaviour in frontotemporal dementia. Brain. 2011;134(Pt 9):2493–501.
Finger EC, MacKinley J, Blair M, et al. Oxytocin for frontotemporal dementia: a randomized dose-finding study of safety and tolerability. Neurology. 2015;84(2):174–81.
Noble W, Planel E, Zehr C, et al. Inhibition of glycogen synthase kinase-3 by lithium correlates with reduced tauopathy and degeneration in vivo. Proc Natl Acad Sci USA. 2005;102(19):6990–5.
Limanaqi F, Biagioni F, Ryskalin L, et al. Molecular mechanisms linking ALS/FTD and psychiatric disorders, the potential effects of lithium. Front Cell Neurosci. 2019;13:450.
Devanand DP, Pelton GH, D’Antonio K, et al. Low-dose lithium treatment for agitation and psychosis in Alzheimer disease and frontotemporal dementia: a case series. Alzheimer Dis Assoc Diord. 2017;31(1):73–5.
Fellgiebel A, Müller MJ, Hiemke C, et al. Clinical improvement in a case of frontotemporal dementia under aripiprazole treatment corresponds to partial recovery of disturbed frontal glucose metabolism. World J Biol Psychiatry. 2007;8(2):123–6.
Nomoto H, Matsubara Y, Ichimiya Y, et al. A case of frontotemporal dementia with sexual disinhibition controlled by aripiprazole. Psychogeriatrics. 2017;17(6):509–10.
Reeves RR, Perry CL. Aripiprazole for sexually inappropriate vocalizations in frontotemporal dementia. J Clin Psychopharmacol. 2013;33(1):145–6.
Moretti R, Torre P, Antonello RM, et al. Olanzapine as a treatment of neuropsychiatric disorders of Alzheimer’s disease and other dementias: a 24-month follow-up of 68 patients. Am J Alzheimers Dis Other Demen. 2003;18(4):205–14.
Curtis RC, Resch DS. Case of pick’s central lobar atrophy with apparent stabilization of cognitive decline after treatment with risperidone. J Clin Psychopharmacol. 2000;20(3):384–5.
Poetter CE, Stewart JT. Treatment of indiscriminate, inappropriate sexual behavior in frontotemporal dementia with carbamazepine. J Clin Psychopharmacol. 2012;32(1):137–8.
Shinagawa S, Tsuno N, Nakayama K. Managing abnormal eating behaviours in frontotemporal lobar degeneration patients with topiramate. Psychogeriatrics. 2013;13(1):58–61.
Cruz M, Marinho V, Fontenelle LF, et al. Topiramate may modulate alcohol abuse but not other compulsive behaviors in frontotemporal dementia: case report. Cogn Behav Neurol. 2008;21(2):104–6.
Tsai RM, Boxer AL. Treatment of frontotemporal dementia. Curr Treat Options Neurol. 2014;16(11):319.
Bragoni M, Altieri M, Di Piero V, et al. Bromocriptine and speech therapy in non-fluent chronic aphasia after stroke. Neurol Sci. 2000;21(1):19–22.
Reed DA, Johnson NA, Thompson C, et al. A clinical trial of bromocriptine for treatment of primary progressive aphasia. Ann Neurol. 2004;56(5):750.
Huey ED, Garcia C, Wassermann EM, et al. Stimulant treatment of frontotemporal dementia in 8 patients. J Clin Psychiatry. 2008;69(12):1981–2.
Goforth HW, Konopka L, Primeau M, et al. Quantitative electroencephalography in frontotemporal dementia with methylphenidate response: a case study. Clin EEG Neurosci. 2004;35(2):108–11.
Rahman S, Robbins TW, Hodges JR, et al. Methylphenidate ('Ritalin’) can ameliorate abnormal risk-taking behavior in the frontal variant of frontotemporal dementia. Neuropsychopharmacology. 2006;31(3):651–8.
Kerchner GA, Tartaglia MC, Boxer A. Abhorring the vacuum: use of Alzheimer’s disease medications in frontotemporal dementia. Expert Rev Neurother. 2011;11(5):709–17.
Pijnenburg YA, Sampson EL, Harvey RJ, et al. Vulnerability to neuroleptic side effects in frontotemporal lobar degeneration. Int J Geriatr Psychiatry. 2003;18(1):67–72.
Liu M-N, Lau C-I, Lin C-P. Precision medicine for frontotemporal dementia. Front Psychiatry. 2019;21(10):75.
Williams S, Miller G, Khoury R, et al. Rational deprescribing in the elderly. Ann Clin Psychiatry. 2019;31(2):144–52.
Finch N, Baker M, Crook R, et al. Plasma progranulin levels predict progranulin mutation status in frontotemporal dementia patients and asymptomatic family members. Brain. 2009;132(Pt 3):583–91.
Meeter LH, Patzke H, Loewen G, et al. Progranulin levels in plasma and cerebrospinal fluid in granulin mutation carriers. Dement Geriatr Cogn Dis Extra. 2016;6(2):330–40.
Miller ZA, Rankin KP, Graff-Radford NR, et al. TDP-43 frontotemporal lobar degeneration and autoimmune disease. J Neurol Neurosurg Psychiatry. 2013;84(9):956–62.
Tang W, Lu Y, Tian QY, et al. The growth factor progranulin binds to TNF receptors and is therapeutic against inflammatory arthritis in mice. Science. 2011;332(6028):478–84.
Zhang J, Velmeshev D, Hashimoto K, et al. Neurotoxic microglia promote TDP-43 proteinopathy in progranulin deficiency. Nature. 2020;31(588):459–65.
Lui H, Zhang J, Makinson SR, et al. Progranulin deficiency promotes circuit-specific synaptic pruning by microglia via complement activation. Cell. 2016;165(4):921–35.
Capell A, Liebscher S, Fellerer K, et al. Rescue of progranulin deficiency associated with frontotemporal lobar degeneration by alkalizing reagents and inhibition of vacuolar ATPase. J Neurosci. 2011;31(5):1885–94.
Alberici A, Archetti S, Pilotto A, et al. Results from a pilot study on amiodarone administration in monogenic frontotemporal dementia with granulin mutation. Neurol Sci. 2014;35(8):1215–9.
Sha SJ, Miller ZA, Min SW, et al. An 8-week, open-label, dose-finding study of nimodipine for the treatment of progranulin insufficiency from GRN gene mutations. Alzheimers Dement. 2017;3(4):507–12.
Cenik B, Sephton CF, Dewey CM, et al. Suberoylanilide hydroxamic acid (vorinostat) up-regulates progranulin transcription: rational therapeutic approach to frontotemporal dementia. J Biol Chem. 2011;286(18):16101–8.
Riboldi G, Zanetta C, Ranieri M, et al. Antisense oligonucleotide therapy for the treatment of C9ORF72 ALS/FTD diseases. Mol Neurobiol. 2014;50(3):721–32.
Miller TM, Pestronk A, David W, et al. An antisense oligonucleotide against SOD1 delivered intrathecally for patients with SOD1 familial amyotrophic lateral sclerosis: a phase 1, randomised, first-in-man study. Lancet Neurol. 2013;12(5):435–42.
Donnelly CJ, Zhang PW, Pham JT, et al. RNA toxicity from the ALS/FTD C9ORF72 expansion is mitigated by antisense intervention. Neuron. 2013;80(2):415–28.
Scoles DR, Minikel EV, Pulst SM. Antisense oligonucleotides: a primer. Neurol Genet. 2019;5(2):e323.
Young JJ, Lavakumar M, Tampi D, et al. Frontotemporal dementia: latest evidence and clinical implications. Ther Adv Psychopharmacol. 2018;8(1):33–48.
Zhukareva V, Mann D, Pickering-Brown S, et al. Sporadic Pick’s disease: a tauopathy characterized by a spectrum of pathological tau isoforms in gray and white matter. Ann Neurol. 2002;51(6):730–9.
Bodea L-G, Eckert A, Ittner LM, et al. Tau physiology and pathomechanisms in frontotemporal lobar degeneration. J Neurochem. 2016;1381 Suppl 1(Suppl 1):71–94.
Sanders DW, Kaufman SK, DeVos SL, et al. Distinct tau prion strains propagate in cells and mice and define different tauopathies. Neuron. 2014;82(6):1271–8.
Vossel KA, Miller BL. New approaches to the treatment of frontotemporal lobar degeneration. Curr Opin Neurol. 2008;21(6):708–16.
Boutajangout A, Ingadottir J, Davies P, et al. Passive immunization targeting pathological phospho-tau protein in a mouse model reduces functional decline and clears tau aggregates from the brain. J Neurochem. 2011;118(4):658–67.
Chai X, Wu S, Murray TK, et al. Passive immunization with anti-Tau antibodies in two transgenic models: reduction of Tau pathology and delay of disease progression. J Biol Chem. 2011;286(39):34457–67.
Yanamandra K, Kfoury N, Jiang H, et al. Anti-tau antibodies that block tau aggregate seeding in vitro markedly decrease pathology and improve cognition in vivo. Neuron. 2013;80(2):402–14.
West T, Hu Y, Verghese PB, et al. Preclinical and clinical development of ABBV-8E12, a humanized anti-Tau antibody, for treatment of Alzheimer’s disease and other tauopathies. J Prev Alzheimers Dis. 2017;4(4):236–41.
Qureshi IA, Tirucherai G, Ahlijanian MK, et al. A randomized, single ascending dose study of intravenous BIIB092 in healthy participants. Alzheimers Dement. 2018;4:746–55.
CISION PR Newswire. FDA grants orphan-drug designation for TauRx's LMTX in frontotemporal dementia. 2018. Available from: https://www.prnewswire.co.uk/news-releases/fda-grants-orphan-drug-designation-for-taurx-s-lmtx-in-frontotemporal-dementia-825389573.html. Accessed 15 Mar 2021.
ALZFORUM. First round of FTD therapeutics fell short, but many more are up and running. 2016. Available from: https://www.alzforum.org/news/conference-coverage/first-round-ftd-therapeutics-fell-short-many-more-are-and-running. Accessed 15 Mar 2021.
Shiells H, Schelter BO, Bentham P, et al. Concentration-dependent activity of hydromethylthionine on clinical decline and brain atrophy in a randomized controlled trial in behavioral variant frontotemporal dementia. J Alzheimers Dis. 2020;75(2):501–19.
Hashweh NN, Bartochowski Z, Khoury R, et al. An evaluation of hydromethylthionine as a treatment option for Alzheimer’s disease. Expert Opin Pharmacother. 2020;21(6):619–27.
Boxer AL, Gold M, Feldman H, et al. New directions in clinical trials for frontotemporal lobar degeneration: methods and outcome measures. Alzheimers Dement. 2020;16(1):131–43.
Milan G, Lamenza F, Iavarone A, et al. Frontal Behavioural Inventory in the differential diagnosis of dementia. Acta Neurol Scand. 2008;117(4):260–5.
Boeve B, Rosen H, Boxer A, et al. The Multidomain Impairment Rating (MIR) Scale: initial reliability data on a multidimensional scale for FTLD (P5.1–010). Neurology. 2019;92(15 Suppl.):P5.1-010.
Boutoleau-Bretonnière C, Evrard C, Hardouin JB, et al. DAPHNE: a new tool for the assessment of the behavioral variant of frontotemporal dementia. Dement Geriatr Cogn Dis Extra. 2015;5(3):503–16.
Gossink F, Schouws S, Krudop W, et al. Social cognition differentiates behavioral variant frontotemporal dementia from other neurodegenerative diseases and psychiatric disorders. Am J Geriatr Psychiatry. 2018;26(5):569–79.
Funkiewiez A, Bertoux M, de Souza LC, et al. The SEA (Social cognition and Emotional Assessment): a clinical neuropsychological tool for early diagnosis of frontal variant of frontotemporal lobar degeneration. Neuropsychology. 2012;26(1):81–90.
Toller G, Ranasinghe K, Cobigo Y, et al. Revised self-monitoring scale: a potential endpoint for frontotemporal dementia clinical trials. Neurology. 2020;94(22):e2384–95.
Jack CR Jr, Bennett DA, Blennow K, et al. NIA-AA Research Framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–62.
Swift IJ, Sogorb-Esteve A, Heller C, et al. Fluid biomarkers in frontotemporal dementia: past, present and future. J Neurol Neurosurg Psychiatry. 2021;92(2):204–15.
Foster NL, Heidebrink JL, Clark CM, et al. FDG-PET improves accuracy in distinguishing frontotemporal dementia and Alzheimer’s disease. Brain. 2007;130(Pt 10):2616–35.
Meeter LH, Kaat LD, Rohrer JD, et al. Imaging and fluid biomarkers in frontotemporal dementia. Nat Rev Neurol. 2017;13(7):406–19.
Panza F, Lozupone M, Seripa D, et al. Development of disease-modifying drugs for frontotemporal dementia spectrum disorders. Nat Rev Neurol. 2020;16(4):213–28.
Ferrari R, Hernandez DG, Nalls MA, et al. Frontotemporal dementia and its subtypes: a genome-wide association study. Lancet Neurol. 2014;13(7):686–99.
Desmarais P, Rohrer JD, Nguyen QD, et al. Therapeutic trial design for frontotemporal dementia and related disorders. J Neurol Neurosurg Psychiatry. 2019;90(4):412–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflicts of interest/Competing interests
Rita Khoury, Yu Liu, and Quratulanne Sheheryar have no conflicts of interest that are directly relevant to the content of this article. George T. Grossberg is a consultant for Acadia, Alkahest, Avanir, Axsome, Biogen, Bioxcel, Karuna, Lundbeck, Otsuka, Roche, and Takeda. He received research support from NIA, Janssen, and Roche, and is on the safety monitoring committee of Anavex, EryDel, Intra-Cellular Therapies, Merck, and Newron, and on the data monitoring committee of ITI Therapeutics.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
RK participated in the literature review, interpretation of data, and writing and revising the paper. YL and QS conducted the literature search and wrote the first draft of two sections of the paper. GG conceived the paper and critically reviewed its scientific content.
Rights and permissions
About this article
Cite this article
Khoury, R., Liu, Y., Sheheryar, Q. et al. Pharmacotherapy for Frontotemporal Dementia. CNS Drugs 35, 425–438 (2021). https://doi.org/10.1007/s40263-021-00813-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-021-00813-0