INTRODUCTION
Fatigue is a debilitating and prevalent experience for people with Multiple Sclerosis (PwMS) that can exacerbate other symptoms of MS (Fisk, Pontefract, Ritvo, Archibalnd, & Murray, Reference Fisk, Pontefract, Ritvo, Archibalnd and Murray1994; Freal, Kraft, & Coryell, Reference Freal, Kraft and Coryell1984; Homorodean, Leucuta, & Perju-Dumbravă, Reference Homorodean, Leucuta and Perju-Dumbravă2016; MacAllister & Krupp, Reference MacAllister and Krupp2005). Between 76 and 97% of PwMS report fatigue as one of their symptoms (van Kessel & Moss-Morris, Reference van Kessel and Moss-Morris2006) and 40% of PwMS report fatigue as their most disabling symptom (MacAllister & Krupp, Reference MacAllister and Krupp2005). Fatigue in MS worsens over the course of the day and can be aggravated or worsened by heat and stress among other factors (Freal et al., Reference Freal, Kraft and Coryell1984; Schwartz, Coulthard-Morris, & Zeng, Reference Schwartz, Coulthard-Morris and Zeng1996). MS-related fatigue is distinctly different from other types of fatigue. It tends to be more persistent, comes on easily, and can prevent sustained physical functioning (Homorodean et al., Reference Homorodean, Leucuta and Perju-Dumbravă2016). As such, the Multiple Sclerosis Council for Clinical Practice Guidelines has defined fatigue in the context of MS as a “subjective lack of physical and/or mental energy that is perceived by the individual or caregiver to interfere with usual and desired activities” (Multiple Sclerosis Council For Clinical Practice Guidelines, 1998). It has been suggested that secondary factors common in MS, such as sleep disturbance and mood difficulties, are involved in MS-related fatigue (Krupp, Serafin, & Christodoulou, Reference Krupp, Serafin and Christodoulou2010; Strober & Arnett, Reference Strober and Arnett2005). The disruption in daily life caused by this fatigue can manifest as interference with physical activities and difficulty with activities of daily living. It also contributes to problems maintaining full-time employment (Strober et al., Reference Strober, Chiaravalloti and DeLuca2018) and is sometimes associated with lapses in memory, concentration, and other important cognitive processes (Cadden & Arnett, Reference Cadden and Arnett2015; Jongbloed, Reference Jongbloed1998; Strober, Chiaravalloti, & DeLuca, Reference Strober, Chiaravalloti and DeLuca2018).
FATIGUE AND FATIGUABILITY
Across the literature, many terms have been used to refer to different aspects or components of fatigue, including central fatigue, peripheral fatigue, domains of fatigue (e.g., cognitive and physical fatigue), and performance fatiguability. Oftentimes, some of these terms are not clearly defined or operationalized. This occurs despite evidence that perceived fatigue and fatiguability are distinct constructs (Kluger, Krupp, & Enoka, Reference Kluger, Krupp and Enoka2013). Perceived fatigue is the subjective experience of fatigue and is often collected using self-report measures of fatigue. This may include the subjective experience of weariness, an increase in effort, or an experienced mismatch between the effort being exerted and the actual outcome or performance (DeLuca, Reference DeLuca2005; Kluger et al., Reference Kluger, Krupp and Enoka2013). Fatiguability, on the other hand, is typically measured as the rate of change in performance over a period of time, usually relative to a control or some other reference value, and is thought to be a more objective measurement of fatigue (Charvet, Serafin, & Krupp, Reference Charvet, Serafin and Krupp2014; Kluger et al., Reference Kluger, Krupp and Enoka2013). Fatiguability tends to be most associated with the domain of cognitive fatigue. Fatiguability has been examined utilizing several paradigms including where cognitive fatigue is created via effortful mental tasks, and then performance on neuropsychological measures is compared before and after this effortful task, by comparing performance at the end of a single task to performance at the beginning of that same task, or by observing performance decrement on motor tasks over time.
Perceived fatigue and cognitive dysfunction
While there is some evidence that fatigue, in healthy individuals, is correlated with neuropsychological test performance in a number of different domains including concentration, verbal memory, speed of information processing, and motor speed (Busichio, Tiersky, Deluca, & Natelson, Reference Busichio, Tiersky, Deluca and Natelson2004; Cockshell & Mathias, Reference Cockshell and Mathias2010; Johnson, Lange, DeLuca, Korn, & Natelson, Reference Johnson, Lange, DeLuca, Korn and Natelson1997; Lezak, Howieson, Bigler, & Tranel, Reference Lezak, Howieson, Bigler and Tranel2012), the literature in PwMS specifically has been mixed regarding the impact of self-reported fatigue on neuropsychological test performance. Most studies report no association between subjective reports of fatigue and cognitive deficits (Bryant, Chiaravalloti, & DeLuca, Reference Bryant, Chiaravalloti and DeLuca2004; DeLuca, Reference DeLuca2005; Krupp et al., Reference Krupp, Serafin and Christodoulou2010; Parmenter, Denney, & Lynch, Reference Parmenter, Denney and Lynch2003; Paul, Beatty, Schneider, Blanco, & Hames, Reference Paul, Beatty, Schneider, Blanco and Hames1998), but some studies report fatigue-related differences in cognitive performance (Bruce, Bruce, & Arnett, Reference Bruce, Bruce and Arnett2010; Hanken, Eling, & Hildebrandt, Reference Hanken, Eling and Hildebrandt2015; Krupp et al., Reference Krupp, Serafin and Christodoulou2010; Pokryszko-Dragan et al., Reference Pokryszko-Dragan, Zagrajek, Slotwinski, Bilinska, Gruszka and Podemski2016).
Fatiguability and cognitive dysfunction
Research on the association between fatiguability and cognitive performance has been somewhat more conclusive, with the majority of studies demonstrating that fatiguability (e.g., cognitive exertion) impairs cognitive performance over time (Johnson et al., Reference Johnson, Lange, DeLuca, Korn and Natelson1997; Krupp & Elkins, Reference Krupp and Elkins2000; Kujala, Portin, Revonsuo, & Ruutiainen, Reference Kujala, Portin, Revonsuo and Ruutiainen1995). One group of researchers has examined the neural correlates of diminished or variable performance during sustained effort over time using performance on a modified Symbol Digit Modalities (mSDMT) test as a marker of state mental fatigue (Chen et al., Reference Chen, Wylie, Sandroff, Dacosta-Aguayo, DeLuca and Genova2020; DeLuca, Genova, Hillary, & Wylie, Reference DeLuca, Genova, Hillary and Wylie2008). Results from this series of studies demonstrated that state mental fatigue was associated with greater activation in the caudate in PwMS compared to controls and that PwMS allocated neural resources less efficiently when sustaining effort over time. Another study comparing PwMS to control participants on neuropsychological test performance revealed that PwMS had a larger decline in cognitive performance than controls following cognitive effort on indices of visual memory, verbal memory, and verbal fluency (Krupp & Elkins, Reference Krupp and Elkins2000).
VARIABILITY IN PERFORMANCE
Researchers have hypothesized that the lack of consensus in the literature around the role of fatigue on cognitive performance in MS may be the result of differences in categorization or definition of fatigue, differences in methods employed to “invoke” fatiguing conditions, and method of performance measurement. We argue that the mixed findings tying reported fatigue to objective performance deficits may be the result of the method of performance measurement. Most of the literature has focused on mean differences before and after a period of mental exertion (effortful cognitive tasks). One previous study by Bryant and colleagues (2004) suggested that different performance measures may be reflective of different underlying mechanisms, thus highlighting the importance of using more than just mean-level differences. Another study found that measures of performance strategy, rather than pure performance measures, are more sensitive to cognitive fatigue in PwMS than HCs (Bryant et al., Reference Bryant, Chiaravalloti and DeLuca2004). Others have examined changes in intraindividual variability (IIV) over time and determined that this might be a more ecologically valid metric for measuring fatiguability and the impact on cognitive performance (Wang, Ding, & Kluger, Reference Wang, Ding and Kluger2014). Taken together, this suggests that measuring cognitive impairment at the intraindividual level, rather than examining group-level mean differences, might be particularly illuminating when considering the impact of fatigue in MS. Further, IIV may be conceptualized as a measurement of fatiguability over a testing session.
In a variety of clinical samples, it has been established that IIV may be a better predictor of cognitive outcome than mean differences (Burton, Strauss, Hultsch, Moll, & Hunter, Reference Burton, Strauss, Hultsch, Moll and Hunter2006; Cole, Weinberger, & Dickinson, Reference Cole, Weinberger and Dickinson2011; Haynes, Bauermeister, & Bunce, Reference Haynes, Bauermeister and Bunce2017; MacDonald, Nyberg, & Bäckman, Reference MacDonald, Nyberg and Bäckman2006). While more limited, there is some literature on the use of variability as a performance-based measure thought to reflect the impact of fatigue on performance over a period of time in MS (Bruce et al., Reference Bruce, Bruce and Arnett2010; Krupp et al., Reference Krupp, Serafin and Christodoulou2010). Bruce and colleagues (2010) examined the association between self-reported cognitive fatigue and a measure of response time variability (RTV). PwMS demonstrated higher RTV compared to HCs and RTV was highly correlated with cognitive fatigue (Bruce et al., Reference Bruce, Bruce and Arnett2010). Another study examined RTV in MS as a performance-based measure of fatiguability and demonstrated that performance on an attention task was significantly associated with perceived physical and cognitive fatigue (Aldughmi, Bruce, & Siengsukon, Reference Aldughmi, Bruce and Siengsukon2017). Holtzer et al. (2013) employed burst measurement of the SDMT and found increased variability in processing speed across repeated administrations of the SDMT. Wojowicz and colleagues (2012) compared PwMS to HCs and PwMS demonstrated greater IIV, measured by an individual standard deviation score, on all subtests of the Computerized Test of Information Processing (Wojtowicz, Berrigan, & Fisk, Reference Wojtowicz, Berrigan and Fisk2012). Group differences in cognitive impairments may not fully capture the subtle differences that can be the result of MS-related fatigue; as such, indices of variability may be more reflective of the impact of fatigue.
CURRENT STUDY
With these considerations in mind, the goal of the current study was to evaluate differences between PwMS and HCs on cognitive variability indices and examine the relationship between self-report measures of fatigue and cognitive variability between these groups. IIV was operationalized using two different measures, a maximum discrepancy score (MDS) and intraindividual standard deviation (ISD), in two cognitive domains, memory and attention/processing speed. IIV was hypothesized to mediate the group differences expected in total reported fatigue. These data are cross-sectional, and therefore it is difficult to establish the directionality of the mediation. Therefore, we will also test the reverse mediation, whereby total reported fatigue is hypothesized to mediate the group differences in IIV.
METHODS
Procedure
This study involved an analysis of data collected as part of a project examining cognitive, motor, and emotional factors in MS. Analyses from this project were run on data collected as part of this study (Arnett, Smith, Barwick, Benedict, & Ahlstrom, Reference Arnett, Smith, Barwick, Benedict and Ahlstrom2008). Participants completed a psychosocial interview and a battery of neuropsychological tests and questionnaires during a 1-day visit. This study was approved by the Institutional Review Board at the Pennsylvania State University and all participants signed informed consent prior to participating in the study.
Participants
MS group
This study included 59 PwMS (M = 10, F = 49). The mean age was 51.63 and the mean disease duration was 14.90 years. Participants for this study were recruited from the greater Central Pennsylvania area. Thompson et al.’s (2017) revised McDonald criteria were applied to determine a positive diagnosis of MS (Thompson et al., Reference Thompson, Banwell, Barkhof, Carroll, Coetzee, Comi and Cohen2018). Exclusion criteria were as follows: significant history of substance abuse, nervous system disorder other than MS, sensory impairment that could interfere with testing, developmental history of attention-deficit hyperactivity disorder (ADHD) or learning disability, significant medical condition other than MS that could interfere with cognitive or motor function, relapse or corticosteroid use within 4 weeks of participation in the study, or physical or neurological impairment that would make the testing impossible. MS course types included relapsing–remitting (n = 35), secondary progressive (n = 17), and primary progressive (n = 7). All participants were paid $100 for their participation.
Healthy control group
This study included 51 neurologically healthy community-based individuals (M = 8, F = 43). HCs were matched as closely as possible to the MS participants on demographic factors such as age, education, and gender. HCs were recruited using several methods: MS participants were asked to recommend friends, advertisements were posted in public places in Central Pennsylvania, and an ad was posted on the university newswire. HCs were also paid $100 for their participation. See Table 1 for participant demographic characteristics.
Table 1. Demographic characteristics of PwMS and HC groups
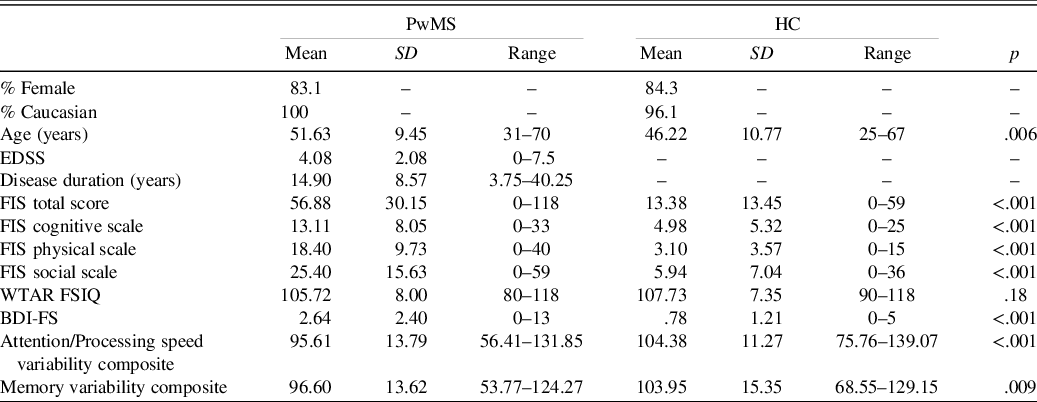
BDI-FS = Beck Depression Inventory-Fast Screen; EDSS = Expanded Disability Status Scale; FIS = Fatigue Impact Scale; HCs = Healthy Controls; PwMS = Persons with Multiple Sclerosis; WTAR FSIQ = Wechsler Test of Adult Reading Full-Scale IQ.
Measures
Fatigue
The Fatigue Impact Scale (FIS) is a 40-item self-report measure of fatigue that measures different types of fatigue including cognitive (e.g., “I have been less alert”), physical (e.g. “My muscles have felt weak”), and psychosocial components (e.g., “I have been limited in my ability to do things away from home”) (Fisk, Ritvo, et al., Reference Fisk, Ritvo, Ross, Haase, Marrie and Schlech1994). Items are rated on a 5-point Likert scale of how much of a problem fatigue has caused in the past month 0 (no problem) to 4 (extreme problem). This self-report measure has been shown to have good psychometric properties and to be sensitive to changes in fatigue in PwMS (Whitehead, Reference Whitehead2009). The three FIS scales were highly correlated in our sample, r = .64−.85, and thus the total fatigue score from this scale was used as our outcome variable.
Depression
Depression was measured using the Beck Depression Inventory-Fast Screen (BDI-FS) (Beck, Steer, & Brown, Reference Beck, Steer and Brown2000). The BDI-FS is a commonly used brief self-report measure of depression in medical populations. Previous work has identified the BDI-FS as a good screen for depression in MS since it excludes neurovegetative symptoms that commonly overlap with symptoms of MS (Benedict, Fishman, McClellan, Bakshi, & Weinstock-Guttman, Reference Benedict, Fishman, McClellan, Bakshi and Weinstock-Guttman2003; Strober & Arnett, Reference Strober and Arnett2015). It includes seven items that examinees rate based on how they have felt over the past 2 weeks. Each item has four statements that are assigned a value of 0 through 3, with lower scores indicating lower depression symptomatology.
Neuropsychological test battery
The neuropsychological test battery included the following measures: Wechsler Test of Adult Reading (WTAR; The Psychological Corporation, 2001), Digits Forward, Digits Backward (Weschler, Reference Weschler1997), Written Symbol Digit Modalities Test (SDMT), Oral SDMT (Shum, McFarland, & Bain, Reference Shum, McFarland and Bain1990), Controlled Oral Word Association Test (COWAT) Total, Animal Naming Total (Delis, Kaplan, & Kramer, Reference Delis, Kaplan and Kramer2001), Paced Auditory Serial Addition Task (PASAT) – 3-Second Trial Total Correct, PASAT – 2-Second Trial Total Correct, Visual Elevator subtest from the Test of Everyday Attention Time Per Correct Switch (Robertson, Ward, Ridgeway, & Nimmo-smith, Reference Robertson, Ward, Ridgeway and Nimmo-smith2001), 10/36 Spatial Recall Immediate Recall Total, 10/36 Spatial Recall Delayed Recall (Rao & Cognitive Function Study Group, Reference Rao1990), Brief Visuospatial Memory Test – Revised (BVMT-R) Total Immediate Recall, BVMT-R Delayed Recall (Benedict, Reference Benedict1997), and the California Verbal Learning Test-II (CVLT-II) Immediate Recall, CVLT-II Short Delay Recall, and CVLT-II Long-Delay Recall (Delis, Kramer, Kaplan, & Ober, Reference Delis, Kramer, Kaplan and Ober2000).
Scores from each test index were transformed to standard scores with a mean of 100 and a standard deviation of 15 using the sample mean and standard deviation of the HCs. Scores were created such that higher scores always indicated better performance. Comparable to previous work in other populations (Guty & Arnett, Reference Guty and Arnett2018; Riegler, Guty, & Arnett, Reference Riegler, Guty and Arnett2019), after the scores were standardized, two composites were created based on these neuropsychological test indices by taking the mean of the standard scores of tests comprising that composite. A memory composite was comprised of the 10/36 Spatial Recall Immediate Total, the 10/36 Spatial Recall Delay Total, BVMT-R Total Immediate Recall, BVMT-R Delayed Recall, CVLT-II Immediate Recall, CVLT-II Short Delay Recall, and CVLT-II Long-Delay Recall. An attention/processing speed composite was comprised of Digits Forward, Digits Backward, SDMT Written, SDMT Oral, COWAT Total, Animal Naming Total, PASAT – 3-Second Trial Total Correct, PASAT – 2-Second Trial Total Correct, and Visual Elevator Time Per Correct Switch. A principal components analysis was conducted for the tests in each composite and all of the variables loaded above .50.
Intraindividual cognitive variability indices
Once scores were standardized, the cognitive variability indices were created. Two IIV indices were derived for each of the composites created above (memory and attention/processing speed). Previous work has used the variability metric of MDS (Heyanka, Holster, & Golden, Reference Heyanka, Holster and Golden2013; Rabinowitz & Arnett, Reference Rabinowitz and Arnett2013). This metric subtracts the lowest score from the highest score for each individual participant. Other studies of IIV have used ISD as a measure of variability across a test battery. This method takes the standard deviation of the Standard Scores across the test battery (Burton et al., Reference Burton, Strauss, Hultsch, Moll and Hunter2006; Fuentes et al., Reference Fuentes, Hunter, Strauss and Hultsch2001; Merritt et al., Reference Merritt, Greenberg, Guty, Bradson, Rabinowitz and Arnett2019). Based on this previous work, we calculated these two measures of IIV for participants in our study.
Initially, four indices were created: memory MDS, memory ISD, attention/processing speed MDS, and attention/processing speed ISD. There was a high degree of correlation between the variability indices for each composite so the two variability indices for each set of tests were combined to form one measure of IIV for each set of tests. Memory ISD was significantly correlated with memory MDS, r(108) = 0.96, p < .001, and attention/processing speed ISD was significantly correlated with attention/processing speed MDS, r(108)= .77, p < .001. The two IIV indices for each domain of tests were then standardized and a memory variability composite and attention/processing speed variability composite were created as the final two outcome measures to be used in mediation analyses.
RESULTS
Data analysis
All analyses were conducted with the Statistical Package for the Social Sciences (SPSS), Version 25.0 (IBM Corporation, 2017).
Preliminary analyses
Independent samples t tests were conducted to compare demographic differences between PwMS and HCs. As shown in Table 1, PwMS were significantly older and reported significantly more depression and total fatigue. The groups did not differ on premorbid IQ as measured with the WTAR Full-Scale IQ (FSIQ) estimate. Next, bivariate correlation analyses among key variables of interest in this study were conducted (See Table 2). As seen in this table, age was significantly correlated with total fatigue scores and both IIV variables. Due to the age difference between the groups and the significant correlations between age and the mediators and outcome variables, age was included in the mediation model by regressing age on total fatigue and then using the unstandardized residuals (total residual fatigue) as the new outcome variable in the two mediation models.
Table 2. Correlations among key study variables
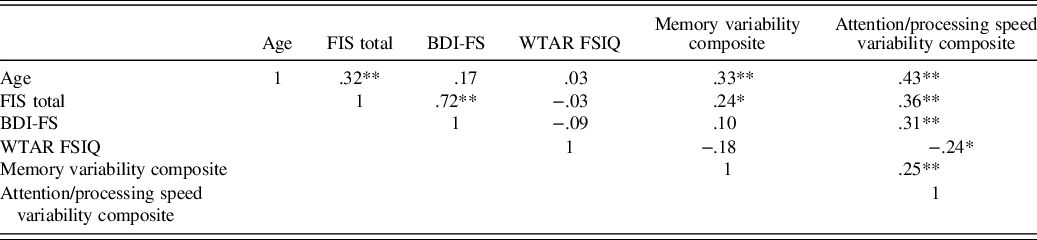
BDI-FS = Beck Depression Inventory-Fast Screen; FIS = Fatigue Impact Scale; HCs = Healthy Controls; PwMS = Persons with Multiple Sclerosis; WTAR FSIQ = Wechsler Test of Adult Reading Full-Scale IQ Estimate.
* = p < .01, ** = p < .001.
Additionally, as seen in Table 2, depression was significantly correlated with one of the mediators (attention/processing speed IIV), r = .31, p < .001, and the outcome (total fatigue), r = .72, p < .001. Since depression is more common in PwMS than in the general population, it is an important defining characteristic of our MS group compared to the HCs; estimates range from 27 to 54% of PwMS meeting criteria for clinically significant depression compared to 7–10% in the general population (American Psychiatric Association, 2013; Arnett, Barwick, & Beeney, Reference Arnett, Barwick and Beeney2008). In our sample, 18 PwMS and 1 HC met the cutoff for clinically significant depression (≥4). Previous studies have reported small to moderate effects for the relationship between depression and fatigue (Arnett et al., Reference Arnett, Barwick and Beeney2008). Further, some of the symptoms of depression are similar to symptoms of fatigue in MS (Strober & Arnett, Reference Strober and Arnett2010). To parse apart the contributions of fatigue separate from depression, depression was included as a covariate in mediation models.
Hypothesis testing analyses: mediation
Mediation analyses with group (MS or HC) as the independent variable, total age-corrected residual fatigue as the dependent variable, variability composite (memory and attention/processing speed IIV) measures as the mediators, and total BDI-FS scores as a covariate were conducted. The Preacher and Hayes approach was used to test mediation (Preacher & Hayes, Reference Preacher and Hayes2004). This method utilizes the PROCESS macro of SPSS and was used to test the strength of the indirect effect (Preacher & Hayes, Reference Preacher and Hayes2004). The indirect effect is the extent to which the dependent variable (total residual fatigue) changes when the independent variable is held fixed and the mediator (IIV) changes by the amount it would have changed had the independent variable (total residual fatigue) increased by one unit. The parameters used for the analyses of the PROCESS macro were Model 4, 5000 bootstrap samples, and a 95% bias-corrected confidence interval (CI).
Attention/processing speed variability composite as mediator
Regression analysis was used to investigate the hypothesis that attention/processing speed IIV mediates the effect of patient status on total residual fatigue after controlling for depression. Results indicate that, after controlling for depression, patient status was a significant predictor of attention/processing speed IIV, b = −5.61, t(104) =−2.14, p = .04, and that attention/processing speed IIV was a significant predictor of total residual fatigue, b = .25, t(103) = 3.38, p = .001. These results support the mediational hypothesis. Patient status was no longer a significant predictor of total residual fatigue after controlling for the mediator, attention/processing speed IIV, b = −.34, t(103) = −.17, p = .87. Results of a mediation analysis using 5000 bootstrap samples indicated that attention/processing speed IIV significantly mediated the increase in total residual fatigue in the MS group relative to the HC group, indirect effect – 1.42, 95% [−3.09, −.09]. PwMS demonstrate more attention/processing speed variability which leads to more self-reported fatigue. See Figure 1 for a graphical representation of the mediation model with attention/processing speed IIV as the mediator. When this relationship was tested in reverse, total residual fatigue did not significantly mediate the increase in attention/processing speed IIV in the MS group relative to the control group, indirect effect = −.70, 95% CI [−2.51, 1.08].
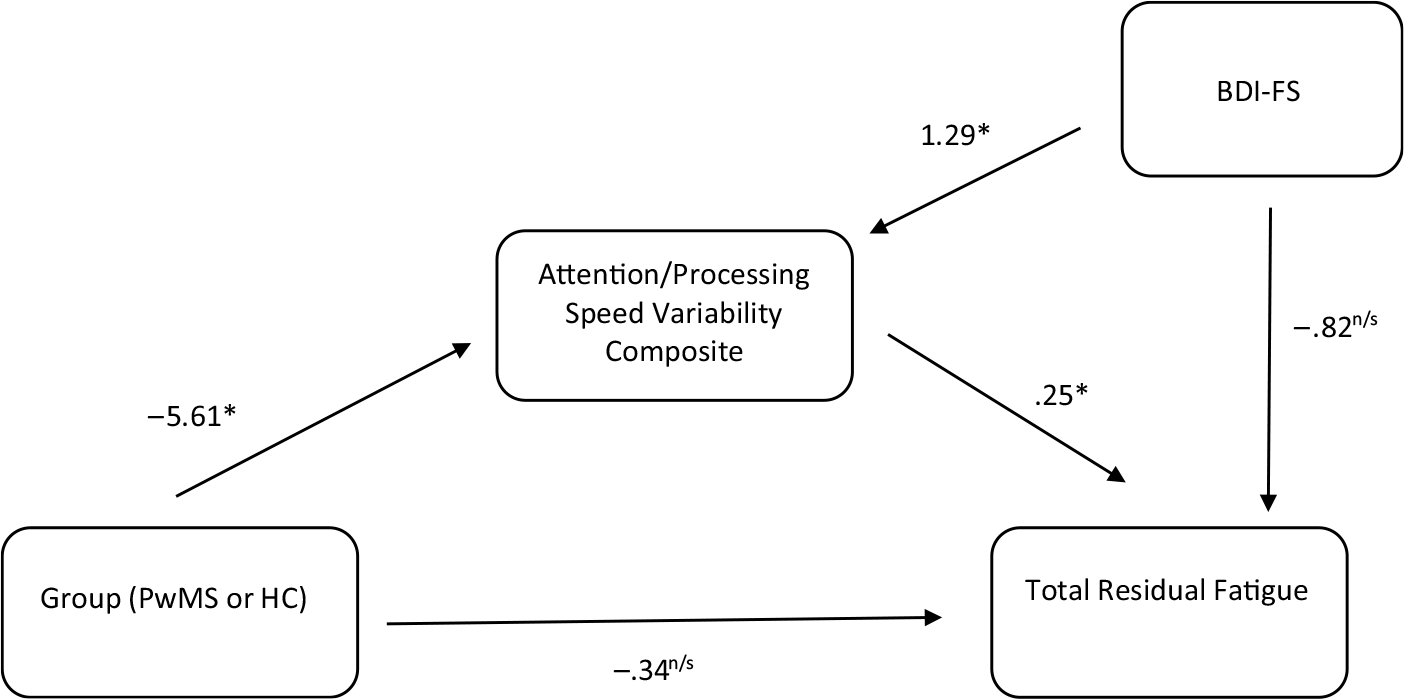
Fig. 1. Mediation model with attention/processing speed composite as mediator and depression as covariate.
BDI-FS = Beck Depression Inventory-Fast Screen; HCs = Healthy Controls; PwMS = Persons with Multiple Sclerosis.
* = p < .05, n/s = p > .05 (not significant).
Memory variability composite variability as mediator
Regression analysis was used to investigate the hypothesis that memory IIV mediates the effect of patient status on total residual fatigue after controlling for depression. Results indicate that, after controlling for depression, patient status was a significant predictor of memory IIV, b = −7.37, t(104) = −2.33, p = .02, and that memory IIV was a significant predictor of total residual fatigue, b = .17, t(103) = 2.76, p = .007. These results support the mediational hypothesis. Patient status was no longer a significant predictor of total residual fatigue after controlling for the mediator, memory IIV, b = −.48, t(103) = −.23, p = .82. Results of a mediation analysis using 5000 bootstrap samples indicated that memory IIV significantly mediated the increase in total residual fatigue in the MS group relative to the HC group, indirect effect – 1.29, 95% [−2.71, −.08]. PwMS demonstrate more memory variability which leads to more self-reported fatigue. See Figure 2 for a graphical representation of the mediation model with memory IIV as the mediator. When this relationship was tested in reverse total residual fatigue did not significantly mediate the increase in memory IIV in the MS group relative to the control group, indirect effect = −.70, 95% CI [−2.52, 1.14].
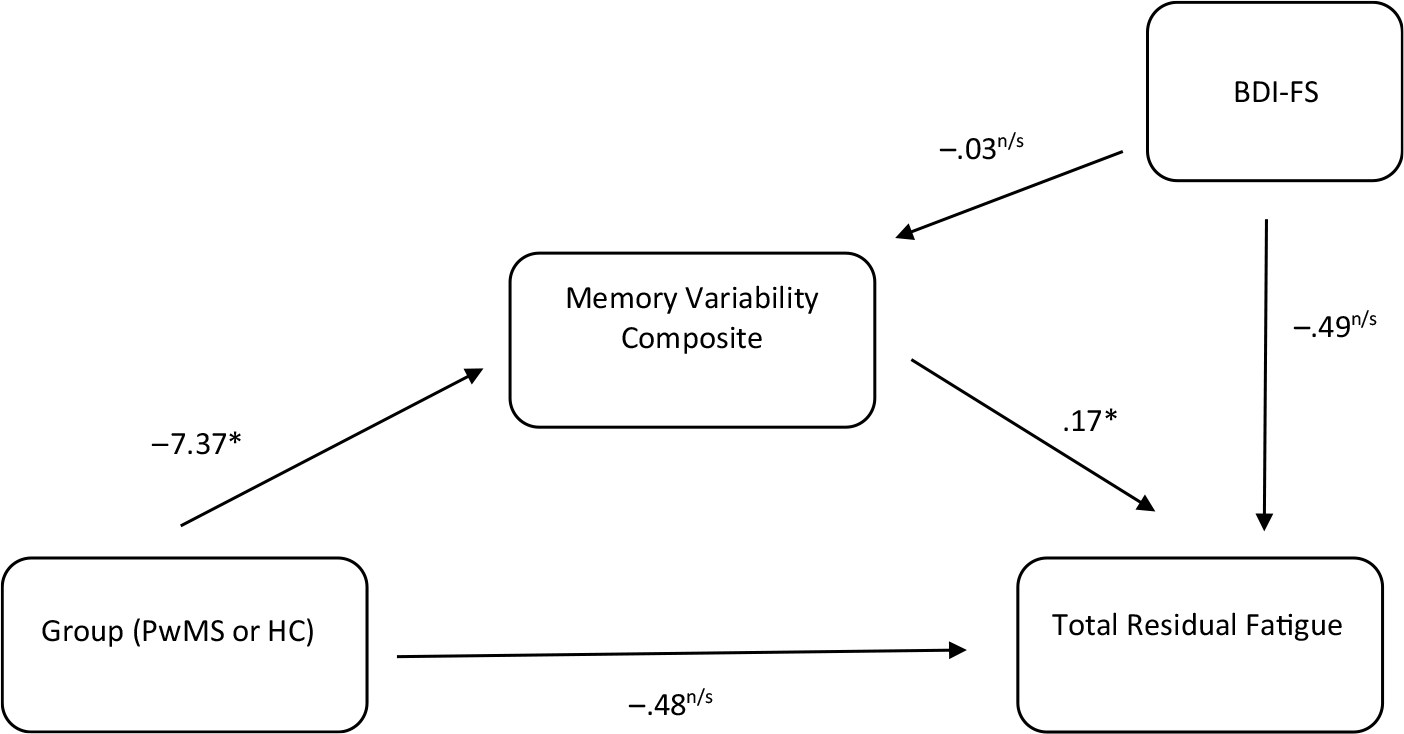
Fig. 2. Mediation model with memory variability composite as mediator and depression as covariate.
BDI-FS = Beck Depression Inventory-Fast Screen; HCs = Healthy Controls; PwMS = Persons with Multiple Sclerosis.
* = p < .05, n/s = p > .05 (not significant).
DISCUSSION
The present study was designed to evaluate differences between PwMS and HCs on IIV indices and examine the relationship between fatigue and cognitive variability between these groups. IIV was hypothesized to mediate the group differences expected in total fatigue. Prior research on fatigue in PwMS has been mixed, with some studies reporting an association between perceived fatigue and cognitive performance and other studies reporting no association. Potential explanations for these mixed findings include both the method of cognitive performance measurement and the conceptualization of the mechanism of fatiguability. Previous studies have measured cognitive performance as mean-level differences before and after an effortful cognitive task, for example, repeated performance on the PASAT or an n-back task. This paradigm, therefore, assumes that cognitive exertion in and of itself evokes fatiguability and that fatiguability may be the mechanism by which fatigue impairs performance. That is, if performance after a period of cognitive exertion is worse than before in PwMS, this paradigm assumes that the cognitive exertion was fatigue causing and that this explains that decline in performance. We sought to further explore the relationship between perceived fatigue and performance in PwMS by utilizing an alternative performance-based measure, IIV, and a mediation model with fatigue, rather than overall mean cognitive performance, as the outcome. Further in line with this previous work, we hypothesized that the direction of the relationship would be that IIV mediated total reported fatigue; that is, variable performance over time would be associated with higher self-report fatigue.
The current study explored the relationship between IIV and fatigue by utilizing a multidimensional scale to measure perceived fatigue, examining IIV as a measure of performance fatiguability, and using fatigue as the outcome of interest. Another benefit of the model used in the current study was that it accounted for total depression scores. As discussed above, depression is a common symptom in MS, is significantly correlated with fatigue, and has previously been shown to be a significant independent predictor, accounting for 31% of the variance, of MS fatigue (Strober & Arnett, Reference Strober and Arnett2005). Prior work has demonstrated that greater IIV may be associated with age-related changes (Sosnoff & Newell, Reference Sosnoff and Newell2006). Thus, to account for these differences, age was included in the mediation model by regressing age on total fatigue and then saving the unstandardized residuals (total residual fatigue) as the new outcome variable. The current mediation models allowed us to explore the effects of IIV on fatigue controlling for the contributing effects of depression on MS-related fatigue and accounting for the significant age difference.
As discussed above, depression is common in PwMS and can also have a measurable impact on cognitive functioning. In our sample, depression scores were significantly correlated with attention/processing speed IIV, but not memory IIV. A meta-analysis by McDermott and Ebmeier (Reference McDermott and Ebmeier2009) highlighted that prior research on depression and cognitive impairments in different domains has included inconsistent and contradictory findings. The meta-analysis revealed a significant correlation between depression severity and cognitive performance in domains of episodic memory, executive functioning, and processing speed, but not semantic or visuospatial memory (McDermott & Ebmeier, Reference McDermott and Ebmeier2009). Further, a review of processing speed, depression, fatigue, and cognition in PwMS found that processing speed is slower in MS depressed compared to MS nondepressed individuals (Arnett et al., Reference Arnett, Higginson, Voss, Bender, Wurst and Tippin1999). Taken together, attention and processing speed do seem to be slower in individuals with depression who do not have MS and in PwMS with depression. With these findings in mind, it may be that variability, rather than just mean differences in cognitive performance, highlights a unique influence of depression on this domain compared to memory.
Consistent with our hypotheses, results of two separate mediation analyses examining the mediating effect of IIV on total residual fatigue between PwMS and HC, after covarying for BDI-FS scores, revealed that IIV on both tests of attention/processing speed and memory mediated the relationship between patient status and total residual fatigue. This relationship was such that PwMS reported more total residual fatigue than HCs and that these group differences in total residual fatigue were reduced to being nonsignificant once accounting for IIV on both tests of attention/processing speed and memory. This indicates that variability in cognitive performance is associated with an increase in perceived fatigue. In short, patient status (MS or HC) leads to differences in IIV, which, in turn, results in differences in the perceived impact of fatigue. To further test the validity of our directionality hypothesis, we tested the reverse mediation, and total residual fatigue did not significantly mediate differences in IIV between the groups. That is, it does not seem that fatigue itself leads to the variability in performance over time.
There are several potential explanations for why IIV was found to be a significant mediator of the relationship between patient status and residual perceived fatigue. It may be the case that there are potential third variables, such as patterns of neural activation or attributions about fatigue symptoms, that contribute to both perceived fatigue and IIV. For example, individuals experiencing more IIV may perceive themselves as more fatigued. This aligns with models that have demonstrated that the way that patients interpret and respond to their symptoms or symptom attributions may increase the subjective experience of fatigue (Skerrett & Moss-Morris, Reference Skerrett and Moss-Morris2006; van Kessel & Moss-Morris, Reference van Kessel and Moss-Morris2006). A study by Skerrett and colleagues (2006) measured symptom interpretation and behavioral responses in PwMS. Results indicated that cognitive interpretations of their symptoms, including attributing a wide range of symptoms to their MS, were associated with fatigue over and above disease severity (EDSS), remission status, and mood (Skerrett & Moss-Morris, Reference Skerrett and Moss-Morris2006).
Alternately, brain activation of areas thought to underlie fatigue, may also be a variable that is related to both perceived fatigue and IIV. A study by DeLuca and colleagues (Reference DeLuca, Genova, Hillary and Wylie2008) examined the effects of sustained mental effort on patterns of brain activation between PwMS and HCs. In this study, cognitive fatigue (e.g., fatiguability) was defined as a relative increase in cerebral activation over time. Results indicated that increased activation was seen in PwMS compared to HCs and that this may be associated with the increased cognitive effort needed to adequately perform a task over a long period of time (DeLuca et al., Reference DeLuca, Genova, Hillary and Wylie2008). Further, this same group found that, when faced with increased cognitive demands, neural resources may be inefficiently activated in PwMS thus resulting in increased mental or cognitive fatigue (Chen et al., Reference Chen, Wylie, Sandroff, Dacosta-Aguayo, DeLuca and Genova2020). Additionally, research on the pathophysiology of MS and MS fatigue has identified the involvement in immune dysregulation of the cortico-striato-thalamo-cortical loop in the generation of MS fatigue (Chalah et al., Reference Chalah, Riachi, Ahdab, Créanget, Lefaucheur and Ayache2015). Demyelination and neurodegeneration of these brain regions may also underlie both perceived fatigue and lead to increased variability in performance.
These findings have important implications for understanding the impact of fatigue on the daily lives of PwMS and for the treatment of this fatigue. Variable performance, such as what might occur in the case of diurnal fatigue, may be reflective of fatiguability. This may be true of variable performance across a test battery, as was the case in this study, or variability in the performance of daily tasks throughout the workday that are reflective of difficulties commonly reported by PwMS. Fortunately, manualized treatments based on the cognitive behavioral therapy model of fatigue in MS have been created and a meta-analysis of these treatments demonstrated both positive short-term and long-term effects on fatigue (Induruwa, Constantinescu, & Gran, Reference Induruwa, Constantinescu and Gran2012; van den Akker et al., Reference van den Akker, Beckerman, Collette, Eijssen, Dekker and de Groot2016). Further, some disease modifying pharmacological treatments have demonstrated an impact on reducing the perception of fatigue in PwMS (Jongen et al., Reference Jongen, Lehnick, Sanders, Seeldrayers, Fredrikson, Andersson and Speck2010; Putzki, Yaldizli, Tettenborn, & Diener, Reference Putzki, Yaldizli, Tettenborn and Diener2009). More recently, exercise interventions have also been explored and progressive resistance training has been shown to be effective at reducing fatigue in MS (Akbar et al., Reference Akbar, Sandroff, Wylie, Strober, Smith, Goverover and Genova2020).
This study had several limitations. First, this study design was cross-sectional, therefore fatigue and IIV were measured on the same testing day. Future studies may explore IIV and perceived fatigue in a prospective and longitudinal design to understand the relationship between cognitive variability and fatigue over time. Additionally, the test battery administered in this study was comprised mostly of test indices known to be sensitive to difficulties experienced by PwMS. However, the battery was comprehensive and included tests covering several domains of functioning including immediate and delayed visual recall, immediate and delayed verbal recall, attention, and processing speed. Additionally, the study sample, both PwMS and HCs, was predominantly White and well educated. Therefore, these findings may not replicate in more heterogeneous populations and research on more diverse populations is warranted in the future.
Overall, this study demonstrated that IIV is an objective performance measure that is related to differences in fatiguability between PwMS and HCs. PwMS experience more variability across tests of attention/processing speed and memory and this experience of variable performance may increase the perception of fatigue. While traditional measures of performance have been variably linked to perceived fatigue, IIV may better capture the self-reported difficulties of individuals with MS-related fatigue. Another important conclusion from this study is that the relationship between MS and fatigue may not be direct, but rather may be the result of the mediating factor of cognitive variability.
FINANCIAL SUPPORT
This investigation was supported (in part) by a grant to the last author from the National Multiple Sclerosis Society (PP0978). The authors thank the many neurologists in the Pennsylvania region who contributed their time to verifying MS diagnoses and ratings and of course, for the MS participants in the project. The authors also thank Megan Smith, Fiona Barwick, Joseph Beeney, and Andrae Laws for their help with various aspects of the study.
CONFLICTS OF INTEREST
Dr. Bruce is a paid part-time employee of the National Hockey League. He is a grantee of the National Multiple Sclerosis Society, has served on the Novartis unbranded Speaker’s Bureau, and has received funding from Genzyme and Med-IQ. None of the other authors have conflicts of interest to report.








