Abstract
Purpose of Review
The aim of this study is to summarize anthropometric and advanced methods used to assess body composition in adults diagnosed with type 2 diabetes (T2D) or at risk for T2D that provide clinically relevant information about T2D disease-related complications or risk factors.
Recent Findings
Anthropometry is commonly used in clinical settings; however, provides unreliable estimates of fat mass, fat-free mass, and body fat distribution for metabolic health assessments compared to advanced techniques such as bioelectrical impedance analysis (BIA), dual-energy x-ray absorptiometry (DXA), computerized tomography (CT), and magnetic resonance imaging (MRI). Few studies report the clinical use of anthropometric and advanced body composition methods that identify T2D disease-related complications or T2D risk factors.
Summary
Anthropometry, BIA, DXA, CT, and MRI were used to estimate body adiposity and distribution, visceral and subcutaneous adipose tissue depots, and skeletal muscle mass. Review findings indicate that these methods were capable of identifying clinically relevant T2D disease-related complications such as sarcopenia and T2D risk factors such as obesity or regional adiposity. However, estimates were often sex and race/ethnicity specific warranting cross-validation of these methods in broader populations with T2D or risk for T2D prior to clinical implementation.

Similar content being viewed by others
References
American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S13. https://doi.org/10.2337/dc19-S002.
Centers for Disease Control and Prevention. National diabetes statistics report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020.
Lee SY, Gallagher D. Assessment methods in human body composition. Curr Opin Clin Nutr Metab Care. 2008;11(5):566–72. https://doi.org/10.1097/MCO.0b013e32830b5f23.
Teigen LM, Kuchnia AJ, Mourtzakis M, Earthman CP. The use of technology for estimating body composition(strengths and weaknesses of common modalities in a clinical setting [Formula: see text]). Nutr Clin Pract. 2017;32(1):20–9. https://doi.org/10.1177/0884533616676264.
Mooney SJ, Baecker A, Rundle AG. Comparison of anthropometric and body composition measures as predictors of components of the metabolic syndrome in a clinical setting. Obes Res Clin Pract. 2012;7(1):e55–66. https://doi.org/10.1016/j.orcp.2012.10.004.
Preis SR, Massaro JM, Robins SJ, Hoffmann U, Vasan RS, Irlbeck T, et al. Abdominal subcutaneous and visceral adipose tissue and insulin resistance in the Framingham heart study. Obesity (Silver Spring). 2010;18(11):2191–8. https://doi.org/10.1038/oby.2010.59.
Vanderwood KK, Kramer MK, Miller RG, Arena VC, Kriska AM. Evaluation of non-invasive screening measures to identify individuals with prediabetes. Diabetes Res Clin Pract. 2015;107(1):194–201. https://doi.org/10.1016/j.diabres.2014.06.003.
Battezzati A, Bertoli S, Testolin C, Testolin G. Body composition assessment: an indispensable tool for disease management. Acta Diabetol. 2003;40(1):s151–s3.
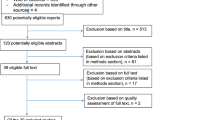
Moher D, Liberati A, Tetzlaff J, Altman DG, The Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Anbalagan VP, Venkataraman V, Pradeepa R, Deepa M, Anjana RM, Mohan V. The prevalence of Presarcopenia in Asian Indian individuals with and without type 2 diabetes. Diabetes Technol Ther. 2013;15(9):768–75. https://doi.org/10.1089/dia.2013.0068.
Anoop S, Misra A, Bhatt SP, Gulati S, Mahajan H, Prabakaran G. High plasma glucagon levels correlate with waist-to-hip ratio, suprailiac skinfold thickness, and deep subcutaneous abdominal and intraperitoneal adipose tissue depots in nonobese Asian Indian males with type 2 diabetes in North India. J Diabetes Res. 2017;2017:1–9. https://doi.org/10.1155/2017/2376016.
Buffa R, Saragat B, Succa V, Ruggiu R, Carboni L, Putzu PF, et al. Elderly subjects with type 2 diabetes show altered tissue electrical properties. Nutrition. 2013;29(1):132–7. https://doi.org/10.1016/j.nut.2012.05.007.
Chang Y, Guo X, Chen Y, Guo L, Li Z, Yu S, et al. A body shape index and body roundness index: two new body indices to identify diabetes mellitus among rural populations in northeast China. BMC Public Health. 2015;15:794. https://doi.org/10.1186/s12889-015-2150-2.
Mavros Y, Kay S, Anderberg KA, Baker MK, Wang Y, Zhao R, et al. Changes in insulin resistance and HbA1c are related to exercise-mediated changes in body composition in older adults with type 2 diabetes: interim outcomes from the GREAT2DO trial. Diabetes Care. 2013;36(8):2372–9. https://doi.org/10.2337/dc12-2196.
Park JS, Cho MH, Ahn CW, Kim KR, Huh KB. The association of insulin resistance and carotid atherosclerosis with thigh and calf circumference in patients with type 2 diabetes. Cardiovasc Diabetol. 2012;11:62. https://doi.org/10.1186/1475-2840-11-62.
Pramyothin P, Limpattanachart V, Dawilai S, Sarasak R, Sukaruttanawong C, Chaiyasoot K, et al. Fat-free mass, metabolically healthy obesity, and type 2 diabetes in severely obese asian adults. Endocr Pract. 2017;23(8):915–22. https://doi.org/10.4158/EP171792.OR.
Smits MM, Boyko EJ, Utzschneider KM, Leonetti DL, McNeely MJ, Suvag S, et al. Arm length is associated with type 2 diabetes mellitus in Japanese-Americans. Diabetologia. 2012;55(6):1679–84. https://doi.org/10.1007/s00125-012-2500-x.
Solanki JD, Makwana AH, Mehta HB, Gokhale PA, Shah CJ. Body composition in type 2 diabetes: change in quality and not just quantity that matters. Int J Prev Med. 2015;2015-December. https://doi.org/10.4103/2008-7802.172376.
Tajiri Y, Kato T, Nakayama H, Yamada K. Reduction of skeletal muscle, especially in Lower Limbs, in Japanese type 2 diabetic patients with Insulin resistance and cardiovascular risk factors. Metab Syndr Relat Disord. 2010;8(2):137–42. https://doi.org/10.1089/met.2009.0043.
Wanderley Rocha DR, Jorge AR, Braulio VB, Arbex AK, Marcadenti A. Visceral adiposity measurements, metabolic and inflammatory profi le in obese patients with and without type 2 diabetes mellitus: a crosssectional analysis. Curr Diabetes Rev. 2017;13(1):11–8. https://doi.org/10.2174/1573399812666151015115924.
Wium C, Eggesbø HB, Ueland T, Michelsen AE, Torjesen PA, Aukrust P, et al. Adipose tissue distribution in relation to insulin sensitivity and inflammation in Pakistani and Norwegian subjects with type 2 diabetes. Scand J Clin Lab Invest. 2014;74(8):700–7. https://doi.org/10.3109/00365513.2014.953571.
Alvim RDO, Mourao Jr CA, De Oliveira CM, Krieger JE, Mill JG, Pereira AC. Body mass index, waist circumference, body adiposity index, and risk for type 2 diabetes in two populations in Brazil: General and Amerindian. PLoS One. 2014;9(6). https://doi.org/10.1371/journal.pone.0100223.
Bianco A, Pomara F, Raccuglia M, Bellafiore M, Battaglia G, Filingeri D, et al. The relationship between type 2 diabetes family history, body composition and blood basal glycemia in sedentary people. Acta Diabetol. 2014;51(1):79–84. https://doi.org/10.1007/s00592-013-0502-x.
Biggs ML, Mukamal KJ, Luchsinger JA, Ix JH, Carnethon MR, Newman AB, et al. Association between adiposity in midlife and older age and risk of diabetes in older adults. JAMA J Am Med Assoc. 2010;303(24):2504–12. https://doi.org/10.1001/jama.2010.843.
Jowitt LM, Lu LW, Rush EC. Migrant Asian Indians in New Zealand; prediction of metabolic syndrome using body weights and measures. Asia Pac J Clin Nutr. 2014;23(3):385–93. https://doi.org/10.6133/apjcn.2014.23.3.06.
Kim CH, Kim HK, Kim EH, Bae SJ, Park JY. Association between changes in body composition and risk of developing type 2 diabetes in Koreans. Diabet Med. 2014;31(11):1393–8. https://doi.org/10.1111/dme.12527.
Kwon SS, Lee SG, Lee YH, Lim JB, Kim JH. Homeostasis model assessment of insulin resistance in a general adult population in Korea: additive association of sarcopenia and obesity with insulin resistance. Clin Endocrinol. 2017;86(1):44–51. https://doi.org/10.1111/cen.13233.
Lesser IA, Gasevic D, Lear SA. The effect of body fat distribution on ethnic differences in cardiometabolic risk factors of Chinese and Europeans. Appl Physiol Nutr Metab. 2013;38(7):701–6. https://doi.org/10.1139/apnm-2012-0125.
Liu X, Sun Q, Sun L, Zong G, Lu L, Liu G, et al. The development and validation of new equations for estimating body fat percentage among Chinese men and women. Br J Nutr. 2015;113(9):1365–72. https://doi.org/10.1017/S0007114515000616.
Srikanthan P, Karlamangla AS. Relative muscle mass is inversely associated with insulin resistance and prediabetes. Findings from the Third National Health and Nutrition Examination Survey. J Clin Endocrinol Metab. 2011;96(9):2898–903. https://doi.org/10.1210/jc.2011-0435.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 2012;7(7):e39504. https://doi.org/10.1371/journal.pone.0039504.
Thomas DM, Bredlau C, Bosy-Westphal A, Mueller M, Shen W, Gallagher D, et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity. 2013;21(11):2264–71.
Goodpaster BH, Krishnaswami S, Resnick H, Kelley DE, Haggerty C, Harris TB, et al. Association between regional adipose tissue distribution and both type 2 diabetes and impaired glucose tolerance in elderly men and women. Diabetes Care. 2003;26(2):372–9.
Janiszewski PM, Janssen I, Ross R. Does waist circumference predict diabetes and cardiovascular disease beyond commonly evaluated cardiometabolic risk factors? Diabetes Care. 2007;30(12):3105–9.
Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: a consensus statement from shaping America's health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am J Clin Nutr. 2007;85(5):1197–202.
Goss AM, Darnell BE, Brown MA, Oster RA, Gower BA. Longitudinal associations of the endocrine environment on fat partitioning in postmenopausal women. Obesity. 2012;20(5):939–44. https://doi.org/10.1038/oby.2011.362.
Toth M, Tchernof A, Sites C, Poehlman E. Effect of menopausal status on body composition and abdominal fat distribution. Int J Obes. 2000;24(2):226–31.
Jiang G, Zhang BB. Glucagon and regulation of glucose metabolism. Am J Physiol Endocrinol Metab. 2003;284(4):E671–E8. https://doi.org/10.1152/ajpendo.00492.2002.
Johnston LW, Harris SB, Retnakaran R, Gerstein HC, Zinman B, Hamilton J, et al. Short leg length, a marker of early childhood deprivation, is associated with metabolic disorders underlying type 2 diabetes: the PROMISE cohort study. Diabetes Care. 2013;36(11):3599–606.
Lee J-K, Wu C-K, Lin L-Y, Cheng C-L, Lin J-W, Hwang J-J, et al. Insulin resistance in the middle-aged women with “Tigerish Back and Bearish Waist”. Diabetes Res Clin Pract. 2010;90(3):e85–e7.
Snijder M, Visser M, Dekker J, Goodpaster BH, Harris TB, Kritchevsky SB, et al. Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The Health ABC Study. Diabetologia. 2005;48(2):301–8.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5. https://doi.org/10.1161/circulationaha.109.192644.
Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS One. 2010;5(5).
Bosy-Westphal A, Müller M. Identification of skeletal muscle mass depletion across age and BMI groups in health and disease—there is need for a unified definition. Int J Obes. 2015;39(3):379–86.
Kim KS, Park KS, Kim MJ, Kim SK, Cho YW, Park SW. Type 2 diabetes is associated with low muscle mass in older adults. Geriatr Gerontol Int. 2014;14:115–21.
Park SW, Goodpaster BH, Strotmeyer ES, de Rekeneire N, Harris TB, Schwartz AV, et al. Decreased muscle strength and quality in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes. 2006;55(6):1813–8.
Lund A, Bagger JI, Christensen M, Knop FK, Vilsbøll T. Glucagon and type 2 diabetes: the return of the alpha cell. Curr Diab Rep. 2014;14(12):555.
Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity. 2011;19(5):1083–9.
Herman WH, Smith PJ, Thompson TJ, Engelgau MM, Aubert RE. A new and simple questionnaire to Identify people at increased risk for undiagnosed diabetes. Diabetes Care. 1995;18(3):382–7. https://doi.org/10.2337/diacare.18.3.382.
McAuley KA, Williams SM, Mann JI, Walker RJ, Lewis-Barned NJ, Temple LA, et al. Diagnosing insulin resistance in the general population. Diabetes Care. 2001;24(3):460–4. https://doi.org/10.2337/diacare.24.3.460.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9. https://doi.org/10.1007/bf00280883.
Cornelis MC, Zaitlen N, Hu FB, Kraft P, Price AL. Genetic and environmental components of family history in type 2 diabetes. Hum Genet. 2015;134(2):259–67. https://doi.org/10.1007/s00439-014-1519-0.
Sharma AM, Chetty VT. Obesity, hypertension and insulin resistance. Acta Diabetol. 2005;42(Suppl 1):S3–8. https://doi.org/10.1007/s00592-005-0175-1.
Heymsfield S, Lohman T, Wang ZM, Going S. Human body composition. vol v. 918. Human Kinetics; 2005.
Alberti KG, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23(5):469–80. https://doi.org/10.1111/j.1464-5491.2006.01858.x.
Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V. Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis. 2008;18(5):388–95. https://doi.org/10.1016/j.numecd.2007.10.002.
Miyazaki Y, DeFronzo RA. Visceral fat dominant distribution in male type 2 diabetic patients is closely related to hepatic insulin resistance, irrespective of body type. Cardiovasc Diabetol. 2009;8(1):44.
Lim U, Ernst T, Buchthal S, Latch M, Albright CL, Wilkens LR, et al. Asian women have greater abdominal and visceral adiposity than Caucasian women with similar body mass index. Nutr Diabetes. 2011;1(5):e6–e.
Nyamdorj R, Qiao Q, Lam TH, Tuomilehto J, Ho SY, Pitkäniemi J, et al. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity (Silver Spring). 2008;16(7):1622–35. https://doi.org/10.1038/oby.2008.73.
Centers for Disease Control and Prevention: diabetes and Asian Americans. https://www.cdc.gov/diabetes/library/spotlights/diabetes-asian-americans.html (2019). Accessed May 10, 2020 2020.
Beechy L, Galpern J, Petrone A, Das SK. Assessment tools in obesity - psychological measures, diet, activity, and body composition. Physiol Behav. 2012;107(1):154–71. https://doi.org/10.1016/j.physbeh.2012.04.013.
Andreoli A, Garaci F, Cafarelli FP, Guglielmi G. Body composition in clinical practice. Eur J Radiol. 2016;85(8):1461–8.
Acknowledgements
NMS was supported by doctoral study funding through the University of Alabama Birmingham Graduate School and University of Alabama Birmingham School of Nursing Doctoral Scholarship.
Author information
Authors and Affiliations
Contributions
NS, study design; NS, data collection; NS, SM analysis; NS, SM manuscript preparation.
Corresponding author
Ethics declarations
Conflict of Interest
Nadia Markie Sneed and Shannon A. Morrison each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Obesity
Rights and permissions
About this article
Cite this article
Sneed, N.M., Morrison, S.A. Body Composition Methods in Adults with Type 2 Diabetes or at Risk for T2D: a Clinical Review. Curr Diab Rep 21, 14 (2021). https://doi.org/10.1007/s11892-021-01381-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s11892-021-01381-9