Abstract
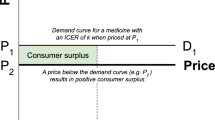
Pharmaceuticals are priced uniformly by convention, but vary in their degree of effectiveness for different disease indications. As more high-cost therapies have launched, the demand for alternative payment models (APMs) has been increasing in many advanced markets, despite their well-documented limitations and challenges to implementation. Among policy justifications for such contracts is the maximization of value given scarce resources. We show that while uniform pricing rules can handle variable effectiveness in efficient markets, market inefficiencies of other kinds create a role for different value-based pricing structures. We first present a stylized theoretical model of efficient interaction among drug manufacturers, payers, and beneficiaries. In this stylized setting, uniform pricing works well, even when treatment effects are variable. We then use this framework to define market failures that result in obstacles to uniform pricing. The market failures we identify include: (1) uncertainty of patient distribution, (2) asymmetric beliefs, (3) agency imperfection by payer, (4) agency imperfection by provider, and (5) patient behavior and treatment adherence. We then apply our insights to real-world examples of alternative payment models, and highlight challenges related to contract implementation.
Similar content being viewed by others
Notes
By uniform pricing, we refer to a lack of price variation occuring between most individual payers and drug manufacturers for the majority of products they trade with.
Our argument builds on the insight that price-bargaining can mitigate or eliminate monopoly losses in healthcare [18].
It is straightforward to show that all our results obtain with positive marginal costs.
The assumption of Nash-bargaining is not entirely innocuous. For example, Nash-bargaining fails to cover cases in which one or both players find it optimal to walk away from the negotiation without a deal [19]. More complex sequential bargaining models are needed to study such contexts.
Notice there are no copayments in this model. This is without loss of generality, as we can simply redefine \({P}_{i}\) as the price net of the copayment.
Note that a risk-neutral payer focuses only on expected consumer surplus and does not care independently about the actual realization of variance in the treatment effect. This is why the expression is independent of \({\epsilon }_{i}\).
If the drug were costly to manufacture, this production cost would appear within the left-hand side expression for profits.
It is not obvious that bargaining will always make consumers better off. While price-bargaining increases the total amount of gross consumer surplus, \(\sum_{i=1}^{{i}^{*}}n(i){G}_{i}\left({\Delta }_{i},{\sigma }_{i}^{2}\right)\), insurers with market power may extract these gains in the form of higher premiums. Governments may wish to return some surplus to consumers via taxes on firms and transfers to consumers. We leave the analysis of optimal redistribution policy to future work.
References
Goldman, D., Jena, A., Philipson, T., Sun, E.: Drug licenses: a new model for pharmaceutical pricing. Health Aff. 27(1), 122–129 (2008)
Carlson, J.J., Chen, S., Garrison, L.P., Jr.: Performance-based risk-sharing arrangements: an updated international review. Pharmacoeconomics 35(10), 1063–1072 (2017)
Drummond, M.: When do performance-based risk-sharing arrangements make sense? Eur. J. Health Econ. HEPAC Health Econ. Prevent. Care 16(6), 569–571 (2015)
Goldman D, Van Nuys K, Cheng W-H, Hlávka JP, Pani L, Chassang S, et al. (2018) A New Model for Pricing Drugs of Uncertain Efficacy. NEJM Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0035. Accessed 18 Aug 2020
Jean-Jacques Laffont, D.M.: The theory of incentives: the principal-agent model. Princeton University Press, Princeton (2002)
Conrad, D.A.: The theory of value-based payment incentives and their application to health care. Health Serv. Res. 50(Suppl 2), 2057–2089 (2015)
Economist Intelligence Unit. Value-based healthcare in Europe: Laying the foundation. London; 2016. https://eiuperspectives.economist.com/sites/default/files/ValuebasedhealthcareEurope_0.pdf. Accessed 18 Aug 2020
Vogler S, Haasis MA, Dedet G, Lam J, Pedersen HB (2018) Medicines Reimbursement Policies in Europe WHO Regional Office for Europe. https://www.euro.who.int/__data/assets/pdf_file/0011/376625/pharmaceutical-reimbursement-eng.pdf?ua=1. Accessed 18 Aug 2020
University of Washington. Performance-Based Risk Sharing Database Home: University of Washington; 2019 [Available from: https://depts.washington.edu/pbrs/index.php. Accessed 18 Aug 2020
Meyer H. As a cure for high drug prices, outcomes-based deals aren't delivering yet: Modern Healthcare; 2019. Available from: https://www.modernhealthcare.com/insurance/cure-high-drug-prices-outcomes-based-deals-arent-delivering-yet. Accessed March 23, 2019
Mannion, R., Davies, H.T.: Payment for performance in health care. BMJ 336(7639), 306–308 (2008)
Neumann, P.J., Chambers, J.D., Simon, F., Meckley, L.M.: Risk-sharing arrangements that link payment for drugs to health outcomes are proving hard to implement. Health Aff. (Millwood). 30(12), 2329–2337 (2011)
Sachs, R., Bagley, N., Lakdawalla, D.N.: Innovative contracting for pharmaceuticals and medicaid’s best-price rule. J. Health Polit. Policy Law 43(1), 5–18 (2018)
Chandra, A., Garthwaite, C.: The economics of indication-based drug pricing. N. Engl. J. Med. 377(2), 103–106 (2017)
Garber AM, Jones CI, Romer P, (eds) (2006)Insurance and incentives for medical innovation. Forum for Health Economics and Policy. De Gruyter. https://www.nber.org/system/files/working_papers/w12080/w12080.pdf. Accessed 18 Aug 2020
Pauly, M.V.: The questionable economic case for value-based drug pricing in market health systems. Value Health. 20(2), 278–282 (2017)
PhRMA. Delivering Results for Patients: The Value of Value-Based Contracts: PhRMA; 2018. Available from: http://phrma-docs.phrma.org/files/dmfile/PhRMA-Value-of-Value-Based-Contracts1.pdf. Accessed February 2018
Lakdawalla, D., Sood, N.: Innovation and the welfare effects of public drug insurance. J. Public. Econ. 93(3–4), 541–548 (2009)
Lakdawalla, D., Yin, W.: Insurers’ negotiating leverage and the external effects of medicare part D. Rev. Econ. Stat. 97(2), 314–331 (2015)
Lakdawalla D, Phelps C. Evaluation of medical technologies with uncertain benefits. National Bureau of Economic Research; 2019. Report No.: 0898–2937.
Lakdawalla, D., Sood, N.: Health insurance as a two-part pricing contract. J. Public Econ. 102, 1–12 (2013)
Lakdawalla, D.N.: Economics of the pharmaceutical industry. J. Econ. Lit. 56(2), 397–449 (2018)
Goldman, D., Smith, J.: Can patient self-management help explain the SES health gradient? Proc. Natl. Acad. Sci. 99(16), 10929–10934 (2002)
Goldman, D., Lakdawalla, D.: A theory of health disparities and medical technology. Contribut. Econ. Anal. Policy 4(1), 1 (2005)
Towse, A., Cole, A., Zamora, B.: The debate on indicationbased pricing in the U.S. and five major European Countries. OHE Consulting Ltd., London (2018)
Highlights of Prescribing Information: VIAGRA (sildenafil citrate), (2014). https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/20895s039s042lbl.pdf. Accessed 18 Aug 2020
FDA. Highlights of Prescribing Information: REVATIO (sildenafil): Pfizer; 2019 [Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/20895s039s042lbl.pdf. Accessed 18 Aug 2020
IBM Corporation. Redbook Online: Truven Health Analytics (IBM Watson Health); 2019 [Available from: https://www.micromedexsolutions.com/home/dispatch/ssl/true. Accessed 18 Aug 2020
Lien, S., Lowman, H.B.: Therapeutic anti-VEGF antibodies. Handb. Exp. Pharmacol. 181, 131–150 (2008)
Raftery, J., Clegg, A., Jones, J., Tan, S.C., Lotery, A.: Ranibizumab (Lucentis) versus bevacizumab (Avastin): modelling cost effectiveness. Br. J. Ophthalmol. 91(9), 1244–1246 (2007)
King R (2018) Trump administration moves to give Medicare drug plans more control over their offerings Washington Examiner. https://www.washingtonexaminer.com/policy/healthcare/trump-administration-moves-to-give-medicare-drug-plans-more-control-overtheir-offerings. Accessed 18 Aug 2020
Mestre-Ferrandiz, J., Towse, A., Dellamano, R., Pistollato, M.: Multi-indication pricing: pros cons and applicability to the UK seminar briefing. Office of Health Economics, London (2015)
Blumenthal, D.M., Goldman, D., Jena, A.B.: Tying reimbursement to outcomes is an ideal strategy for PCSK9 inhibitorstying reimbursement to outcomes is ideal for PCSK9 inhibitorstying reimbursement to outcomes is ideal for PCSK9 inhibitors. JAMA Cardiol. 2(10), 1063–1064 (2017)
Goldman, D., Philipson, T.J.: Integrated insurance design in the presence of multiple medical technologies. Am. Econ. Rev. 97(2), 427–432 (2007)
Blumenthal, D.M., Goldman, D.P., Jena, A.B.: Outcomes-based pricing as a tool to ensure access to novel but expensive biopharmaceuticalsoutcomes-based pricing to ensure access to novel biopharmaceuticals. Ann. Intern. Med. 166(3), 219–220 (2017)
Amgen And Harvard Pilgrim Agree To First Cardiovascular Outcomes-Based Refund Contract For Repatha® (Evolocumab) [press release]. 2017. https://www.amgen.com/newsroom/press-releases/2017/05/amgen-and-harvard-pilgrim-agree-to-first-cardiovascular-outcomesbasedrefund-contract-for-repatha-evolocumab.Accessed 18 Aug 2020
Cigna Reaches Pay-for-Performance Deals for PCSK9 Inhibitors [press release]. 2016. https://www.ajmc.com/view/cigna-reaches-pay-for-performance-deals-for-pcsk9-inhibitors. Accessed 18 Aug 2020
Pagliarulo N. Biogen inks outcomes-based contract for MS meds. BiopharmaDive. 2017. https://www.biopharmadive.com/news/biogen-outcomes-based-contract-prime-multiple-sclerosis/512422/. Accessed 18 Aug 2020
Shaw G. Abarca, Amgen Bet on PCSK9 Outcomes. Specialty Pharmacy Continuum. 2018. https://www.specialtypharmacycontinuum.com/Policy/Article/10-17/Abarca-Amgen-Bet-on-PCSK9-Outcomes/48440. Accessed 18 Aug 2020
PRNewswire. Prime Therapeutics prefers both cholesterol lowering drugs Praluent® and Repatha® on its national drug list. 2015. https://www.prnewswire.com/news-releases/prime-therapeutics-prefers-both-cholesterol-lowering-drugs-praluent-and-repatha-on-itsnational-drug-list-300196593.html. Accessed 18 Aug 2020
Kitamura, M., Koch, J.: When cancer treatments fail. Italy Wants Money Back, Bloomberg (2016)
Colasante W. What Risks Do Annuity Pricing Models Present To Cell & Gene Therapy Developers? 2019 [Available from: https://www.cellandgene.com/doc/what-risks-do-annuity-pricing-models-present-to-cell-gene-therapy-developers-0001. Accessed 18 Aug 2020
WHO. Medicines reimbursement policies in Europe WHO Collaborating Centre for Pharmaceutical Pricing and Reimbursement Policies, editor: WHO Regional Office for Europe; 2018.
Slocomb T, Werner M. New Payment And Financing Models For Curative Regenerative Medicines: Informa Pharma Intelligence; 2017. Available from: https://invivo.pharmaintelligence.informa.com/IV005132/New-Payment-And-Financing-Models-For-Curative-Regenerative-Medicines. Accessed July 24, 2017
Bhattacharya, J., Chandra, A., Chernew, M., Goldman, D., Jena, A., Lakdawalla, D., Philipson, T.: Best of both worlds: uniting universal coverage and personal choice in health care. American Enterprise Institute, Washington D.C. (2013)
Jommi, C., Armeni, P., Costa, F., Bertolani, A., Otto, M.: Implementation of value-based pricing for medicines. Clin. Ther. 42(1), 15–24 (2020)
Mattke, S., Liu, H., Hoch, E., Mulcahy, A.W.: Avoiding the tragedy of the commons in health care: policy options for covering high-cost cures. RAND Health Quart. 6(2), 1 (2017)
Goldman D. What Health Care Can Learn from Netflix: LinkedIn; 2013 [Available from: https://www.linkedin.com/pulse/20130527215225-22738440-what-health-care-can-learn-from-netflix/. Accessed 18 Aug 2020
Alcorn T. Louisiana’s Deal for Hepatitis C Drugs May Serve as Model. Wall Street Journal. 2019. https://www.wsj.com/articles/louisianas-deal-for-hepatitis-c-drugs-may-serve-as-model-11568347621. Accessed 18 Aug 2020
Chen, A., Lakdawalla, D.N.: Healing the poor: the influence of patient socioeconomic status on physician supply responses. J. Health Econ. 64, 43–54 (2019)
Hussey, P.S., Ridgely, M.S., Rosenthal, M.B.: The PROMETHEUS bundled payment experiment: slow start shows problems in implementing new payment models. Health Aff. 30(11), 2116–2124 (2011)
NEJM Catalyst. What Is Value-Based Healthcare 2017 [Available from: https://catalyst.nejm.org/what-is-value-based-healthcare/.
Ward, J.C., Levit, L.A., Page, R.D., Hennessy, J.E., Cox, J.V., Kamin, D.Y., et al.: Impact on oncology practices of including drug costs in bundled payments. J. Oncol. Pract. 14(5), e259–e268 (2018)
UnitedHealthcare. UnitedHealthcare Expands Use of Bundled Payments with Medicare Advantage Health Care Providers Minnetonka, Minn. 2019 [Available from: https://www.unitedhealthgroup.com/newsroom/2019/2019-04-10-uhc-bundled-payments-medicare-advantage.html. Accessed 18 Aug 2020
Robinson, J.C.: Value-based physician payment in oncology: public and private insurer initiatives. Milbank. Q. 95(1), 184–203 (2017)
Struijs JN. How Bundled Health Care Payments Are Working in the Netherlands 2015 [Available from: https://hbr.org/2015/10/how-bundled-health-care-payments-are-working-in-the-netherlands. Accessed 18 Aug 2020
Eaddy, M.T., Cook, C.L., O’Day, K., Burch, S.P., Cantrell, C.R.: How patient cost-sharing trends affect adherence and outcomes: a literature review. Pharm. Ther. 37(1), 45–55 (2012)
Pagliarulo N. Can value-based deals work if patients don't take the drug? BiopharmaDive. 2017. https://www.biopharmadive.com/news/adherence-value-based-deal-payment-patient-outcomes/442449/. Accessed 18 Aug 2020
Dayer, L., Heldenbrand, S., Anderson, P., Gubbins, P.O., Martin, B.C.: Smartphone medication adherence apps: potential benefits to patients and providers. J. Am. Pharm. Assoc. 53(2), 172–181 (2013)
Papanicolas I, Woskie LR, Jha A. Health Care Spending in the United States and Other High-Income Countries: The Commonwealth Fund; 2018 [updated March 13, 2018. Available from: https://www.commonwealthfund.org/publications/journal-article/2018/mar/health-care-spending-united-states-and-other-high-income.
Kesselheim, A.S., Avorn, J., Sarpatwari, A.: The high cost of prescription drugs in the united states: origins and prospects for reform. JAMA 316(8), 858–871 (2016)
Bach, P.B.: Indication-specific pricing for cancer drugs. JAMA 312(16), 1629–1630 (2014)
Claxton, K., Briggs, A., Buxton, M.J., Culyer, A.J., McCabe, C., Walker, S., et al.: Value based pricing for NHS drugs: an opportunity not to be missed? BMJ 336(7638), 251–254 (2008)
Pearson, S.D., Dreitlein, W.B., Henshall, C., Towse, A.: Indication-specific pricing of pharmaceuticals in the US healthcare system. J. Compar. Eff. Res. 6(5), 397–404 (2017)
Garner, S., Rintoul, A., Hill, S.R.: Value-based pricing: l’enfant terrible? Pharmacoeconomics 36(1), 5–6 (2018)
Funding
This study was supported by a grant from NIH under Award Number R01AG062277. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Hlávka does not report any conflicts of interest. Mr. Yu reports personal fees from Boston Health Economics. Dr. Darius Lakdawalla has received consulting fees from Amgen, Genentech, GRAIL, Novartis, Otsuka, and Pfizer. Darius Lakdawalla also holds equity in Precision Medicine Group, which provides consulting services to firms in the pharmaceutical and biotechnology industries. Dr. Goldman reports honoraria from Amgen, The Aspen Institute, and Celgene. Until March 2020, Dr. Goldman served as a scientific advisor to Precision Medicine Group, and owns < 1% equity in the company. Until November 2019, Dr. Goldman served on the scientific advisory board of ACADIA Pharmaceuticals. He currently serves on the scientific advisory board of GRAIL.
Ethical approval
This paper does not require institutional or ethical committee approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hlávka, J.P., Yu, J.C., Goldman, D.P. et al. The economics of alternative payment models for pharmaceuticals. Eur J Health Econ 22, 559–569 (2021). https://doi.org/10.1007/s10198-021-01274-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-021-01274-4
Keywords
- Optimal Pricing
- Price Discrimination
- Pharmacoeconomics
- Health Insurance
- Health Care Financing
- Deadweight Loss