Abstract
Background
Stroke is a devastating complication of cardiovascular surgeries, and the risk is particularly high for those requiring cardiopulmonary bypass (CPB). Embolic particles generated during the unclamping of the aortic cross-clamp may enter the cerebral circulation, lodging in small vessels. External manual compression of the carotid arteries is a non-invasive technique that has been proposed for cerebral protection during CPB procedures but is not widely deployed.
Methods
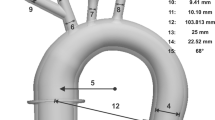
The aim of this study is to assess the potential for cerebral emboli reduction with carotid compression using an in vitro model. Experiments were performed with a glass aortic arch model in a mock cardiovascular circuit. Small fluorescent particles were released into the circulation with and without carotid compression, and the particles visualized in the aortic midplane. The number of particles in the aorta and arch branch vessels were counted from the images before, during and following the release of carotid compression for durations of 10, 15 and 20 s. A gamma variate function was fit to the data to describe the bolus dynamics.
Results
Carotid compression for 10 s reduces the number of embolic articles entering the carotid arteries by over 75%. A compression duration of 15–20 s does not result in greater particle reduction than one of 10 s.
Conclusion
Brief compression of the common carotid arteries during cardiovascular interventions has the potential to dramatically reduce the number of cerebral emboli and should be investigated further.






Similar content being viewed by others
References
Avrahami, I., et al. Numerical investigation of a novel aortic cannula aimed at reducing cerebral embolism during cardiovascular bypass surgery. J. Biomech. 46(2):354–361, 2013. https://doi.org/10.1016/j.jbiomech.2012.11.004.
Barbut, D., et al. Cerebral emboli detected during bypass surgery are associated with clamp removal. Stroke 25:2398–2403, 1994.
Barbut, D., et al. Determination of size of aortic emboli and embolic load during coronary artery bypass grafting. Ann. Thorac. Surg. 63(5):1262–1267, 1997.
Baufreton, C. Role of surgical factors in strokes after cardiac surgery. Arch. Cardiovasc. Dis. 103(5):326–332, 2010.
Büsen, M., T. A. S. Kaufmann, M. Neidlin, U. Steinseifer, and S. J. Sonntag. In vitro flow investigations in the aortic arch during cardiopulmonary bypass with stereo-PIV. J. Biomech. 48(10):2005–2011, 2015. https://doi.org/10.1016/j.jbiomech.2015.03.030.
Chan, A. A., and S. J. Nelson. Simplified gamma-variate fitting of perfusion curves. IEEE 2(2):1067–1070, 2004.
Doenst, T., M. A. Borger, R. D. Weisel, T. M. Yau, M. Maganti, and V. Rao. Relation between aortic cross-clamp time and mortality—Not as straightforward as expected. Eur. J. Cardio-Thorac. Surg. 33:660–665, 2008. https://doi.org/10.1016/j.ejcts.2008.01.001.
Gallo, M., A. Putzu, M. Conti, G. Pedrazzini, S. Demertzis, and E. Ferrari. Embolic protection devices for transcatheter aortic valve replacement. Eur. J. Cardio-thoracic Surg. 53(6):1118–1126, 2018. https://doi.org/10.1093/ejcts/ezx457.
Gasparovic, H., M. Borojevic, B. Malojcic, K. Gasparovic, and B. Biocina. Single aortic clamping in coronary artery bypass surgery reduces cerebral embolism and improves neurocognitive outcomes. Vasc. Med. 2013. https://doi.org/10.1177/1358863x13502699.
Gerriets, T., et al. Cardiac surgery Protecting the brain from gaseous and solid micro-emboli during coronary artery bypass grafting : a randomized controlled trial. Thorac. Cardiovasc. Surg. 2010. https://doi.org/10.1093/eurheartj/ehp178.
Gold, J. P., et al. Improvement of outcomes after coronary artery bypass. A randomized trial comparing intraoperative high versus low mean arterial pressure. J. Thorac. Cardiovasc. Surg. 110(5):1302–1314, 1995.
Hillebrand, J., A. Rouhollahpour, A. Zierer, A. Moritz, and S. Martens. Digital carotid compression: A simple method to reduce solid cerebral emboli during cardiac surgery. J. Cardiothorac. Vasc. Anesth. 30(2):304–308, 2016. https://doi.org/10.1053/j.jvca.2015.11.017.
Ling, I., Z. Moyedi, K. Wong, W. P. Dembitsky, R. M. Adamson, and K. D. May-Newman, Flow dynamics in the aortic root of the LVAD-assisted heart. In Biomedical Engineering Society Annual Meeting, 2013, p. P-Thurs-A-101.
Lisle, T. C., et al. Timing of stroke after cardiopulmonary bypass determines mortality. Ann. Thorac. Surg. 85(5):1556–1563, 2008. https://doi.org/10.1016/j.athoracsur.2008.02.035.Timing.
Lou, S., B. Ji, J. Liu, K. Yu, and C. Long. Generation, detection and prevention of gaseous microemboli during cardiopulmonary bypass procedure. Int. J. Artif. Organs 34:1039–1051, 2011. https://doi.org/10.5301/ijao.5000010.
Markus, H. S., and M. M. Brown. Differentiation between different pathological cerebral embolic materials using transcranial Doppler in an in vitro model. Stroke 24(1):1–5, 1993.
May-Newman, K., J. H. Omens, R. S. Pavelec, and A. D. McCulloch. Three-dimensional transmural mechanical interaction between the coronary vasculature and passive myocardium in the dog. Circ. Res. 74:6, 1994.
Menon, P. G., N. Teslovich, C. Y. Chen, A. Undar, and K. Pekkan. Characterization of neonatal aortic cannula jet flow regimes for improved cardiopulmonary bypass. J. Biomech. 46(2):362–372, 2013. https://doi.org/10.1016/j.jbiomech.2012.10.029.
Moyedi, Z. Pulsatile Flow in the Aorta of the LVAD Supported Heart Studied Using Particle Image Velocimetry. San Diego: San Diego State University, 2014.
Pekkan, K., et al. Neonatal aortic arch hemodynamics and perfusion during cardiopulmonary bypass. J. Biomech. Eng. 130(6):10–13, 2008. https://doi.org/10.1115/1.2978988.
Schwartz, J. P., M. Bakhos, A. Patel, S. Botkin, and S. Neragi-miandoab. Repair of aortic arch and the impact of cross-clamping time, New York Heart Association stage, circulatory arrest time, and age on operative outcome. Interactive Cardiovasc. Thorac. Surg. 7:425–429, 2008. https://doi.org/10.1510/icvts.2007.164871.
Skjelland, M., et al. Cerebral microembolization during off-pump coronary artery bypass surgery with the Symmetry aortic connector. Cardiopulm. Support Physiol. 130(6):1581–1585, 2005. https://doi.org/10.1016/j.jtcvs.2005.08.015.
Sorteberg, A., W. Sorteberg, S. J. Bakke, K. F. Lindegaard, M. Boysen, and H. Nornes. Varying impact of common carotid artery digital compression and internal carotid artery balloon test occlusion on cerebral hemodynamics. Head Neck 20(8):687–694, 1998. https://doi.org/10.1002/(sici)1097-0347(199812)20:8<687::aid-hed5>3.0.co;2-1.
Sungurtekin, H., W. Plochl, and J. Cook. Relationship between cardiopulmonary bypass rate and cerebral embolization in dogs. Anesthesiology 92:1387–1393, 1999.
Van Mieghem, N. M., and A. Van Der Lugt. How embolism proof is the embrella embolic deflector system? JACC Cardiovasc. Interv. 7(10):1156–1158, 2014. https://doi.org/10.1016/j.jcin.2014.07.007.
Acknowledgments
The work was performed in the Cardiovascular Bioengineering Laboratory at San Diego State University with internal funding sources. There are no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Amy L. Throckmorton oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Isingoma, P., Moon, J. & May-Newman, K. Manual Carotid Compression is a Viable Alternative for Reduction of Cerebral Microemboli. Cardiovasc Eng Tech 12, 353–360 (2021). https://doi.org/10.1007/s13239-021-00528-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-021-00528-9