Abstract
Purpose of Review
The COVID-19 pandemic has provided us with a unique opportunity to experiment with telehealth and evaluate its benefits and limitations. This review discusses the impact of telehealth on multiple sclerosis (MS) care and research in adults and children.
Recent Findings
Telehealth visits for MS patients have been shown to reduce missed workdays and costs for patients. Brief telephone-based counseling may be associated with better adherence to disease-modifying therapy, although results of multiple home-based tele-rehabilitation for people with MS have been equivocal. Overall, patients and providers have reported high levels of satisfactions with telehealth. Several remote disability measures and numerous other technological tools have emerged for use in remote MS research and care. Major challenges of telehealth include limitations to performing a complete neurologic exam and disparities in access to telehealth amongst vulnerable populations with limited access to virtual platforms.
Summary
Following the rapid expansion of telehealth during the pandemic, it is highly likely that we will continue to embrace the benefits of this valuable tool. Future directions for improving telehealth should include more evidence-based research on the diagnostic accuracy in neuroimmunology and reducing disparities in the access to telehealth.
Similar content being viewed by others
Introduction
Telehealth is the use of virtual technology-based platforms to deliver health information and medical care, and it includes several distinct types of services [1]. Synchronous telehealth is defined as the delivery of health information in real-time that allows for a live discussion conducted remotely. In asynchronous telehealth, a patient or physician collects and sends medical information such as medical history, images, and lab reports to a specialist for medical expertise. Novel technologies, including biosensors and mobile devices, have also expanded the scope of telehealth in recent years.
Before the onset of the COVID-19 pandemic, telehealth in neurology had been driven primarily by the lack of access to adult and child neurologic consultations for certain geographic parts of the country [2]. Teleneurology has been used for a variety of neurologic disorders, including cerebrovascular disorders, neuro-oncological disorders, and multiple sclerosis (MS) [3]. A retrospective study in 2002 compared outpatient neurology telehealth encounters with two cohorts of face-to-face neurology evaluations, and with neurology outpatients seen by general physicians [4]. The study found that management of patients from the telehealth group was also not significantly different from those seen face-to-face by neurologists in hospital clinics, but the telehealth patients had significantly fewer investigations and follow-ups than those patients managed by general physicians [4]. This study showed that the management of outpatient neurology patients by neurologists using telehealth is similar to that by neurologists in face-to-face visits [4].
While the COVID-19 pandemic has accelerated our integration of telehealth platforms in all areas of neurologic care, this article will primarily address the impact of telehealth on MS care and research in adults and children.
Use of Telehealth in MS Clinical Care
HIPPA-Compliant Platforms
Although the US Department of Health and Human Services allows for HIPAA flexibility for good faith use of telemedicine during the COVID-19 pandemic, a HIPAA-compliant platform is recommended to avoid potential complications after the pandemic has ended. The American Academy of Neurology (AAN) does not endorse specific vendors of telemedicine platforms. There are now numerous HIPAA-compliant platforms available, and some of which have been integrated into electronic health records, but the integration is not necessary to conduct a telehealth visit [5, 6].
Remote Neurologic Examination for Adults and Children
One of the major challenges of telehealth is the limitation in the ability to complete a remote neurologic exam, especially when evaluating sensation, reflexes, tone, motor strength, and optic nerve function [7]. In March 2020, the AAN released a guide for implementing telemedicine and included a detailed description of performing the adult neurologic exam via virtual platforms [5]. Some platforms offer technical focusing options that allow examiners to evaluate pupils and palate. Most of the remaining neurologic exam requires an additional person with the patient to help the remote examiner. The neurologist may inspect for subtle signs of weakness by checking for drift and asking the patient to perform functional assessments such as standing up with arms crossed and crouch then stand (sit to stand). The neurologist may then use an assistant present with the patient to assess individual roots and branches of the brachial and lumbar plexus. During the sensory exam, an assistant may be instructed to evaluate for sensory differences between left and right, differences between dermatomes, and evaluate for extinction with double simultaneous stimulation. Examination of reflexes may be difficult without a skilled examiner, but an assistant present with the patient may be instructed to look for the plantar response [5].
In May 2020, the Child Neurology Society published a guide for the pediatric neurologic examination via telemedicine [8]. Included in the guide are instructions for the exam based on three different age groups: infant (< 12 months), toddler (12–36 months), and child (3–10 years). This guide emphasizes that pediatric neurologic exams via telemedicine are mostly observational and therefore require ongoing and careful observation of the patient throughout the visit [8]. The authors also recommended having a shiny or visually interesting toy and a noise-making toy available for all ages [8]. Additional tips for performing the cranial nerve exam include assessing for extraocular eye movements by having the patient fixate on the camera while the caregiver rotates the patient’s head from side to side. For the evaluation of reflexes in young patients, the examiner may instruct the caregiver to assess for Moro [8].
Use of Telehealth in Adult MS Care
In 2019 prior to the COVID-19 pandemic, the Telemedicine Work Group of the AAN reported that telemedicine visits for MS patients reduced missed workdays by 65%, saved travel by an average of 258 km, and reduced costs of lodging by 17% [9]. A randomized controlled pilot trial found that brief telephone-based counseling was associated with better adherence to disease-modifying therapy (DMT) amongst veterans with MS [10]. Another longitudinal cohort study among veterans with MS found that 87.5% of participants reported positive experiences with home telehealth monitor [11].
Results of multiple home-based tele-rehabilitation for people with MS have shown equivocal results [12••]. Several prospective studies found that telephone- or web-based interventions were feasible and effective for reducing fatigue and increasing physical activity in MS patients [13,14,15,16,17]. A pilot study of a web-based module designed for self-management of MS showed significant improvement in the timed 25-foot walk (T25FW) and the 6-min walk, but a larger randomized trial of the same platform did not show a significant difference in the T25FW [12••]. A randomized, controlled study found no significant difference in the T25FW following 12 weeks of internet-based physical therapy compared to usual care in people with MS, and the same study also found that participants who were less familiar with the internet required more technological support and showed decreased login rates over the course of the program [12••, 18]. Another randomized, controlled tele-rehabilitation study found decreased compliance over time with no improvements in health-related quality of life after 6 months despite noting significant improvements in muscles strength and sports activity [12••, 19].
Overall, patients and providers have reported high levels of satisfactions with telehealth across multiple specialties [20,21,22,23]. A prospective study of 36 MS patients found that 97% of participants would recommend telemedicine visits to others, and 94% of participants rated it easy to connect via telemedicine [22]. Participants in this study provided qualitative comments that expressed appreciation for the convenience of telemedicine visits and similarity to in-clinic visits [22]. Another study included 36 patients with movement disorders who completed telepsychiatry visits for management of psychiatric symptoms [23]. Ninety-five percent of the participants were very satisfied with the care, and 76% of participants reported they were very satisfied with the technical quality [23]. A third study evaluated the implementation of in-hospital teleneurology consultations conducted using handheld tablet technology and found that community physicians were able to successfully manage 87% of patients in partnership with neurologists at a community-based hospital, and 91% of community physicians were satisfied or somewhat satisfied with the overall service [20]. In specialties beyond neurology, a controlled study included patients who were referred for dermatology consultation, and patients were examined in-person, by video, and by store-and-forward methods [21]. While both dermatologists and patients preferred in-person examinations, satisfaction with telehealth remained high. Patients in this study were equally divided with preference for store-and-forward and live video interactions [21].
Telemedicine in Child Neurology and Pediatric MS Care
The use of telemedicine in general child neurology has also been widely implemented following the COVID-19 pandemic. A study that analyzed over 2,500 child neurology telehealth encounters necessitated by the COVID-19 pandemic found no differences in patient’s age and major ICD10 codes before and after the transition to telehealth [24]. Ninety-three percent of the encounters were considered satisfactory by clinicians [24]. Eighty-nine percent of follow-up encounters included telemedicine as a component, and face-to-face assessments were recommended following 5% of encounters [24]. While technical difficulties were reported in 40% of encounters, patients or caregivers reported interest in using telemedicine for future care in 86% of the encounters [24].
While studies on the use of telehealth for children with MS are limited, one double-blind randomized controlled pilot study evaluated the efficacy of a home-based computerized program for retraining attention in 16 pediatric-onset MS patients and 20 attention-deficit hyperactivity disorder patients who failed at least two out of four attention tests on a neuropsychological battery [25]. The participants were randomized to either specific computerized training based on the Attention Processing Training program or non-specific computerized training that consisted of a series of non-specific exercises. In participants with pediatric-onset MS, exposure to specific computerized training was associated with significantly improved cognitive impairment index and improved attention, concentration, and visuospatial memory performances [25].
Applying Telehealth to MS Clinical Research
Clinical research in MS depends on the ability to assess for disability. The Expanded Disability Status Scale (EDSS) has been the standard disability assessment tool in both clinical practice and research studies. A proof of principle study evaluated disability using telemedicine in people with mild to moderate MS by comparing EDSS scores obtained using a standardized in-person EDSS evaluation to a tele-EDSS score [26•]. The tele-EDSS evaluation required an “in-home neuro kit” that included standard neurologic examination tools such as a vision card, cotton swab, tuning fork, and alcohol swab. The authors found that in 88% of evaluations, tele-EDSS and standardized EDSS scores were within 1 point, which was similar to reported in-person interrater differences [26•]. Another study showed good agreement between remote and face-to-face evaluators when obtaining disability scores; however, the remote evaluation required an in-person examiner available to guide the patient [9, 27•, 28]. A third study showed modest agreement between conventional and telemedicine formats for EDSS score ≤ 4.0 and good agreement for EDSS scores ≥ 4.5 [9]. Other investigators have proposed using more non-conventional forms of data such as those from biosensors to substitute for the EDSS score [12••, 29•]. For example, authors have found that lower step counts measured by an accelerometer correlated with higher EDSS disability score and captured variability in walking masked by standard disability scales [12••, 27•, 30].
While remote disability assessments studied prior to the COVID-19 pandemic suggest that telemedicine may be used as part of follow-up assessments for MS clinical care and research, the additional requirements such as the in-home neuro kit, assistant examiners, and biosensory data integration have imposed challenges for the immediate implementation of remote EDSS evaluations during the pandemic [26•, 29•]. A different approach to disability assessment has focused on patient-reported outcome measures (PROMs) that would be exclusively reported online. One example of PROM is the Patient Determined Disease Steps (PDDS) available online [29•]. The PDDS has been found to strongly correlate to EDSS scores and has been validated in multiple languages [29•, 31].
Investigators in other specialties are also searching for ways to facilitate ongoing research during the COVID-19 pandemic [32, 33]. Remote measures of upper limb function and ambulation have been associated with functional recovery following rehabilitation in stroke care; remote monitoring may help to predict falls in patients with Parkinson’s disease [33]. Researchers in geriatrics have continued studies during the pandemic by offering electronic consents, implementing remote assessments by using alternative tools and scales that can be administered by phone or virtual visits, and proactively partnering with the institutional IRBs to develop language to easily report such minor protocol deviations [32].
Technologic Devices for MS Telehealth
As a supplement to the synchronous video visits, numerous other technological tools have emerged over the past two decades that have become relevant to the management of MS. Wearable devices include biosensors that convert biological signal into electrical signal and allow easy accessibility with potential for asynchronous remote monitoring. The most common biosensors are accelerometers and gyroscopes.
Accelerometers are worn on a patient’s hip, arm, or thigh and can measure steps and activity patterns that include time spent in different intensity of activities. Many commercial devices such as smart phones and smart watches have incorporated accelerometers. Tracking the daily step count in a person with MS has been shown to reliably measure free-living walking behavior [34, 35]. In MS patients with EDSS between 0.0 and 6.5, moderate to good correlations have been shown between daily step count and EDSS [34, 36]. Lower step counts may also capture variability in walking masked by standard disability scales [12••, 27•, 30].
Gyroscopes measure angular velocity and record orientation, changes in posture, and the acceleration and angle of force for movements, allowing a more objective measurement of patients’ stability and balance. Studies have shown good-to-excellent reliability of gyroscope measurements during Time Up and Go tests for people with MS [36]. Gyroscopes may also help distinguish gait patterns and tremors associated with the severity of disease and have been used to detect subtle differences in the 6-min walk test and the Timed Up and Go tests [36].
New composite disability metrics such as the self-administered Multiple Sclerosis Performance Test (MSPT) now include gyroscope and accelerometer data. The MSPT was developed to be used on the iPad computer platform to resemble the Multiple Sclerosis Functional Composite. The MSPT includes four neuroperformance subtests: Contrast sensitivity test (CST) to assess vision, manual dexterity test (MDT) to assess upper extremity motor function, walking speed test (WST) to assess lower extremity motor function, and processing speed test (PST) to assess processing speed and cognition. A study found that the CST, MDT, and WST were reliable, valid, and sensitive measures of MS outcomes in 30 MS patients and 30 healthy controls [37]. An earlier study compared the PST with the Symbol Digit Modalities Test (SDMT) and found the PST had excellent test-retest reliability, was highly correlated with the SDMT, and was slightly more sensitive than the SDMT in differentiating patients with MS from healthy controls [38].
Other biosensors, such as force sensors and eye trackers, have also been studied in people with MS. Grip force sensors measure grip, load force, and movement speed during simple tasks and may provide an objective measure of upper extremity motor function. Studies have shown that increased peak grip force and longer time lag before peak grip force correlate with EDSS scores in MS patients with mild disability [36]. Eye trackers use near-infrared light to capture the cornea and pupil and detect subtle efferent vision abnormalities, including diplopia, oscillopsia, and fixation abnormalities that may not be easily detectable on the standard neurologic exam but may impair the ability to read or lead to dizziness and falls [36]. Biosensors designed to evaluate autonomic dysfunction include sensors measuring heart rate, core temperature, and other vital signs; however, these sensors still require further investigations before they could be incorporated into standard assessments for disability in people with MS [39].
Wearable devices and biosensors continue to evolve as an asynchronous form of telehealth. Although these technologies have been more useful in the research arena in recent years, they may become increasing incorporated into clinical applications due to the social distancing demands of the COVID-19 pandemic.
Challenges of Telehealth
While synchronous telehealth visits offer numerous benefits such as reduced missed workdays, cost, travel, and exposure to COVID-19, several major challenges remain.
One limitation of synchronous telehealth is the challenge of performing a complete neurologic exam. Although the AAN and CNS have released formal guidelines for remote neurologic exams as described in earlier sections of this article, there is still no reliable way for the remote neurologist to evaluate tone, sensation, reflexes, and fundoscopy via telehealth [7]. This limitation poses a concern for potential misdiagnosis and mismanagement. For example, an abnormal neurologic exam in the setting of a non-concerning history would prompt neurologists to obtain neuroimaging; similarly, the inability to perform a full neurologic exam may theoretically lead to the overuse of and over-dependence on neuroimaging and other diagnostic tests instead of relying at least partially on the neurologic exam to provide reassurance. A randomized study of non-acute headache patients found no difference between telehealth and traditional consultations in long-term treatment efficacy over a 12-month period as measured by change in the Headache Impact Test-6 and pain intensity [40]. Importantly, the presence of secondary headache within 12 months after consultation was assessed as the primary safety endpoint. One secondary headache was identified in the 200 patients randomized to telehealth, and the number of telehealth consultations needed to miss one secondary headache was 20,200 [40]. Overall, however, research in this arena has been limited, but the pandemic will likely provide the opportunity for more objective evaluations of the diagnostic accuracy of telehealth.
Within MS care, several opportunities exist to capitalize on the unique benefits of telehealth for clinical care while avoiding some of its current limitations. Following the initial diagnosis and evaluation of an MS patient, a dedicated follow-up visit is usually necessary to discuss disease-modifying treatment (DMT) options and for symptom management. Similarly, follow-up visits to review the results of crucial diagnostic evaluations such as neuroimaging or lumbar punctures are often planned to offer physicians ample time to address patients’ questions and concerns. During these discussions, a full neurologic exam is usually not essential unless the patient has new concerns. Telehealth visits offer families ease and flexibility while avoiding the potential risks of misdiagnosis and mismanagement.
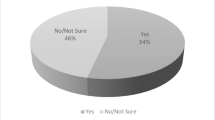
Another limitation of telehealth in its current form is the equity of access. A study examining telehealth and outpatient subspecialty visits amongst pediatric Medicaid patients in 2014 found that although children in rural communities were more likely to use telehealth, early telemedicine policies and implementation did not close disparities in rates of subspecialty visits by geographic and sociodemographic characteristics and may actually exacerbate or perpetuate disparities for urban and minority patients [41]. Disparities to the access of healthcare have been highlighted following the rapid expansion of telehealth due to the COVID-19 pandemic [42, 43]. Primary care clinicians at UCSF compared a 2-week period before telemedicine implementation to a 2-week period after implementation, and the proportion of telehealth visits increased from 3 to 80% of the total weekly visit; however, the proportion of visits with population at risk for limited digital access had decreased significantly [43]. Proportion of visits with patients ≥ 65 years of age decreased from 41 to 35% (p = 0.002), of non-English language preference from 14 to 7% (p < 0.001), insured by Medicare from 43 to 22% (p < 0.001), and insured by Medicaid from 17 to 10% (p < 0.001) [43]. Patients identifying as non-Hispanic White and other showed increased proportion of visits, whereas all other groups, including Black/African American, Latinx, and Asian/Pacific Islander, represented a smaller proportion of visits (p = 0.006) [43]. The authors of this study identified several strategies to overcome barriers for telehealth access. Training and teaching specific populations on how to use tools for telemedicine have been shown to be effective, and UCSF has recruited health community members such as research coordinators and medical students to contact all patients ≥ 65 years of age to guide them through setting up and connecting to virtual platform applications [43]. Other interventions include creating video tutorials in different languages on how to set up telehealth visits and offering telephone visits if video visits are not possible [43]. Broadband internet access is also an essential determinant in the use of telehealth [43, 44]. Expanding low-cost or free broadband Internet access and ensuring pay parity for both telephone and video visits are crucial to addressing the access barriers faced by many vulnerable patient groups [42, 43, 45].
Conclusion
The COVID-19 pandemic has provided us with a unique opportunity to experiment with telehealth and evaluate its benefits and limitations for both synchronous forms—more useful in clinical care—and asynchronous forms, which are more applicable for research. Following the rapid expansion of telehealth during the pandemic, it is highly likely that we will continue to embrace the benefits of this valuable tool, especially given the chronic healthcare needs of people with multiple sclerosis and other neuroimmunologic disorders. Future directions for improving telehealth should include more evidence-based research on the diagnostic accuracy in neuroimmunology, especially amongst the pediatric population, as well as reducing disparities in the access to telehealth.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mechanic OJ, Persaud Y, Kimball AB. Telehealth systems. Treasure Island (FL): StatPearls; 2020.
Kang PB, Bale JF Jr, Mintz M, Joshi SM, Gilbert DL, Radabaugh C, et al. The child neurology clinical workforce in 2015: report of the AAP/CNS Joint Taskforce. Neurology. 2016;87(13):1384–92.
Chirra M, Marsili L, Wattley L, Sokol LL, Keeling E, Maule S, et al. Telemedicine in neurological disorders: opportunities and challenges. Telemed J E Health. 2019;25(7):541–50.
Chua R, Craig J, Esmonde T, Wootton R, Patterson V. Telemedicine for new neurological outpatients: putting a randomized controlled trial in the context of everyday practice. J Telemed Telecare. 2002;8(5):270–3.
Neurology AAo. Telemedicine and COVID-19 implementation guide: American Academy of Neurology; 2020 [updated April 10 2020. Available from: https://www.aan.com/siteassets/home-page/tools-and-resources/practicing-neurologist--administrators/telemedicine-and-remote-care/20-telemedicine-and-covid19-v103.pdf.
Association TM. Telemedicine vendor options 2020 [updated 2020. Available from: https://www.texmed.org/uploadedFiles/Current/2016_Practice_Help/Health_Information_Technology/Telemedicine/Telemedicine%20Vendor%20Options.pdf.
Lo MD, Gospe SM Jr. Telemedicine and child neurology. J Child Neurol. 2019;34(1):22–6.
Annette Grefe DH, Charuta Joshi, Sucheta Joshi, Mark Mintz, Mickey Segal, and Asim Shahid. Pediatric neurological examination via telemedicine Child Neurology Society 2020 [updated May 2020. Available from: https://www.childneurologysociety.org/docs/default-source/2020-cns-/pediatric-neuro-exam-via-telemedicine---may-2020-final.pdf?sfvrsn=8e2165b8_2.
Hatcher-Martin JM, Adams JL, Anderson ER, Bove R, Burrus TM, Chehrenama M, et al. Telemedicine in neurology: telemedicine work group of the American Academy of Neurology update. Neurology. 2020;94(1):30–8.
Turner AP, Sloan AP, Kivlahan DR, Haselkorn JK. Telephone counseling and home telehealth monitoring to improve medication adherence: results of a pilot trial among individuals with multiple sclerosis. Rehabil Psychol. 2014;59(2):136–46.
Turner AP, Wallin MT, Sloan A, Maloni H, Kane R, Martz L, et al. Clinical management of multiple sclerosis through home telehealth monitoring: results of a pilot project. Int J MS Care. 2013;15(1):8–14.
•• Yeroushalmi S, Maloni H, Costello K, Wallin MT. Telemedicine and multiple sclerosis: a comprehensive literature review. J Telemed Telecare. 2020;26(7-8):400–13 The authors provided a comprehensive and systematic review of the medical literature from 2000 to 2018 that included 28 studies to investigate the types of telemedicine being utilized and overall outcomes for people with MS.
D'Hooghe M, Van Gassen G, Kos D, Bouquiaux O, Cambron M, Decoo D, et al. Improving fatigue in multiple sclerosis by smartphone-supported energy management: the MS TeleCoach feasibility study. Mult Scler Relat Disord. 2018;22:90–6.
Dlugonski D, Motl RW, Mohr DC, Sandroff BM. Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: sustainability and secondary outcomes. Psychol Health Med. 2012;17(6):636–51.
Finlayson M, Preissner K, Cho C, Plow M. Randomized trial of a teleconference-delivered fatigue management program for people with multiple sclerosis. Mult Scler. 2011;17(9):1130–40.
Moss-Morris R, McCrone P, Yardley L, van Kessel K, Wills G, Dennison L. A pilot randomised controlled trial of an Internet-based cognitive behavioural therapy self-management programme (MS Invigor8) for multiple sclerosis fatigue. Behav Res Ther. 2012;50(6):415–21.
Turner AP, Hartoonian N, Sloan AP, Benich M, Kivlahan DR, Hughes C, et al. Improving fatigue and depression in individuals with multiple sclerosis using telephone-administered physical activity counseling. J Consult Clin Psychol. 2016;84(4):297–309.
Paul L, Coulter EH, Miller L, McFadyen A, Dorfman J, Mattison PG. Web-based physiotherapy for people moderately affected with multiple sclerosis; quantitative and qualitative data from a randomized, controlled pilot study. Clin Rehabil. 2014;28(9):924–35.
Tallner A, Streber R, Hentschke C, Morgott M, Geidl W, Maurer M, et al. Internet-supported physical exercise training for persons with multiple sclerosis-a randomised, controlled study. Int J Mol Sci. 2016;17(10):1667.
Harper K, McLeod M, Brown SK, Wilson G, Turchan M, Gittings EM, et al. Teleneurology service provided via tablet technology: 3-year outcomes and physician satisfaction. Rural Remote Health. 2019;19(1):4743.
Marchell R, Locatis C, Burgess G, Maisiak R, Liu WL, Ackerman M. Patient and provider satisfaction with teledermatology. Telemed J E Health. 2017;23(8):684–90.
Robb JF, Hyland MH, Goodman AD. Comparison of telemedicine versus in-person visits for persons with multiple sclerosis: a randomized crossover study of feasibility, cost, and satisfaction. Mult Scler Relat Disord. 2019;36:101258.
Seritan AL, Heiry M, Iosif AM, Dodge M, Ostrem JL. Telepsychiatry for patients with movement disorders: a feasibility and patient satisfaction study. J Clin Mov Disord. 2019;6:1.
Rametta SC, Fridinger SE, Gonzalez AK, Xian J, Galer PD, Kaufman M, et al. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. 2020;95(9):e1257–e66.
Simone M, Viterbo RG, Margari L, Iaffaldano P. Computer-assisted rehabilitation of attention in pediatric multiple sclerosis and ADHD patients: a pilot trial. BMC Neurol. 2018;18(1):82.
• Bove R, Bevan C, Crabtree E, Zhao C, Gomez R, Garcha P, et al. Toward a low-cost, in-home, telemedicine-enabled assessment of disability in multiple sclerosis. Mult Scler. 2019;25(11):1526–34 The authors showed that a telemedicine-based MS disability examination is feasible in mild to moderate MS without an aide at the patient’s location.
• Block VJ, Bove R, Zhao C, Garcha P, Graves J, Romeo AR, et al. Association of continuous assessment of step count by remote monitoring with disability progression among adults with multiple sclerosis. JAMA Netw Open. 2019;2(3):e190570 The authors showed that a decreasing average daily step count was associated with standard ambulatory measure worsening provided support for using the average daily step count as an outcome measure in MS.
Kane RL, Bever CT, Ehrmantraut M, Forte A, Culpepper WJ, Wallin MT. Teleneurology in patients with multiple sclerosis: EDSS ratings derived remotely and from hands-on examination. J Telemed Telecare. 2008;14(4):190–4.
• Moccia M, Lanzillo R, Brescia Morra V, Bonavita S, Tedeschi G, Leocani L, et al. Assessing disability and relapses in multiple sclerosis on tele-neurology. Neurol Sci. 2020;41(6):1369–71 The authors reviewed available tools for MS telehealth and suggested a battery for assessing MS disability and relapses that can be delivered remotely and in multiple languages.
Block VJ, Lizee A, Crabtree-Hartman E, Bevan CJ, Graves JS, Bove R, et al. Continuous daily assessment of multiple sclerosis disability using remote step count monitoring. J Neurol. 2017;264(2):316–26.
Lavorgna L, Sparaco M, Esposito S, Motl RW, Gallo A, Bisecco A, et al. Validity and reproducibility of the Italian version of the patient determined disease steps scale in people with multiple sclerosis. Mult Scler Relat Disord. 2017;18:173–6.
Nicol GE, Piccirillo JF, Mulsant BH, Lenze EJ. Action at a distance: geriatric research during a pandemic. J Am Geriatr Soc. 2020;68(5):922–5.
Block VA, Pitsch E, Tahir P, Cree BA, Allen DD, Gelfand JM. Remote physical activity monitoring in neurological disease: a systematic review. PLoS One. 2016;11(4):e0154335.
Lavorgna L, Brigo F, Moccia M, Leocani L, Lanzillo R, Clerico M, et al. e-Health and multiple sclerosis: an update. Mult Scler. 2018;24(13):1657–64.
Motl RW, Pilutti L, Sandroff BM, Dlugonski D, Sosnoff JJ, Pula JH. Accelerometry as a measure of walking behavior in multiple sclerosis. Acta Neurol Scand. 2013;127(6):384–90.
Yousef A, Jonzzon S, Suleiman L, Arjona J, Graves JS. Biosensing in multiple sclerosis. Expert Rev Med Devices. 2017;14(11):901–12.
Rao SM, Galioto R, Sokolowski M, McGinley M, Freiburger J, Weber M, et al. Multiple sclerosis performance test: validation of self-administered neuroperformance modules. Eur J Neurol. 2020;27(5):878–86.
Rao SM, Losinski G, Mourany L, Schindler D, Mamone B, Reece C, et al. Processing speed test: validation of a self-administered, iPad((R))-based tool for screening cognitive dysfunction in a clinic setting. Mult Scler. 2017;23(14):1929–37.
Bradshaw MJ, Farrow S, Motl RW, Chitnis T. Wearable biosensors to monitor disability in multiple sclerosis. Neurol Clin Pract. 2017;7(4):354–62.
Muller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017;89(2):153–62.
Ray KN, Mehrotra A, Yabes JG, Kahn JM. Telemedicine and outpatient subspecialty visits among pediatric Medicaid beneficiaries. Acad Pediatr. 2020;20(5):642–51.
Hirko KA, Kerver JM, Ford S, Szafranski C, Beckett J, Kitchen C, et al. Telehealth in response to the COVID-19 pandemic: implications for rural health disparities. J Am Med Inform Assoc. 2020;27(11):1816–8.
Nouri S, Khong EC, Lyles CR, Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal Innov Care Deliv. 2020.
Rodriguez JALS, Lyles CR, Samal L. Association between patient portal use and broadband access: a national evaluation. J Gen Intern Med. 2020;35:3719–20.
Lyles C. Tackling digital inequality in the tech capital of the world. San Francisco Examiner. 2019 May;7.
Acknowledgements
The editors would like to thank Dr. John Brust for taking the time to review this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Xinran Maria Xiang declares no potential conflicts of interest. Jacqueline Bernard has served as a Consultant to MedLink Neurology.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Demyelinating Disorders
Rights and permissions
About this article
Cite this article
Xiang, X.M., Bernard, J. Telehealth in Multiple Sclerosis Clinical Care and Research. Curr Neurol Neurosci Rep 21, 14 (2021). https://doi.org/10.1007/s11910-021-01103-4
Accepted:
Published:
DOI: https://doi.org/10.1007/s11910-021-01103-4