Abstract
Men who have sex with men (MSM) are disproportionately affected by anal cancer, predominantly caused by high-risk (HR) human papillomavirus (HPV) infection. Currently, the nonavalent HPV vaccine provides coverage against nine HPV genotypes, including seven HR-HPV genotypes. Here, we characterize anal HR-HPV genotype distribution and associated risk factors in MSM from Toronto, Canada recruited between September 2010 and June 2012. Wilcoxon–Mann–Whitney test was used for continuous variables, Chi-square test was performed for categorical variables, and a multivariable model using logistic regression was created to assess for correlates of anal HR-HPV infection. A total of 442 MSM were recruited, with a median age of 45 (IQR 38–50) and an overall HPV prevalence of 82%. The prevalence of any HR-HPV infection was 65.3% and 50.7% in the HIV-positive and HIV-negative MSM, respectively. No participant tested positive for all genotypes covered by the nonavalent vaccine. HIV status (aOR 1.806; 95% CI 1.159–2.816), smoking (aOR 2.176; 95% CI 1.285–3.685) and the number of lifetime sexual partners (aOR 2.466; 95% CI 1.092–5.567) were independent risk factors for anal HR-HPV infection. Our findings will be useful to inform HPV vaccine rollout and HPV prevention strategies in Canadian MSM.
Similar content being viewed by others
Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) globally1. Of the more than 200 HPV genotypes that have been identified to date, over 50 genotypes primarily target the transformation zone between the squamous and columnar epithelia of mucosal surfaces such as the ano-rectum2,3. Importantly, while most mucosal HPV infections have no symptoms and are spontaneously cleared by the host immune system, some cause persistent infection and can eventually lead to cancer of the affected area4. Mucosal HPV genotypes are classified as either low-risk (LR) or high-risk (HR), with LR genotypes sometimes causing benign warts but not cancerous lesions, while HR genotypes have oncogenic potential5.
Anal cancer is an important consequence of HPV infection, with a meta-analysis finding over 80% of anal cancers to be linked to HPV infection, most strongly with HPV-16 at a rate of 82% in HIV-negative and 67% in HIV-positive men6,7. The incidence of anal cancer has been increasing in high-income countries8, with particularly rapid increases in men who have sex with men (MSM) where the incidence is 40/100,000 in HIV-negative MSM and over 100/100,000 in HIV-positive MSM9, in comparison to a background rate of 2/100,000 in the general population10. Current treatment options for anal dysplasia include mechanical or chemical ablative techniques, but there are high recurrence rates regardless of clinical approach and it has not been formally demonstrated that any of these approaches prevents the subsequent development of cancer11,12. Moreover, recent evidence shows that the clearance of anal dysplasia in the absence of any intervention occurs at a fairly high rate of 22/100 person-years, further adding to the complexity of this clinical issue13.
Although clinical trials are underway to optimize screening and treatment protocols for anal HPV-associated disease, prophylactic vaccination is an important and validated method of HPV prevention. There are currently three commercially available vaccines in Canada, two of which are recommended for MSM. The quadrivalent Gardasil vaccine, which targets HPV 6, 11, 16 and 18, was shown to be effective in reducing the incidence of anal precancer14. More recently the nonavalent Gardasil-9 vaccine, which adds protection against HPV 31, 33, 45, 52 and 58, has also shown safety and efficacy in MSM15. Notably, while the HPV vaccine is recommended up to the age of 45 for everyone in the United States, the indications in Canada are only up to the age of 26 for men16. Nonetheless, Canada’s National Advisory Committee on Immunization (NACI) still recommends that HPV vaccine be strongly considered in all MSM and people living with HIV regardless of their age17,18. As such, these guidelines lead to uncertainty and inconsistency in practices around HPV vaccine recommendations19. Furthermore, men generally have lower acquired immunity in response to natural HPV infection as compared to women20,21, and unlike cervical HPV infection which peaks shortly after sexual debut, anal HPV infection in men are found at relatively constant rates across the lifespan22,23. Taken together, these findings suggest that older MSM may also benefit from the HPV vaccine.
Given this rationale for HPV vaccination among all MSM including older MSM, understanding the prevalence and risk factors for HR-HPV infection in this population may better inform vaccination policy, research priorities and future clinical implementation strategies. The current study expands on a prior analysis of HPV infection in MSM from Toronto24 to characterize genotype distribution of anal HPV infection, and risk factors associated with HR-HPV infection among HIV-positive and HIV-negative older MSM.
Results
Participant characteristics
A total of 442 MSM were enrolled in our study, consisting of 294 HIV-positive MSM and 148 HIV-negative MSM. The median age for the overall population was 45 (IQR 38–50), with the majority being white (74.1%). A third (31.0%) of the population had never smoked cigarettes, while 34.3% reported as former smokers and 34.7% as current smokers. Complete data including socio-demographic characteristics were available for 429 participants, of whom 267 (62.2%) tested positive for at least one high-risk (HR) HPV genotype versus 162 (37.8%) who tested negative for any HR-HPV genotype (Table 1). Demographic characteristics were broadly similar in the HR-HPV-positive and HR-HPV-negative groups.
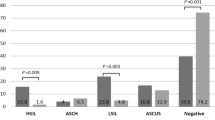
Anal HPV prevalence by HIV status
Overall, any HPV infection and any HR-HPV infection were both commonly found in our study cohort of 442 MSM regardless of HIV status, with overall prevalence of 82.4% and 60.4%, respectively. However, MSM living with HIV were disproportionately impacted by HR-HPV infection in a number of different ways: HIV infection was associated with an increased prevalence of any HPV infection (88.4%, 95% CI [84.1–91.6%] vs 77.9% [70.5–83.9%]; p = 0.0043), any HR-HPV infection (65.3% [59.7–70.5%] vs 50.7% [42.7–58.6%]; p = 0.0013) and infection by multiple HR-HPV genotypes (29.2% [24.3–34.8%] vs 13.8% [9.1–20.3%]; p = 0.0004). Notably, HIV-positive MSM had an increased prevalence of both HPV-16 (33.7% [28.5–39.3%] vs 23.0% [16.9–30.4%]; p = 0.016) and HPV-18 (16.3% [12.5–21.0%] vs 8.1% [4.7–13.6%]; p = 0.015), as well as the low-risk HPV genotype HPV-11 that is typically associated with anogenital warts (19.7% [15.5–24.7%] vs 10.3% [6.3–16.3%]; p = 0.014; Fig. 1). Several other HR-HPV genotypes were relatively common in our cohort, regardless of HIV status. Importantly, only three participants (two living with HIV, and one not) were infected with all four HPV genotypes that are targeted by the quadrivalent vaccine (HPV-6, 11, 16 and 18) while no participant was infected by all nine genotypes targeted by the nonavalent vaccine (HPV-6, 11, 16, 18, 31, 33, 45, 52 and 58).
Factors associated with anal HR-HPV infection
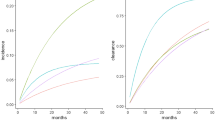
Using a priori inclusion of HIV serostatus, lifetime number of sexual partners and smoking and change-in-estimate methods to construct the multivariable model, the following variables were retained in the final multivariable analysis (Table 2): HIV-positive status; a history of receptive anal intercourse (RAI) in the previous six months; current smoking; ≥ 50 lifetime sexual partners; ≥ 5 sexual partners in the previous six months; a history of crystal methamphetamine, ecstasy or MDMA use in the previous six months, and a history of drug use within two hours of sexual activity. In the multivariable analysis, HIV infection (adjusted odds ratio [aOR] 1.806, p = 0.009), current smoking (aOR 2.176, p = 0.004) and ≥ 50 lifetime sexual partners (aOR 2.466, p = 0.030) remained significantly associated with anal HR-HPV infection (Table 2).
We then constructed multivariable models stratified by HIV status. Among HIV-positive MSM (Table 2), current smoking (aOR 2.113, p = 0.027) was the only factor that remained significantly associated with anal HR-HPV infection. Among HIV-negative MSM (Table 2), reporting ≥ 50 lifetime sexual partners (aOR 3.809, p = 0.042) was the only factor significantly associated with anal HR-HPV infection.
Factors associated with any HPV infection and infection by multiple HPV genotypes
A similar multivariable analytic approach was then used to assess associations of any anal HPV infection and infection by multiple anal HPV genotypes among Toronto MSM.
In a combined cohort analysis that included both HIV infected and uninfected participants, HIV serostatus was the only variable significantly associated with any anal HPV infection (aOR 2.260; 95% CI 1.261–4.049; p = 0.006; Table 3). Limiting this analysis to HIV infected participants, self-reported RAI in the last 6 months was the only variable associated with HPV infection (aOR 2.683; 95% CI 1.045–6.890; p = 0.040); none of the variables remained significantly associated with any HPV infection among HIV-negative participants.
The prevalence of anal infection by multiple HPV genotypes among HIV-infected participants was 67.3% (191/284), compared to 40.7% (59/145) among their HIV-uninfected peers. In the combined cohort analysis, HIV status (aOR 2.809; 95% CI 1.789–4.412; p = 0.000007), RAI in the last 6 months (aOR 1.899; 95% CI 1.183–3.051; p = 0.008), current smoking (aOR 1.805; 95% CI 1.056–3.086; p = 0.031) and reporting ≥ 50 lifetime sexual partners (aOR 3.295; 95% 1.378–7.881; p = 0.007) all remained significantly associated with anal infection by multiple HPV genotypes (Table 4). Within the HIV-positive population, only RAI in the past 6 months remained associated with anal infection by multiple HPV genotypes (aOR 2.438; 95% CI 1.323–4.494; p = 0.004); among HIV uninfected participants only current smoking remained associated (aOR 2.612; 95% CI 1.018–6.701; p = 0.046). The most common genotypes detected in participants with anal infection by multiple HPV genotypes were HPV16 (41.9%), HPV11 (26.7%) and HPV18 (23.6%) among HIV-infected participants, while HPV16 (40.7%), HPV6 (23.7%) and HPV70 (18.6%) predominated in HIV-uninfected participants.
Discussion
This cross-sectional study of MSM living in Toronto, Canada was performed to characterize the anal HPV genotype distribution and risk factors for anal HR-HPV infection and found a high prevalence of both HPV and HR-HPV infection in the anal canal. In particular, the rates of HR-HPV infection in both HIV-positive and HIV-negative MSM were broadly similar to rates seen in other countries such as Spain, Italy and China25,26,27. Factors significantly associated with HR-HPV infection were HIV serostatus, cigarette smoking and a higher number of lifetime sexual partners. After stratifying for HIV status, lifetime sexual partners only remained significant among HIV-negative MSM. Interestingly, although over 60% of participants tested positive for at least one HR-HPV genotype included in the nonavalent vaccine, none of the study participants were infected by all nine genotypes. Even when we narrowed down our definition of “vaccine types” to those genotypes included in the quadrivalent vaccine, only three individuals tested positive for all four vaccine genotypes. While the cross-sectional nature of our study precludes us from determining whether prior HPV infections and subsequent clearance occurred in our cohort, it is important to note that even a prior, natural infection may not necessarily confer immunity. As such, our findings imply that older (median age = 45 years) MSM may still obtain benefit from HPV vaccination.
The risk factors for HR-HPV anal infection identified in our study are consistent with findings from other groups. For instance, cigarette smoking has consistently been associated with anal HPV infection28,29, and we also found it to be a risk factor associated with both having any anal HR-HPV infection and having multiple HPV infections. We also found having ≥ 50 lifetime sexual partners to be a risk factor for HR-HPV infection only in HIV-negative MSM, which is in line with data from other groups. For example, a group in China found that sexual behavior such as condomless RAI was associated with anal HPV infection in HIV-negative but not HIV-positive MSM30. Likewise, researchers from the Netherlands found that having a higher number of lifetime male sex partners was significantly associated with anal HR-HPV infection in HIV-negative but not HIV-positive MSM31. Similarly, studies that largely (> 96%) included HIV-negative MSM have observed that number of recent sexual partners is associated with anal HPV infection32,33 or that a high number of lifetime sexual partners and recent RAI are associated with the persistence of anal HR-HPV infection34. The reasons for the role of sexual activity in increasing anal HR-HPV infection risk in HIV-negative but not HIV-positive MSM are unclear and merit further investigation.
We decided to focus on the risk factors associated with anal HR-HPV genotypes, and not solely with anal HPV16 infection, given relatively high prevalence of several other HR-HPV genotypes. According to a recent meta-analysis, the prevalence of the following anal HR-HPV infections among HIV-positive MSM was above 5% and even exceeding 15% in some cases: HPV18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68. Similar trends with a generally lower prevalence were seen in HIV-negative MSM with rates above 5% for the following anal HR-HPV genotypes: HPV18, 39, 51 and 5235. Indeed, while HPV16 was the most frequently found anal HR-HPV genotype in both HIV-positive and HIV-negative MSM in our cohort, prevalence of other HR-HPV genotypes targeted by the nonavalent vaccine were found at high rates up to 16.3% and 8.1% in HIV-positive and HIV-negative MSM, respectively. Moreover, while others have reported a significantly higher prevalence of HPV31, 52 and 58 in HIV-positive compared to HIV-negative MSM36, they were found at comparable rates in our cohort; our results highlight the need to broaden our scope of understanding to include all HR-HPV genotypes in MSM regardless of HIV status.
The cross-sectional design of our study is a limitation since it precludes us from making definitive conclusions about the time course of HPV infection detected in our cohort. Notably, several groups have reported a high incidence of HR-HPV infection in HIV-positive MSM with a history of recent sexual activity37,38. However, given that recent sexual activity including having a new sexual partner or RAI in the past 6 months did not associate with anal HPV infection, it is likely that the majority of HPV infection from this study reflected a persistent, rather than an incident, infection. This is an important distinction as persistence of HR-HPV infection is a better surrogate marker of anal pre-cancer and/or cancer than the incidence/prevalence, which may reflect a transient infection. Data regarding participants’ HPV vaccination history were not available. However, at the time this study was performed, the HPV vaccine was not yet covered in Ontario for boys or gay men under the age of 26 years. Therefore, although it is unlikely that many of our participants would have received the HPV vaccine, it is not possible for us to completely discount the potential effect of HPV vaccination on the prevalence of HPV genotypes in MSM from Toronto.
In summary, the prevalence of anal HPV and HR-HPV infection was high in a cohort of older MSM in Toronto, Canada, but no participant tested positive for all genotypes targeted by the nonavalent vaccine. Risk factors associated with HR-HPV infection for the entire cohort were HIV serostatus, smoking and the number of lifetime sexual partners. Our findings will be useful to inform HPV vaccine rollout and HPV prevention strategies in Canadian MSM.
Methods
Ethics statement
The study was approved by the Research Ethics Board at the University of Toronto (Toronto, Canada). Research was performed in accordance with the relevant guidelines and regulations. Informed, written consent was obtained from all participants.
Study population
Self-identified MSM were recruited into a cross-sectional study of the epidemiology of HIV and other co-infections at the Maple Leaf Medical Clinic (MLMC) in downtown Toronto, Canada between September 2010 and June 2012. All self-identified MSM at or over the age of 16 receiving clinical care from MLMC were invited to participate in the study. A high-level overview of the prevalence of sexually transmitted infections in this cohort has been previously described24.
Study protocol and specimen collection
Participants attended a single study visit. They completed a computerized, self-administered ACASI questionnaire (Audio Computer Assisted Self-Interview; Questionnaire Development System (QDS) 2.5, Nova Research Company, Bethesda, USA), which included information about socio-demographics, sexual and medical history. The sections on the ACASI questionnaire included: (1) interview information, (2) socio-economic characteristics, (3) sexual history and behavior, (4) STI, hepatitis and HIV testing, diagnosis and treatment, (5) other health behaviors, and (6) HIV and STI knowledge, beliefs and attitudes. Blood, first-void urine and a self-collected anal swab were collected to perform diagnostics tests against viral and bacterial infections as described in the next section. All specimens were stored at 4 °C until pick-up.
Laboratory tests
Participants were screened for HIV, herpes simplex virus (HSV)-1/2, cytomegalovirus (CMV), hepatitis C (HCV), hepatitis B (HBV) and syphilis with serology tests using 20 mL of blood collected in the serum separating tube and the acid citrate dextrose (ACD) tube. First-void urine was used to test for N. gonorrhoeae and C. trachomatis as previously described24. For HBV testing, “active HBV infection” was defined as having a detectable HBV surface Ag and “ever infected with HBV” was defined as having undetectable HBV surface Ag but a positive HBV surface or core Ab with no vaccination history. With regards to syphilis testing, non-reactive CMIA test was considered as negative, “active syphilis” was defined by positive reactions from all three tests (CMIA, RPR and TPPA), and “previously treated syphilis” was defined by having reaction to CMIA and TPPA but not RPR.
HPV genotyping
Participants were instructed to self-collect an anal swab by moistening the CultureSwab polyester-tipped swab (BD) tip with a saline solution, inserting the swab about 2–3 cm into the anus and rotating the swab 10 times in one direction and 10 times the other direction. Self-collected anal swab was collected in PreservCyt Transport Medium (Cytyc Corporation) and used to perform microsphere-based HPV genotyping (Luminex Corporation, Austin, USA) to test for 46 mucosal HPV genotypes at the Toronto Public Health Laboratory39. Of note, 13 of the 46 genotypes were defined as being high-risk: HPV-16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68. All other genotypes were defined as being low-risk. DNA from anal samples were extracted using the Roche MagNA pure 96 automatic extractor. In brief, samples were spun down and subsequently eluted using MagNA Pure 96 DNA and Viral NA Large Volume Kit (Roche) and the Viral NA Universal Program. HPV DNA extracted from anal swabs was amplified by nested PCR using AmpliTaq Gold DNA polymerase (Perkin-Elmer) with the PGMY primers followed by the GP5+/GP6+ primers. HPV type-specific probes of 30 nucleotides in length located at the L1 gene were used to detect the PCR products by xMAP technology. Hybridization was analyzed using a Luminex Liquid Chip 200 flow cytometer (Qiagen) and the Luminex IS software (Luminex). A fluorescence signal of 100 fluorescent units or higher was determined as the threshold for positivity. Beta-globin negative specimens post-amplification were considered invalid and therefore excluded from our analyses.
Statistical analysis
Data from the laboratory and the ACASI questionnaire were analyzed using SPSS, version 27 for Mac (SPSS). Wilcoxon–Mann–Whitney test was used for continuous variables being reported with medians and interquartile ranges (IQR), while Chi-square test was performed for categorical variables being reported as frequencies and proportions with 95% confidence intervals (CIs). Factors associated with anal HR-HPV infection were determined using logistic regression. A conceptual framework of anal HPV infection among MSM was constructed based on the literature, to help better understand the different risks and correlates, along with any potential interactions, and to guide the construction of our multivariable model. Multicollinearity was assessed by checking the ‘tolerance’ and ‘variance inflation factor’, and it was determined that none of the variables in the models constructed had ‘tolerance’ or ‘variance inflation factor’ values that indicated multicollinearity. A combination of a priori and a change-in-estimate inclusion of variables were used for our model. The following variables that have consistently been associated with HR-HPV infection were selected a priori regardless of the results from the univariate analyses: history of receptive anal intercourse in the last 6 months, HIV serostatus, lifetime number of male sexual partners and smoking status. The following variables were selected using a change-in-estimate approach, defined as changing the parameter estimate of the primary risk factor variable—receptive anal intercourse—by 10% or higher: number of sexual partners in the last 6 months, use of methamphetamine, ecstasy or MDMA in the last 6 months and drug use within two hours of sexual activity.
References
Koutsky, L. Epidemiology of genital human papillomavirus infection. Am. J. Med. 102, 3–8. https://doi.org/10.1016/s0002-9343(97)00177-0 (1997).
de Villiers, E. M. Cross-roads in the classification of papillomaviruses. Virology 445, 2–10. https://doi.org/10.1016/j.virol.2013.04.023 (2013).
Muhr, L. S. A., Eklund, C. & Dillner, J. Towards quality and order in human papillomavirus research. Virology 519, 74–76. https://doi.org/10.1016/j.virol.2018.04.003 (2018).
Machalek, D. A. et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: A systematic review and meta-analysis. Lancet Oncol. 13, 487–500. https://doi.org/10.1016/S1470-2045(12)70080-3 (2012).
zur Hausen, H. Papillomaviruses and cancer: From basic studies to clinical application. Nat. Rev. Cancer 2, 342–350. https://doi.org/10.1038/nrc798 (2002).
De Vuyst, H., Clifford, G. M., Nascimento, M. C., Madeleine, M. M. & Franceschi, S. Prevalence and type distribution of human papillomavirus in carcinoma and intraepithelial neoplasia of the vulva, vagina and anus: A meta-analysis. Int. J. Cancer 124, 1626–1636. https://doi.org/10.1002/ijc.24116 (2009).
Lin, C., Franceschi, S. & Clifford, G. M. Human papillomavirus types from infection to cancer in the anus, according to sex and HIV status: A systematic review and meta-analysis. Lancet Infect. Dis. 18, 198–206. https://doi.org/10.1016/S1473-3099(17)30653-9 (2018).
Islami, F., Ferlay, J., Lortet-Tieulent, J., Bray, F. & Jemal, A. International trends in anal cancer incidence rates. Int. J. Epidemiol. 46, 924–938. https://doi.org/10.1093/ije/dyw276 (2017).
Silverberg, M. J. et al. HIV infection and the risk of cancers with and without a known infectious cause. AIDS 23, 2337–2345. https://doi.org/10.1097/QAD.0b013e3283319184 (2009).
Chiao, E. Y., Krown, S. E., Stier, E. A. & Schrag, D. A population-based analysis of temporal trends in the incidence of squamous anal canal cancer in relation to the HIV epidemic. J. Acquir. Immune Defic. Syndr. 40, 451–455. https://doi.org/10.1097/01.qai.0000159669.80207.12 (2005).
Siddharthan, R. V., Lanciault, C. & Tsikitis, V. L. Anal intraepithelial neoplasia: Diagnosis, screening, and treatment. Ann. Gastroenterol. 32, 257–263. https://doi.org/10.20524/aog.2019.0364 (2019).
Corral, J. et al. Clinical results of infrared coagulation as a treatment of high-grade anal dysplasia: A systematic review. Tech. Coloproctol. 23, 707–712. https://doi.org/10.1007/s10151-019-02041-7 (2019).
Poynten, I. M. et al. The natural history of anal high-grade squamous intraepithelial lesions in gay and bisexual men. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa166 (2020).
Palefsky, J. M. et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N. Engl. J. Med. 365, 1576–1585. https://doi.org/10.1056/NEJMoa1010971 (2011).
Castellsague, X. et al. Immunogenicity and safety of the 9-valent HPV vaccine in men. Vaccine 33, 6892–6901. https://doi.org/10.1016/j.vaccine.2015.06.088 (2015).
Public, H. A. O. C. Updated Recommendations on Human Papillomavirus Vaccines: 9-valent HPV vaccine and clarification of minimum intervals between doses in the HPV immunization schedule. https://www.canada.ca/en/public-health/services/publications/healthy-living/9-valent-hpv-vaccine-clarification-minimum-intervals-between-doses-in-hpv-immunization-schedule.html (2016).
(NACI), N. A. C. o. I. Updated Recommendations on Human Papillomavirus (HPV) Vaccines: 9-valent HPV vaccine 2-dose immunization schedule and the use of HPV vaccines in immunocompromised populations. https://www.canada.ca/en/public-health/services/publications/healthy-living/updated-recommendations-human-papillomavirus-immunization-schedule-immunocompromised-populations.html (2017).
(NACI), N. A. C. o. I. NACI Statement: HPV vaccine update. (2012).
Grace, D. et al. Economic barriers, evidentiary gaps, and ethical conundrums: A qualitative study of physicians’ challenges recommending HPV vaccination to older gay, bisexual, and other men who have sex with men. Int. J. Equity Health 18, 159. https://doi.org/10.1186/s12939-019-1067-2 (2019).
Giuliano, A. R. et al. Seroconversion following anal and genital HPV infection in men: The HIM study. Papillomavirus Res. 1, 109–115. https://doi.org/10.1016/j.pvr.2015.06.007 (2015).
Beachler, D. C., Jenkins, G., Safaeian, M., Kreimer, A. R. & Wentzensen, N. Natural acquired immunity against subsequent genital human papillomavirus infection: A systematic review and meta-analysis. J. Infect. Dis. 213, 1444–1454. https://doi.org/10.1093/infdis/jiv753 (2016).
Clarke, M. A. & Wentzensen, N. Strategies for screening and early detection of anal cancers: A narrative and systematic review and meta-analysis of cytology, HPV testing, and other biomarkers. Cancer Cytopathol. 126, 447–460. https://doi.org/10.1002/cncy.22018 (2018).
Han, J. J., Beltran, T. H., Song, J. W., Klaric, J. & Choi, Y. S. Prevalence of genital human papillomavirus infection and human papillomavirus vaccination rates among US adult men: National Health and Nutrition Examination Survey (NHANES) 2013–2014. JAMA Oncol. 3, 810–816. https://doi.org/10.1001/jamaoncol.2016.6192 (2017).
Remis, R. S. et al. Prevalence of sexually transmitted viral and bacterial infections in HIV-positive and HIV-negative men who have sex with men in Toronto. PLoS ONE 11, e0158090. https://doi.org/10.1371/journal.pone.0158090 (2016).
Torres, M. et al. Anal human papillomavirus genotype distribution in HIV-infected men who have sex with men by geographical origin, age, and cytological status in a Spanish cohort. J. Clin. Microbiol. 51, 3512–3520. https://doi.org/10.1128/JCM.01405-13 (2013).
Ucciferri, C. et al. Prevalence of anal, oral, penile and urethral Human Papillomavirus in HIV infected and HIV uninfected men who have sex with men. J. Med. Virol. 90, 358–366. https://doi.org/10.1002/jmv.24943 (2018).
Ren, X. et al. Human papillomavirus positivity in the anal canal in HIV-infected and HIV-uninfected men who have anal sex with men in Guangzhou, China: Implication for anal exams and early vaccination. Biomed. Res. Int. 2017, 2641259. https://doi.org/10.1155/2017/2641259 (2017).
Nyitray, A. G. et al. Six-month incidence, persistence, and factors associated with persistence of anal human papillomavirus in men: The HPV in men study. J. Infect. Dis. 204, 1711–1722. https://doi.org/10.1093/infdis/jir637 (2011).
Phanuphak, N. et al. Anal human papillomavirus infection among Thai men who have sex with men with and without HIV infection: Prevalence, incidence, and persistence. J. Acquir. Immune Defic. Syndr. 63, 472–479. https://doi.org/10.1097/QAI.0b013e3182918a5a (2013).
Hu, Y. et al. Anal human papillomavirus infection among HIV-infected and uninfected men who have sex with men in Beijing, China. J. Acquir. Immune Defic. Syndr. 64, 103–114. https://doi.org/10.1097/QAI.0b013e31829b6298 (2013).
van Aar, F. et al. Anal and penile high-risk human papillomavirus prevalence in HIV-negative and HIV-infected MSM. AIDS 27, 2921–2931. https://doi.org/10.1097/01.aids.0000432541.67409.3c (2013).
Dona, M. G. et al. Prevalence, genotype diversity and determinants of anal HPV infection in HIV-uninfected men having sex with men. J. Clin. Virol. 54, 185–189. https://doi.org/10.1016/j.jcv.2012.02.014 (2012).
Strong, C. et al. Prevalence and risk factors of anogenital human papillomavirus infection in a community sample of men who have sex with men in Taiwan: Baseline findings from a cohort study. Sex Transm. Infect. 96, 62–66. https://doi.org/10.1136/sextrans-2018-053629 (2020).
Nyitray, A. G. et al. Incidence, duration, persistence, and factors associated with high-risk anal human papillomavirus persistence among HIV-negative men who have sex with men: A multinational study. Clin. Infect. Dis. 62, 1367–1374. https://doi.org/10.1093/cid/ciw140 (2016).
Marra, E., Lin, C. & Clifford, G. M. Type-specific anal human papillomavirus prevalence among men, according to sexual preference and HIV status: A systematic literature review and meta-analysis. J. Infect. Dis. 219, 590–598. https://doi.org/10.1093/infdis/jiy556 (2019).
Poynten, I. M. et al. Vaccine-preventable anal human papillomavirus in Australian gay and bisexual men. Papillomavirus Res. 3, 80–84. https://doi.org/10.1016/j.pvr.2017.02.003 (2017).
Hernandez, A. L. et al. Incidence of and risk factors for type-specific anal human papillomavirus infection among HIV-positive MSM. AIDS 28, 1341–1349. https://doi.org/10.1097/QAD.0000000000000254 (2014).
Ong, J. J. et al. Incidence, clearance, and persistence of anal human papillomavirus in men who have sex with men living with human immunodeficiency virus: Implications for human papillomavirus vaccination. Sex Transm. Dis. 46, 229–233. https://doi.org/10.1097/OLQ.0000000000000958 (2019).
Zubach, V., Smart, G., Ratnam, S. & Severini, A. Novel microsphere-based method for detection and typing of 46 mucosal human papillomavirus types. J. Clin. Microbiol. 50, 460–464. https://doi.org/10.1128/JCM.06090-11 (2012).
Acknowledgements
We acknowledge the participants who took the time to take part in this study.
Funding
This work was supported by the Canadian Institutes of Health Research (CIHR) (R.K. #TE2-138200 and #HET-85518). Y.C. received studentship from the CIHR’s Frederick Banting and Charles Best Canada Graduate Scholarships Doctoral Award and the Ontario Graduate Scholarship—Queen Elizabeth II/Aventis Pasteur Graduate Scholarship in Science and Technology. T.G received CIHR Canadian HIV Trials Network Post-Doctoral Fellowship.
Author information
Authors and Affiliations
Contributions
R.K., R.R., and M.L. contributed to the conception and design of the study, J.B., G.S, T.R. and R.H. coordinated the study including patient recruitment, A.R. and S.H. prepared specimens and performed laboratory experiments and assays, J.L., Y.C., and T.G. performed statistical analysis and Y.C. and R.K. drafted the manuscript. All authors have edited and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, Y., Loutfy, M., Remis, R.S. et al. HPV genotyping and risk factors for anal high-risk HPV infection in men who have sex with men from Toronto, Canada. Sci Rep 11, 4779 (2021). https://doi.org/10.1038/s41598-021-84079-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84079-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.