Abstract
Amid growing concern regarding the potential added burden of care due to population aging, we have very little understanding of what is the burden of care in aging populations. To answer this question, we introduce a novel metric that encompasses demographic complexity and social context to summarize unpaid family care work provided to children, elderly, and other family members across the life cycle at a population level. The measure (Care Life Expectancy), an application of the Sullivan method, estimates the number of years and proportion of adult life that people spend in an unpaid caregiving role. We demonstrate the value of the metric by using it to describe gender differences in unpaid care work in 23 European aging countries. We find that at age 15, women and men are expected to be in an unpaid caregiving role for over half of their remaining life. For women in most of the countries, over half of those years will involve high-level caregiving for a family member. We also find that men lag in caregiving across most countries, even when using the lowest threshold of caregiving. As we show here, demographic techniques can be used to enhance our understanding of the gendered implications of population aging, particularly as they relate to policy research and public debate.
Similar content being viewed by others
Introduction
Population aging has been a matter of concern in the United States and Europe for the past several decades. One primary concern is that the share of the population that will require health services and pension benefits is increasing while the share of the population that will provide for these needs is decreasing (Bloom et al. 2010; Bongaarts 2004; Christensen et al. 2009; Gruber and Wise 2000; Murphy et al. 2006). So far, the debate has centered mostly around the economic consequences of population aging, rendering demographers to focus on the duration of working life to project how long people are expected to be economically active and contribute to social security given current rates of employment and current mortality schedules (Dudel and Myrskylä 2017, 2020; Loichinger and Weber 2016; Skoog and Ciecka 2010).
The focus on employment overlooks unpaid care work, which is a crucial pillar in aging societies. Theoretically, as people are living longer, they will also require more unpaid family support, but fewer family members will be available to provide it. Although the potential added burden of care due to population aging is a concern, we have little understanding of what the burden of care is in aging populations. Families are the primary source of caregiving for their members, regardless of the generosity of national social services (Albertini et al. 2007; Brandt and Deindl 2013; Brandt et al. 2009; Schmid et al. 2012). However, women do the majority of unpaid care work within families continuously over the life course by taking care of their children, spouses, parents, and other members of their kinship networks (Patterson and Margolis 2019). Moreover, there is evidence that taking an unpaid caregiving role is a barrier to women’s participation in paid work (Crespo and Mira 2010; Dentinger and Clarkberg 2002; Hochman and Lewin-Epstein 2013; Lumsdaine and Vermeer 2015; Rupert and Zanella 2018; Van Bavel and De Winter 2013; Wakabayashi and Donato 2005). Thus, the study of the burden of care is central in the study of population aging and its potential gendered implications.
In this paper, we ask what is the burden of care in aging populations? We answer this question by proposing a novel life expectancy measure that provides an intuitive, descriptive, and comparative summary of unpaid family care work that people provide not only to older adults or children, but to all family members throughout adulthood, by looking after them or helping with daily activities. Using a demographic approach, we measure unpaid family care work as a role, or a state, i.e., people who provide care to family members are in a caregiving role. This conceptualization is comparable to other demographic states that have cumulative durations, such as employment and health.
We argue that by estimating the duration of caregiving life, i.e., how many years people are expected to be in a caregiving role, we can summarize family unpaid work in a manner that goes beyond a single-life stage and a particular form of care. Meaning, measuring caregiving as a role allows us to harmonize unpaid family care work continuously over the life cycle. Moreover, this measure encompasses the complexities of counteracting demographic forces such as longevity, fertility, and morbidity that have given rise to variations in degree of population aging and patterns of caregiving, thus facilitating comparisons across populations. By assuming mortality rates, birth rates, and care proportions remain relatively stable over time, and that net migration is zero, care life expectancies can be interpreted as projections of the expected number of years people will provide care into the future, making them useful for policy planning. Using this measure, we provide the first descriptive account of the burden of care of women and men across 23 European countries.
Literature Review
Existing research on unpaid care work often focuses on a single type of caregiving, for example, childcare or elderly care, or a single-life stage, for instance middle-age or older adulthood (Craig and Mullan 2011; Glauber 2017; Grigoryeva 2017; Hank and Buber 2009). However, the provision of unpaid care work spans the life course and takes on various forms as women and men transition into and out of familial roles. Childcare occurs when one becomes a parent, and grandchild care ensues when one becomes a grandparent. Unpaid caregiving also includes providing assistance with Activities of Daily Living (ADL), such as dressing and bathing, as well as Instrumental Activities of Daily Living (IADL), such as doing housework and shopping (Spillman and Pezzin 2000). These forms of care are often provided to disabled, ill, or elderly family members and can occur throughout the life course as family members experience disability or illness, but are more likely to occur as parents and partners enter their elderly years (Patterson and Margolis 2019). At every life stage, women and men face a different set of familial expectations that are embedded in kinship structures and gender dynamics (Ferree 1990, 2010). In keeping with these differential expectations, a gender gap in unpaid care work emerges at every stage of the life course (Craig and Mullan 2011; Glaser et al. 2013; Grigoryeva 2017; Hank and Buber 2009; Leopold et al. 2014; Patterson and Margolis 2019; Raley et al. 2012; Sarkisian and Gerstel 2004; Schmid et al. 2012).
Current demographic research on caregiving is flourishing yet fragmented. One commonly used indicator to signal both economic and non-economic burdens is the old-age-dependency ratio, which is the ratio between the population over age 65 and the population between ages 15 and 64. This measure has many limitations (Sanderson and Scherbov 2015), but most importantly it does not consider that care is unequally divided both over the life cycle and between women and men. Another body of work focuses on “shared lives” (Bengtson 2001) and estimates the duration of life spent in familial roles in the context of increasing longevity and declining fertility. This research shows that across Europe and the U.S., the years men and women are expected to spend as parents to adult children and as grandparents is increasing (Leopold and Skopek 2015; Margolis 2016; Margolis and Verdery 2019; Margolis and Wright 2017; Watkins, Menken and Bongaarts 1987). Finally, a related, prolific body of work focuses on the “sandwich generation,” who provide care to multiple generations simultaneously while still in prime working ages and are often women (Grundy and Henretta 2006; Vlachantoni et al. 2019). This stream of research highlights the burden of care in a particular life stage that is increasingly becoming dense with multiple caregiving responsibilities, but overlooks unpaid work provided to only one generation.
Understanding the changing nature of multigenerational relationships is important because demographic changes suggest a transformation in the kinship-based safety nets that family members can potentially use in times of need (Bengtson 2001; Swartz 2009). However, estimating the potential supply of caregivers or focusing on a single-life stage does not inform us of the cumulative burden of care that family members provide for each other throughout adulthood. Further, a focus on potential caregivers also masks the gendered nature of caregiving and the gendered nature of longevity, fertility, and morbidity. If we wish to capture the gendered burden of care holistically for a population, we need an encompassing measure of unpaid care work that considers the dynamic nature of care over the life cycle as well as the multiple directions of caregiving it involves. Measuring caregiving as a life expectancy will offer a new demographic perspective on unpaid caregiving that is missing, yet central to the debate around population aging.
Caregiving and Population Aging
How is population aging linked to unpaid care work? Unpaid family care work is not merely a private act of love and kinship support (England 2005; Folbre 2001). Caregiving is a reaction to the core demographic events (Johnson-Hanks 2015) that determine population aging (Agree and Glaser 2009), including fertility (caring for children and grandchildren), morbidity (caring for ill or disabled family members), and longevity (caring for elderly family members).
One main characteristic of population aging is high life expectancy. Longevity varies across Europe, but has remained stable over the past decade (Raleigh 2019), and people are expected to live for many years in high-income countries. Still, women live longer than men in all countries (Raleigh 2019). Women’s higher life expectancies and greater involvement in caregiving at every life stage (Patterson and Margolis 2019) imply that the duration of caregiving life is longer for women than for men.
However, longevity varies across Europe. Life expectancy for both women and men is lower in Eastern European countries than in Western and Southern Europe (Raleigh 2019). The regional differences in life expectancy suggest that there should be cross-national variation in the duration of caregiving life among women and men. If longer lives imply longer duration of caregiving life, then women and men in countries with higher life expectancy will have a longer duration of caregiving life, and vice versa.
Low fertility is another characteristic of aging populations (Caldwell 2001). A primary concern surrounding population aging, as it relates to caregiving, is directly related to low fertility. The concern is that countries with relatively low fertility have relatively fewer potential caregivers to the elderly and a larger burden of elderly care falling on younger generations due to high life expectancy. On the other hand, low fertility may suggest that parents and grandparents will have a smaller childcare burden.
However, fertility interacts in complex ways with longevity to impact caregiving because low fertility is a result, in part, of postponement (Bongaarts and Feeney 1998; Sobotka 2004). Early fertility combined with longevity suggests longer “shared lives,” but fertility postponement may have the opposite effect. For instance, Leopold and Skopek (2015) demonstrated that the longest grandparenthood durations were in countries where early fertility concurs with high life expectancy (U.S.) and shortest in countries with high life expectancy and delayed fertility (Spain). Therefore, low fertility in aging populations may have counteracting implications for the duration of caregiving life depending on longevity.
Morbidity is a third integral demographic process with implications for the duration of caregiving life, as it relates to both demand for care and the ability to provide care. There is great variation in morbidity across Europe. Scholars have found higher proportions of the population in frail states in Southern Europe as compared to Northern Europe (Romero-Ortuno et al. 2013; Santos-Eggimann et al. 2009), and health expectancy is lower in Eastern Europe as compared to nations that were part of the EU prior to 2004 (Jagger et al. 2008). Moreover, there is a well-documented “male–female health-survival paradox,” wherein women have higher longevity, but worse health, as compared to same-age men (Case and Paxson 2005; Mathers et al. 2001; Nusselder et al. 2010; Oksuzyan, Brønnum-Hansen and Jeune 2010) This results in a gender gap in longevity that is wider than the gender gap in health expectancy, suggesting that women require more care in their elderly years than men. Moreover, if mortality is equal, we expect countries with higher morbidity to have a higher burden of care because dependent life is increased (Crimmins et al. 1994), meaning younger generations would need to provide more elderly care while older generations would be less able to provide grandchild care or spousal care.
Demographic forces interact in complex ways, introducing great challenges to the study of unpaid work. However, we argue that estimating caregiving as a life expectancy measure overcomes this complexity. Conceptualizing unpaid care work as a role that spans adulthood allows us to measure its cumulative duration and compare the total burden of care across aging populations which have different “aging regimes,” i.e., different combinations of longevity, fertility, and morbidity characteristics. In this paper, we estimate the burden of care in a broad and encompassing manner, offering an initial holistic, descriptive account of unpaid care work at the population level by estimating the duration of caregiving life for women and men across 23 aging countries.
The Cross-National Context
We take a cross-national approach to demonstrate the utility of our measure. The social contexts of the countries we study are embedded in this comparative approach, as well as the degree of population aging based on underlying fertility, mortality, and morbidity pattern. We introduce a measure that summarizes care work across these endogenous domains, making countries comparable.
Countries vary in the degree to which policies aim to promote gender equality (for review see Lewis 1992; Orloff 1996; Pfau-Effinger 2005). Policies and culture structure gender relations differently as the norms and expectations of women and men in the private and public spheres are distinct (for review of gender ideologies see Davis and Greenstein 2009). Thus, although women are responsible for most of the unpaid care work worldwide (Addati 2018), some countries are more egalitarian and facilitate gender equality, while others facilitate the traditional gender segregation of labor (Jappens and Van Bavel 2012; Kalmijn and Saraceno 2008).
The welfare state shapes gender relations through its social provisions (Lewis 1992; Orloff 1996). Welfare states vary in the extent to which they assign, explicitly or implicitly, caregiving responsibilities to families, especially to women (Leitner 2003). As countries face different demographic challenges, these assigned responsibilities will also vary by the type of caregiving, i.e., for children, elderly, and the disabled, and its intensity, creating different care regimes (Bettio and Plantenga 2004).Footnote 1 There is an abundance of research on the diverse typologies and country clusters of welfare and care regimes. However, these typologies vary by the pool of countries available to researchers, the unit of analysis, and form of care. Nonetheless, scholars consistently find a general divide in caregiving participation between Nordic and Northern European countries and Southern and Eastern European countries.
The Nordic countries follow a universal approach to welfare wherein public care provision is generous (Bettio and Plantenga 2004). Family members are not expected to be the sole caretakers, but instead have a more modest caregiving role because the state offers generous services that reduce the caregiving burden. These countries offer universal and generous childcare as well as elderly care provisions (Bettio et al. 2012; Mills et al. 2014), which alleviates families’ care burden throughout the life course. Moreover, these countries use policies to explicitly promote gender equality, so caregiving responsibilities are shared more equally between women and men (Gornick and Meyers 2003), and family members are less likely to engage in various forms of intensive caregiving compared to other countries (Bettio and Plantenga 2004; Bordone et al. 2017; Hank and Buber 2009; Igel and Szydlik 2011; Saraceno and Keck 2008).
In contrast, Southern and Eastern European countries offer limited social services for children and the elderly, and family members are expected to be the primary caregivers (Bettio and Plantenga 2004; Mills et al. 2014; Sarasa 2008). Women have a crucial caregiving role and are more likely to provide intense, daily care for family members than are men (Bordone et al. 2017; Brandt et al. 2009; Hofäcker et al. 2011). Continental European countries offer “patchy” sets of policies, wherein families are assigned primary caregiving responsibilities, but are offered some welfare assistance in various forms to support those responsibilities; however, childcare and elderly care might be prioritized differently across Continental Europe (Bettio and Plantenga 2004; Gannon and Davin 2010). In these countries, the gender gap in care tends to be larger than in the Nordic countries but not as high as in Eastern and Southern Europe (Bordone et al. 2017; Igel and Szydlik 2011).
Being a caregiver can have different meanings across different countries. Thus, the discussion about the duration of caregiving life should be sensitive to the levels at which people provide care. One consistent finding in the literature shows an inverse relationship between the likelihood of occurrence of any caregiving and the intensity of caregiving across Europe, which follows regional and welfare lines (Albertini et al. 2007). For example, in Southern Europe, people have a lower likelihood of providing care for family members in general, but when they do provide care it is more likely to be intense, i.e., daily. In contrast, in Scandinavia and Northern Europe, people are more likely to provide any care but are less likely to provide intense care. Countries in continental Europe exhibit an intermediate pattern, with a moderate likelihood to provide care and a moderate intensity of such care. This trend is evident for grandchild care, parental care and even in the exchange of intergenerational financial support (Albertini et al. 2007; Bettio and Plantenga 2004; Bordone et al. 2017; Brandt and Deindl 2013; Brandt et al. 2009; Esping-Andersen 2009; Hank and Buber 2009; Igel and Szydlik 2011; Schmid et al. 2012).
It is vital to consider various levels of caregiving within the duration of caregiving life when comparing across populations. Thus, we estimate the total duration of caregiving life as well as the duration of caregiving life by level of caregiving, capturing both the occurrence and intensity of caregiving over the life cycle. Building on past research, we expect that, overall, the duration of caregiving life will involve a smaller proportion of intense caregiving in the Nordic countries and a greater proportion of intense caregiving in the Southern and Eastern European countries. We also expect that women’s duration of caregiving life will involve a greater proportion of years in intense caregiving as compared with men across all countries.
Data and Methods
Data
To calculate care as a life expectancy, we utilize two sources of data: period life tables and cross-sectional survey data. We use abridged (5-year interval) period life tables from the Human Mortality Database, which provide us with information about the mortality schedule and life expectancy by gender and country.
The cross-sectional survey data provide us with individual-level caregiving participation information. We use the European Social Survey (ESS), a biennial, cross-national, and cross-sectional survey. It is nationally representative of the adult population aged 15 and over living in private households in each participating country. The survey measures a variety of topics including attitudes, beliefs, and behaviors in more than 30 countries, with core and rotating thematic modules. We use data from the second round of the survey (ESS2 hereafter), collected via face-to-face interviews in 2004/2005. The thematic module in ESS2 focused on issues related to family, work, and wellbeing and is the only module to include specific questions about unpaid care work across 26 European countries.
We excluded Italy, Iceland, and Turkey; both Italy and Iceland had sample sizes too small to generate age-specific care proportions under the Sullivan method, and Turkey’s population is projected to grow (Chawla et al. 2007), making it an outlier with regard to population aging. Hence, the current analysis includes 44,803 people (54% women) that had information about their gender and age (99.3% of the available sample) from 23 European countries representing a range of regional, social, and demographic contexts. Table 1 shows the participating countries, country codes, sample sizes, and survey years.
Measures
ESS2 asks respondents two questions about providing unpaid care both inside and outside of the household. First, respondents are asked “And apart from housework, do you look after others in your household, such as small children or someone ill, disabled or elderly?” to which respondents answer “yes” or “no.” Next, the ESS2 asks “Apart from your own children, how often, if at all, do you give unpaid help to a family member or relative outside your household with childcare, other care, housework or home maintenance?”Footnote 2 Possible answers include “never,” “less than once a month,” “once a month,” “several times a month,” “once a week,” “several times a week,” or “every day.”
To measure the total duration of caregiving life, we first classify respondents as caregivers if they provided any care at any frequency. Then, we divide the provision of any care into three mutually exclusive levels of caregiving: high, medium, and low. There is no single, agreed-upon cut-off for different levels of caregiving in the literature, but scholars usually classify caregiving as intense if it exceeds 15 or 20 average weekly hours (Arpino and Bordone 2014; Berecki-Gisolf et al. 2008; Carmichael et al. 2010; Di Gessa et al. 2016; Jacobs et al. 2014). In the absence of information about hours of caregiving, studies using a stylized frequency scale similar to the one in ESS2 classify caregiving that is provided daily or several times a week as intense (Bordone et al. 2017; Hank and Buber 2009; Igel and Szydlik 2011). Finally, some studies define any caregiving in which the caregiver resides with the care recipient as intense (Jang et al. 2012; Marks et al. 2002).
We follow past research by incorporating both frequency and residency to distinguish between varying levels of caregiving. We define caregiving as high level if respondents reported they were looking after someone in their household or if they reported providing care every day or several times a week to someone outside the household (Haberkern et al. 2015). We define caregiving as medium level when respondents report providing care outside the household once a week or several times a month (Bordone et al. 2017). Low-level caregiving refers to respondents who reported providing care outside the household once a month or less.
We classify respondents who reported they do not look after anyone in the household and never provide unpaid help outside the household as non-caregivers. We also classify missing cases as non-caregivers, although we do not expect this to significantly alter our results given that missingness is low; the data regarding care provided in the household contain 206 (0.5%) missing cases, and the data regarding care provided outside the household contain 651 missing cases (1.5%). After classifying respondents’ caregiving status and level, we generate age-specific-proportions of caregiving participation for men and women in each country. These proportions are weighted using the post-stratification weight and are smoothed using a running average.
Analytic Strategy
We use the Sullivan method (Sullivan 1971) to estimate life expectancy in a caregiving role (CareLE) for women and men in each country. The Sullivan method is commonly used to calculate Healthy Life Expectancy, i.e., the number of years that people are expected to live in a healthy state (Crimmins and Saito 2001). We build on work by other demographers that have applied the Sullivan method to estimate life expectancy in various states, for example, the number of years people are expected to be in a happy state (Yang 2008), and the number of years older adults are expected to be grandparents (Margolis 2016), healthy grandparents (Margolis and Wright 2017), or in the labor force (Loichinger and Weber 2016). Similar to Healthy Life Expectancy, CareLE presents the burden of care in a given year within a population, adjusted for mortality levels and age structure, and articulated as the number of remaining years at a given age that an individual is expected to live as a caregiver (Jagger et al. 1999).
The Sullivan Method enables us to apportion total person-years lived, i.e., the number of years lived by the population, from life table data into person-years lived as a caregiver based on age-specific caregiving prevalence rates, i.e., proportions of women and men engaged in care work (Jagger et al. 1999; Yang 2008). We use cross-sectional survey data from the ESS2 to calculate country-, gender-, and age-specific proportions of the population giving unpaid care, \({{}_{n}{}\pi }_{x}\), where age is x and n is the size of the age interval (n = 5). We use country-, gender-, and age-specific person-years lived, \({{}_{n}{}L}_{x}\), from period life tables from the Human Mortality Database. In our analysis, we start with ages 15–19 and end with age 85 and above. We use mortality data for the specific survey year for each country. Then, per Eq. 1, and for each country and gender, we multiply the vector of age-specific caregiving proportions, \({{}_{n}{}\pi }_{x}\), by the corresponding vector of age-specific person-years lived, \({{}_{n}{}L}_{x}\). This creates a vector of person-years lived in a caregiving role at each age interval, \({{}_{n}{}L}_{x}^{\mathrm{care}}\).
Then, using Eq. 2, we sum the vector of person-years lived as a caregiver in each age interval beyond age x into a single number, \({T}^{\mathrm{care}}\). Finally, we divide \({T}^{\mathrm{care}}\) by the radix, or the number of people alive at the beginning of the initial age interval, denoted as \({l}_{x}\), where x is age 15. This results in \({e}_{x}^{\mathrm{care}}\), the number of years the average person is expected to live in a caregiving role at age x, or CareLE. We calculate this separately for high, medium, and low levels of caregiving.
On one hand, the Sullivan method presents a period measure of the burden of care in a specific population while accounting for that population’s age structure, summarized as care life expectancies. However, by making a stationarity assumption, we can also interpret care life expectancies as projections of the expected number of years an individual at age x will spend as a caregiver over her or his life. That is, we assume that populations are stationary where birth rates, age-specific mortality rates, and the age-specific caregiving proportions are unchanging over time, that age-specific proportions of care derived from the cross-sectional survey represent a typical year, and that net migration is zero. These assumptions allow us to create a care life expectancy for a synthetic cohort such that new cohorts are expected to go through the same-age-specific caregiving and mortality schedules.
The stationarity assumption poses a limitation to the interpretation of our measure as a projection if mortality, fertility, migration or caregiving schedules change rapidly (Mathers and Robine 1997). Another limitation of the Sullivan method is that it does not consider individuals’ transition probabilities between states, i.e., the probability that people will transition from a caregiving role to not being a caregiver, or will transition across different levels of caregiving. Methods that account for transition probabilities, like multi-state life tables, might offer more accurate point estimates, but they also require panel data that track individuals over regular intervals of time. Unfortunately, longitudinal or retrospective data on caregiving participation across all adult age groups are not available for an extensive comparative analysis. Nonetheless, the Sullivan method is ideal for calculating life expectancies in particular states using cross-sectional data (see Lynch and Brown 2010).
Results
Descriptive Results
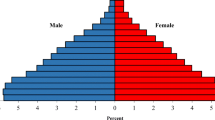
Figure 1 shows the age-specific distribution of participation in any and high-level care over the life cycle for women and men. To best visualize the age-specific distribution of care, we present only the extremes of caregiving levels for six countries that represent different demographic and social contexts. First, Fig. 1 demonstrates marked gender gaps in caregiving, with women more likely than men to provide care across the greater part of the life cycle. The gender gap in caregiving is noticeably smaller in Sweden, concurring with previous studies on gender equality in Scandinavian countries (Gornick and Meyers 2003). The gender gap in care provision, particularly for high-level care, peaks during prime childbearing years, but converges later in the life course. Moreover, the gender gap exists even for the likelihood of providing any care, meaning men’s caregiving lags behind women’s even using the most generous definition of caregiving.
Interestingly, there is a gender crossover late in the life cycle in some countries, wherein men’s caregiving after age 70 is higher than that of women. This pattern is consistent with other studies (Glauber 2017; Kahn et al. 2011; Patterson and Margolis 2019). After retirement, men are increasingly more likely to provide spousal care, which also concurs with the “male–female health-survival” paradox. This pattern could also indicate mortality selection among men, which could explain why there is no crossover in the Czech Republic. The life expectancy of men in Eastern Europe is lower than in other European and developed countries (Aburto and van Raalte 2018; McKee and Shkolnikov 2001).
Figure 1 also shows considerable cross-national and age-specific variation in levels of caregiving, specifically, of providing any care (solid line) and high-level care (dashed lines). Overall, at peak caregiving ages, 50% to 80% of women provide any care, and 40% to 60% provide high-level care compared with 40% to 80% and 30% to 50%, respectively, for men. The largest gap between any and high-level care is evident in Sweden. The age-specific proportions for providing any care are higher in Sweden across the greater part of the life cycle compared to the other countries. However, the age-specific proportions providing high-level care are lower in Sweden, even during the peak years. This pattern suggests that most of the caregiving that women and men provide is not high level and is in striking contrast to Greece, where the age-specific proportions suggest that although proportions providing any care were lower compared to the other countries, most of the care provided is at a high level. The other countries are in between these extremes. This pattern echoes past research (e.g., Albertini et al. 2007) and underscores the importance of including both extremes of caregiving in the estimation of the duration of caregiving life.
Finally, Fig. 1 shows variation in the ebbs and flows of caregiving over the life cycle. High-level caregiving has an obvious peak during prime childbearing years across all six countries for women and men, which is indicative of the concentration of childcare. Caregiving continues after prime childbearing years but with a lower and slowly declining proportion of participation until age 60 and rapidly declining after that. The high proportion of women and men providing any care, but not high-level care, through middle age likely signals the “sandwich” period where people are more likely to be involved in multiple forms of caregiving to multiple generations (Grundy and Henretta 2006). And in spite of a sharp decline in the proportion providing care after age 60, it is also evident that even at 80, women and men continue to participate in some form of caregiving for family members.
Overall, these summary statistics demonstrate the great degree of variation in caregiving by age, gender, and country. Next, we translate these age-specific proportions into life expectancy in a caregiving role by incorporating country-specific mortality regimes.
Duration of Caregiving Life (Care Life Expectancy)
What is the total duration of caregiving life? Fig. 2 shows the total life expectancy at age 15 by caregiving status across all 23 participating countries. The darker bars represent the total CareLE across Europe, i.e., the number of years that women and men age 15 are expected to be in any unpaid caregiving role. The lighter bars represent the number of years that women and men age 15 are expected to be alive, but not in any caregiving role. The horizontal line represents the gender-specific average across all 23 countries. Also, Table 2 shows the total CareLE point estimates as well as total CareLE as a proportion of remaining life by gender and country.
Life expectancy at 15 by caregiving status (years). Note: AT Austria, BE Belgium, CH Switzerland, CZ Czech Republic, DE Germany, DK Denmark, EE Estonia, ES Spain, FI Finland, FR France, GB United Kingdom, GR Greece, HU Hungary, IE Ireland, LU Luxembourg, NL Netherlands, NO Norway, PL Poland, PT Portugal, SE Sweden, SI Slovenia, SK Slovakia, UA Ukraine.
The gender gap in the total CareLE is prominent. Women’s total CareLE ranges from 27 years (Portugal) to 49 years (Norway), whereas men’s total CareLE ranges between 17 years (Portugal) and 50 years (Norway). On average across all countries, at age 15, European women are expected to spend 39 years in any caregiving role throughout adulthood whereas men are expected to spend 33 years. In 19 of the 23 countries, women’s total CareLE is notably higher than men’s total CareLE. In the remaining four countries (Norway, Sweden, Netherlands, and Hungary), the gender gap in total CareLE is less than a year. The countries with the highest CareLE gender gap are Portugal, Greece, Ireland, Estonia, and Denmark.
Although the expected number of years spent in care work is striking, the life expectancies of women and men vary across countries. To account for these differences, we calculate the total CareLE as a proportion of remaining life (Table 2). Women at age 15 are expected to spend between 40% (Portugal) and 73% (Ukraine), and on average 59%, of their remaining life in an unpaid caregiver role. Men at age 15 are expected to spend between 27% (Portugal) and 79% (Norway), and on average 56%, of their remaining life in an unpaid caregiver role. Thus, on average across the 23 countries, over half of women’s and men’s remaining life at age 15 is expected to involve an unpaid caregiving role.
Men’s CareLE has more considerable variation compared with women’s CareLE, suggesting that women tend to bear the primary burden of care. The gender gap in the total CareLE suggests that despite the very low threshold, i.e., considering any frequency of caregiving, and despite the gender crossover later in life (shown in Fig. 1), men lag in their participation in care work when we add up all caregiving that is provided over the life cycle. To sum, the results for the total CareLE suggest that being a caregiver for family members is a significant part of people’s lives and more so for women.
Interestingly, Fig. 2 also shows that the total CareLE does not align with the total Life Expectancy at age 15, meaning longer lives do not imply longer caregiving lives. The Eastern European countries, which have the lowest life expectancies, do not exhibit an unusually shorter duration of caregiving life compared to the countries with higher life expectancies, and the countries with the highest life expectancies, such as Spain, Switzerland, France, and Sweden, are across the CareLE spectrum.
Neither is there a distinct fertility pattern across the total CareLE spectrum. For instance, among countries with above average CareLE, Norway, Finland, and Sweden had TFRs over 1.7, while Austria, Ukraine, and Czech Republic had TFRs of 1.4 and lower. Moreover, France, United Kingdom, Germany, Estonia, Hungary, and Poland have very similar total CareLE (40 years) but very different TFRs, ranging from 1.21 in Poland to 1.92 in France (see Table 3 in Appendix for each country’s demographic indicators). Healthy life expectancy similarly fails to determine a pattern in CareLE. For instance, women’s healthy life expectancy at birth ranges from 72.2 to 72.4 years in Austria, Greece, Luxembourg, and Sweden, but these countries have a large range in CareLE. In sum, demographic indicators are likely to interact with each other and existing policy regimes in complex ways to determine CareLE.
Levels of Caregiving
To fully understand gender and cross-national differences in the burden of care, it is vital to break down total CareLE by levels of caregiving. Figure 3 shows total CareLE at age 15 broken down by level of caregiving for all 23 countries. The black bars represent the proportion of total CareLE that involves high-level caregiving, the dark gray bars represent the share of CareLE that includes caregiving at medium level, and the light gray bars represent the share of CareLE that involve low-level caregiving. Each bar sums to 100% and represents each country’s total Care Life Expectancy as shown in Table 2. The countries are in descending order by the proportion of high-level caregiving (the black bars). The horizontal lines represent 33%, 50%, and 75% to ease interpretation. Table 4 in the Appendix details the point estimates of the bars in years and as proportion of total CareLE.
Total Care Life Expectancy at age 15 by level of caregiving (proportions). Note AT Austria, BE Belgium, CH Switzerland, CZ Czech Republic, DE Germany, DK Denmark, EE Estonia, ES Spain, FI Finland, FR France, GB United Kingdom, GR Greece, HU Hungary, IE Ireland, LU Luxembourg, NL Netherlands, NO Norway, PL Poland, PT Portugal, SE Sweden, SI Slovenia, SK Slovakia, UA Ukraine. High = daily or several times a week; Medium = about once a week or several times a month; Low = once a month or less. 100% = total Care Life Expectancy at age 15.
First, starting with the gender gaps in CareLE by intensity level, Fig. 3 shows that in most of the countries, women’s duration of caregiving life is composed mostly of medium- and high-level caregiving, as more than two thirds of total CareLE includes high- or medium-level caregiving. In contrast, men’s caregiving years are mostly medium- and low-level caregiving. High-level caregiving comprises less than half of men’s total duration of caregiving life across most of the countries. Men’s duration of caregiving life includes more low-level caregiving than women’s and represents a quarter or more of men’s total CareLE. Even in countries with the later-life gender crossover in caregiving we saw in Fig. 1, men’s CareLE does not tend to outpace women’s CareLE because these years contribute few years to the total CareLE and include participation in low-level care.
Figure 4 provides further visualization of the gender gap in years. In most countries, women are expected to spend between 5 and 10 more years in a caregiving role that involves intense caregiving (black circles) compared to men. Luxembourg and Ukraine have the highest gender gap in high-level CareLE (12 and 11 years, respectively), while Norway, Sweden, Finland, and Hungary have the lowest gender gap in high-level CareLE (less than five years). Figure 4 also shows that although the CareLE gender gap is smaller for years involving medium-level care intensity (gray triangles), women still are expected to spend more years in a caregiving role at these levels than men in most countries. In contrast, Fig. 4 highlights that men are expected to spend more years in a caregiving role that involves low-level care intensity (light-gray diamonds) across most countries. To sum, our results suggest that women’s CareLE is both longer and more intense than men’s CareLE.
Care Life Expectancy gender gap at age 15 by level of caregiving. Note Gender gap = Women’s CareLE—Men’s CareLE. High = daily or several times a week; Medium = about once a week or several times a month; Low = once a month or less. AT Austria, BE Belgium, CH Switzerland, CZ Czech Republic, DE Germany, DK Denmark, EE Estonia, ES Spain, FI Finland, FR France, GB United Kingdom, GR Greece, HU Hungary, IE Ireland, LU Luxembourg, NL Netherlands, NO Norway, PL Poland, PT Portugal, SE Sweden, SI Slovenia, SK Slovakia, UA Ukraine.
Shifting back to Fig. 3, there are notable variations across countries in the CareLE composition by intensity levels. We focus on differences in CareLE for women across countries for brevity, but results are similar for men.Footnote 3 The countries with the lowest proportion of high-level caregiving have some of the highest total Care Life Expectancies: Denmark, Sweden, Norway, and Finland. This pattern suggests that women’s caregiving life in these countries is longer, but a smaller proportion of care life is intense relative to women in other countries. In contrast, Portugal, Greece, and Luxemburg have the highest proportions of high-level care. However, these countries had some of the lowest total CareLE. Meaning that women in these countries have a shorter duration of caregiving life, but one composed of more intense care. This pattern echoes past research that finds an inverse relationship between the occurrence and intensity of caregiving across Europe (e.g., Albertini et al. 2007).Footnote 4 An exception to this pattern is Ukraine, where women and men have both a higher total CareLE as well as a higher proportion of high-level caregiving. Meaning, in Ukraine, both women and men are expected to spend more years as caregivers, and most of the caregiving will be intense relative to the other countries.
Interestingly, countries with the lowest proportions of intense caregiving (Denmark, Sweden, Norway, and Finland) tend to share similar demographic profiles (TFRs, age at first birth, life expectancy, HLE, and age-dependency ratios) and care regimes (Bettio and Plantenga 2004), while countries at the highest end of the spectrum (Portugal, Ukraine, Greece, and Luxembourg) are demographically diverse. Portugal and Greece have “classic” population aging characteristics (e.g., very low fertility, postponement of fertility, high life expectancy, high healthy life expectancy, and high old-age-dependency ratio); Ukraine is characterized by very low TFRs, early fertility timing, lower life expectancies, lower old-age-dependency ratios, and lower healthy life expectancies; and Luxembourg is characterized with high TFRs and delayed fertility, and low age-dependency but medium life expectancy and healthy life expectancy.
Also, while Greece and Portugal share similar welfare and care regimes (Bettio and Plantenga 2004; Gal 2010), wherein caregiving responsibilities are delegated to the family, Luxembourg is characterized by a conservative welfare regime (Bambra 2007), wherein caregiving responsibilities are assigned to families, but are somewhat supported by the state (Bettio and Plantenga 2004), similar to Belgium, France, Switzerland, Austria, and Germany which have lower proportions of high-level care. Finally, Ukraine moderately resembles a conservative regime (Fenger 2007). Thus, we see some evidence that women in countries with less state support will spend more years in high-level caregiving. However, other sets of countries that share similar welfare and care regimes do not necessarily share similar CareLE, which suggests that although care regimes are vital for understanding cross-national differences in caregiving levels, demographic characteristics, and care regimes are intertwined in a way that generates a continuous and diverse spectrum of the duration of caregiving life across countries.Footnote 5 CareLE is a measure that encompasses this complexity to make the burden of care across populations comparable.
Conclusion
Population aging has introduced challenges to societies as the share of the population that will require resources has grown and continues to grow, whereas the share of the population that can provide these resources has declined and continues to decline. A focus on the financial burdens of population aging has overshadowed other resource burdens, particularly the burden of unpaid care work. This is in spite of the implications unpaid care work has for a myriad of aging-related topics, such as reforms in pensions, retirement age, and old-age entitlements policies. Moreover, the gendered nature of unpaid care work has meant that women’s work has disproportionately gone unnoticed in the population aging debate. Studies in the US and Europe show that despite a gradual increase in the number of expected years women spend in the labor market, they still spend fewer years in paid work than men (Dudel and Myrskylä 2017; Loichinger and Weber 2016). At the same time, to deal with the increasing burden of old-age entitlements, there has been debate as to whether working life in general and women’s working life in particular should be increased (Bettio et al. 2012). However, this suggestion conflicts with the expectations that women will provide unpaid care work continually over the life course (Glaser et al. 2013). In this context, we bring unpaid care work to the center of the dialog on population aging by generating a benchmark population measure of the burden of care across adulthood.
Unpaid care work is vital for understanding population aging because it is shaped by complex and countervailing demographic determinants. Longevity and fertility influence the length of “shared lives” during which individuals might provide care to family members. Morbidity influences both who requires caregiving and who is able to provide care. We introduce Care Life Expectancy, a novel metric that encompasses this demographic complexity by accounting for care provided across the life cycle while also providing an intuitive summary of the burden of unpaid care work in a population. The measure, an application of the Sullivan method, provides the number of years and proportion of adult life that women and men spend in an unpaid caregiving role. Moreover, this approach allows differentiation between varying levels of caregiving, making this measure a useful tool to compare caregiving burdens across populations. We demonstrate this utility by measuring and comparing CareLE for women and men across 23 European countries.
Our results show that at age 15, women and men in our sample countries are expected to be in an unpaid caregiving role for over half of their remaining adult life. We also find that men lag behind in caregiving across most countries. Using the lowest threshold and averaging across all countries, we find that women are expected to spend 6 additional years as caregivers as compared to men. For women in most of the countries, over half of caregiving years will involve high-level caregiving for a family member, i.e., daily or several times a week. For men in most of the countries, high-level care constitutes less than half of their total caregiving life, but they are expected to spend more years in low-level caregiving. Taken together, our results indicate that unpaid care work is a prominent role in people’s adult life, and more so for women.
Our results also demonstrate that while total duration of caregiving life does not differ dramatically across a majority of countries, there is considerable variation in the proportion of caregiving life composed of high-level caregiving. Compared to other countries in the sample, Nordic countries with generous welfare regimes, more egalitarian gender ideologies, and similar demographic regimes stood out as having caregiving lives that are longer but composed of a smaller proportion of intense care, as well as the smallest gender gap in caregiving life. In contrast, the duration of caregiving life was lower in absolute years and as a proportion of remaining life in Southern European countries, and some Central and Eastern European countries, but it was composed of higher proportions of intense caregiving. However, these countries are demographically diverse, which underscores the intertwined role of social contexts and demographic processes.
Our study has several limitations. First, the measurement of the duration of caregiving life is sensitive to the care measures we use. The questions used here to measure unpaid care work are encompassing, allowing us to conceptualize unpaid work consistently over the life cycle, which are useful for the study’s goal of capturing care as a role. However, our measure of high-level caregiving likely underestimates the gender gap in intense Care Life Expectancy. The current measure assigns a similar high-level intensity role to women and men who provided care within their households, which overlooks women’s added time investment in family work within households (Addati 2018; Craig and Mullan 2011). Moreover, the current measure does not account for people’s multiple caregiving roles, which are more likely to affect women. This limitation is inherent in the conceptualization of care as a role instead of time investment. Our findings that women in most countries spent at least five years more than men in a caregiving role that involved intense caregiving already demonstrate a substantial gender gap. Even with the lowest intensity and most generous definition of care work, a gender gap in care work exists. Meaning, accounting for our underestimation of care work would lead to a more profound gender gap in each of these measures.
Additionally, our care measures do not distinguish types of care given, meaning we cannot apportion the total Care Life Expectancy into the number of years spent in different types of care, e.g., years spent in childcare or elderly care. Other studies offer insight into the ebbs of flows of various types of caregiving over the life cycle (e.g., Patterson and Margolis 2019). Breaking down the number of years spent in each form of care will be an additional step towards a greater understanding of the implications of population aging and the consequences of specific formal care services for unpaid care obligations over the life course. Unfortunately, most large scale, nationally representative surveys do not measure unpaid care work or do not measure it consistently or holistically, hindering comparisons across surveys and over time. Our estimates show that being a caregiver is a prominent role that spans more than half of women’s and men’s adult life, underlining the need to measure unpaid care in nationally representative surveys.
Care Life Expectancy also offers opportunities for future research beyond the scope of the current analysis. For example, our estimates are averages that do not measure heterogeneity among women and men within the same country. Exploring CareLE in the context of stratified life course patterns by education, race, and class (Geruso 2012; Montez et al. 2014; Warner and Brown 2011) will provide further insight into the unequal consequences of population aging.
Furthermore, the COVID-19 pandemic is still unfolding during the preparation of this manuscript, and it is unclear to what extent the pandemic has impacted birth rates, mortality schedules, i.e., age-specific mortality rates, and migration patterns. It is reasonable to assume that COVID-19 will impact the mortality rate at older ages, especially in countries that have been heavily impacted by the pandemic. Moreover, the pandemic has affected the ability of family members to provide care, especially to older adults and grandchildren who live in separate households. These shifts may result in less caregiving, i.e., lower care life expectancies than documented in the current analysis. On the other hand, during the pandemic, more people are providing daily caregiving to those in their households, especially to children. Thus, the age-specific proportions of providing daily care might increase dramatically in middle-adulthood, which could translate to higher care life expectancies. As data become available, future studies should compare post-pandemic CareLE estimates to the benchmark estimates presented here to uncover the effects of COVID-19 on the duration of caregiving life.
Overall, our research makes several contributions. Our study extends the work of other scholars that have used the Sullivan method to summarize other life course states, activities and roles, such as health, work and time in a familial role, as life expectancies (Crimmins and Saito 2001; Dudel and Myrskylä 2017; Loichinger and Weber 2016; Margolis and Wright 2017; Watkins et al. 1987). We also extend demographic work beyond enumerating potential unpaid care providers (e.g., Murphy et al. 2006) to measuring the amount of unpaid care work people are actively providing throughout their lives amidst population aging. We extend current research, which often focuses on a single-life stage or a single form of care (for exception see Patterson and Margolis 2019), and we are the first to summarize caregiving across adulthood as a parsimonious metric.
Our findings also bring to light the centrality, constancy, and cumulative magnitude of unpaid care work in people’s lives, as well as the large gender gap in this work over the life cycle and across countries in a single intuitive measure. In a context of increasing longevity, where scholars seek to understand how people spend their longer lives, focusing on unpaid caregiving roles is instrumental to our understanding of gender inequality across and within populations. As we show here, in the first estimated benchmarks, demographic techniques can be used to enhance our understanding of the gendered implications of population aging, particularly as they relate to policy research and public debate.
Notes
There are numerous combinations of policies and social services that offer care for children and the elderly that fall under the “welfare regime” concept. Countries will vary in the extent to which these services are universal, affordable, and of high quality. Moreover, different countries will prioritize differently childcare and elderly care (or they might equally prioritize both). These provisions refer mostly to formal care arrangements for children, i.e., formal childcare, in-home care, Long-Term Care, and cash transfers that subsidize elderly care. There is an abundance of scholarship that investigates the effects of specific policies on specific types of care at particular life stages (for example, Gannon and Davin 2010; Sarasa 2008). Nonetheless, this literature points to general patterns that align with the general “welfare regime” and “care regimes” concepts. Our goal is to summarize care over the lifecycle and across 23 countries. Therefore, it is beyond the scope of this paper to link specific care policies or specific combinations of care services with CareLE estimates. We use “welfare” in a manner that is guided by previous research on care regimes (to read more about care regimes, see Bettio and Plantenga 2004).
Specifications about kind of unpaid help was excluded from the Norwegian questionnaire, which could affect the distribution of care in Norway.
While the patterns for men in Fig. 3 largely parallel those for women, it is important to note that men in Nordic countries are expected to spend more years in a high-level caregiving role than men in Southern Europe. That is, the proportion of years spent in high-level care work is lower for Nordic men, but this is only because they expect to spend many more years as unpaid caregivers.
There are several explanations for this pattern related to variations across geography, institutionalized familial obligations, values, and co-residence, which shape the frequency and intensity of intergenerational transfers. In the Southern European countries, co-residence is more common, which explains why the intensity is high, but the occurrence (i.e., frequency) is lower. For further reading, see Albertini et al. (2004).
Online Resource 1 shows sensitivity analysis using a different cut-off for high-, medium, and low-level caregiving. The cross-national and gender patterns are robust.
References
Aburto, J. M., & van Raalte, A. (2018). Lifespan dispersion in times of life expectancy fluctuation: The case of central and eastern Europe. Demography, 55(6), 2071–2096.
Addati, L. (2018). Care work and care jobs for the future of decent work. Geneva: International Labour Organization (ILO).
Agree, E. M., & Glaser, K. (2009). Demography of informal caregiving. International handbook of population aging (pp. 647–668). Dordrecht: Springer.
Albertini, M., Kohli, M., & Vogel, C. (2007). Intergenerational transfers of time and money in European families: common patterns—Different regimes? Journal of European Social Policy, 17(4), 319–334.
Arpino, B., & Bordone, V. (2014). Does grandparenting pay off? The effect of child care on grandparents’ cognitive functioning. Journal of Marriage and Family, 76(2), 337–351.
Bambra, C. (2007). Defamilisation and welfare state regimes: A cluster analysis. International Journal of Social Welfare, 16(4), 326–338.
Bengtson, V. L. (2001). Beyond the nuclear family: The increasing importance of multigenerational bonds. Journal of Marriage and Family, 63(1), 1–16.
Berecki-Gisolf, J., Lucke, J., Hockey, R., & Dobson, A. (2008). Transitions into informal caregiving and out of paid employment of women in their 50s. Social Science & Medicine, 67(1), 122–127.
Bettio, F., Corsi, M., D’Ippoliti, C., Lyberaki, A., Lodovici, M. S., & Verashchagina, A. (2012). The impact of the economic crisis on the situation of women and men and on gender equality policies. Brussels: European Commission Brussels.
Bettio, F., & Plantenga, J. (2004). Comparing care regimes in Europe. Feminist Economics, 10(1), 85–113.
Bloom, D. E., Canning, D., & Fink, G. (2010). Implications of population ageing for economic growth. Oxford Review of Economic Policy, 26(4), 583–612.
Bongaarts, J. (2004). Population aging and the rising cost of public pensions. Population and Development Review, 30(1), 1–23.
Bongaarts, J., & Feeney, G. (1998). On the quantum and tempo of fertility. Population and Development Review, 24, 271–291.
Bordone, V., Arpino, B., & Aassve, A. (2017). Patterns of grandparental child care across Europe: The role of the policy context and working mothers’ need. Ageing & Society, 37(4), 845–873.
Brandt, M., & Deindl, C. (2013). Intergenerational transfers to adult children in Europe: do social policies matter? Journal of Marriage and Family, 75(1), 235–251.
Brandt, M., Haberkern, K., & Szydlik, M. (2009). Intergenerational help and care in Europe. European Sociological Review, 25(5), 585–601.
Caldwell, J. C. (2001). Demographers and the study of mortality: Scope, perspectives, and theory. Annals of the New York Academy of Sciences, 954(1), 19–34.
Carmichael, F., Charles, S., & Hulme, C. (2010). Who will care? Employment participation and willingness to supply informal care. Journal of Health Economics, 29(1), 182–190.
Case, A., & Paxson, C. (2005). Sex differences in morbidity and mortality. Demography, 42(2), 189–214.
Chawla, M., Betcherman, G., & Banerji, A. (2007). From red to gray: The" third transition" of aging populations in Eastern Europe and the former Soviet Union. Washington, DC: The World Bank.
Christensen, K., Doblhammer, G., Rau, R., & Vaupel, J. W. (2009). Ageing populations: The challenges ahead. The Lancet, 374(9696), 1196–1208.
Craig, L., & Mullan, K. (2011). How mothers and fathers share childcare: A cross-national time-use comparison. American Sociological Review, 76(6), 834–861.
Crespo, L., & Mira, P. (2010). Caregiving to elderly parents and employment status of European mature women. Documentos de Trabajo (CEMFI)(7) 1.
Crimmins, E. M., Hayward, M. D., & Saito, Y. (1994). Changing mortality and morbidity rates and the health status and life expectancy of the older population. Demography, 31(1), 159–175.
Crimmins, E. M., & Saito, Y. (2001). Trends in healthy life expectancy in the United States, 1970–1990: Gender, racial, and educational differences. Social Science & Medicine, 52(11), 1629–1641.
Davis, S. N., & Greenstein, T. N. (2009). Gender ideology: Components, predictors, and consequences. Annual Review of Sociology, 35, 87–105.
Dentinger, E., & Clarkberg, M. (2002). Informal caregiving and retirement timing among men and women: Gender and caregiving relationships in late midlife. Journal of Family Issues, 23(7), 857–879.
Di Gessa, G., Glaser, K., & Tinker, A. (2016). The impact of caring for grandchildren on the health of grandparents in Europe: A lifecourse approach. Social Science & Medicine, 152, 166–175.
Dudel, C., & Myrskylä, M. (2017). Working life expectancy at age 50 in the United States and the impact of the Great Recession. Demography, 54(6), 2101–2123.
Dudel, C., & Myrskylä, M. (2020). Cohort trends in working life expectancies at age 50 in the United States: A register-based study using social security administration data. The Journals of Gerontology: Series B, 75, 1504–1514.
England, P. (2005). Emerging theories of care work. Annual Review of Sociology, 31, 381–399.
Esping-Andersen, G. (2009). Incomplete revolution: Adapting welfare states to women’s new roles. Oxford: Polity.
European Social Survey Round 2 Data (2004). Data file edition 3.6. NSD—Norwegian Centre for Research Data, Norway—Data Archive and distributor of ESS data for ESS ERIC. https://doi.org/10.21338/NSD-ESS2-2004.
Fenger, M. (2007). Welfare regimes in Central and Eastern Europe: Incorporating post-communist countries in a welfare regime typology. Contemporary Issues and Ideas in Social Sciences, 3(2), 1–30.
Ferree, M. M. (1990). Beyond separate spheres: Feminism and family research. Journal of Marriage and Family, 52(4), 866.
Ferree, M. M. (2010). Filling the glass: Gender perspectives on families. Journal of Marriage and Family, 72(3), 420–439.
Folbre, N. (2001). The invisible heart: Economics and family values. New York: New Press.
Gal, J. (2010). Is there an extended family of Mediterranean welfare states? Journal of European Social Policy, 20(4), 283–300.
Gannon, B., & Davin, B. (2010). Use of formal and informal care services among older people in Ireland and France. The European Journal of Health Economics, 11(5), 499–511.
Geruso, M. (2012). Black-white disparities in life expectancy: How much can the standard SES variables explain? Demography, 49(2), 553–574.
Glaser, K., Price, D., Di Gessa, G., Ribe, E., Stuchbury, R., & Tinker, A. (2013). Grandparenting in Europe: Family policy and grandparents’ role in providing childcare. London: Grandparents Plus.
Glauber, R. (2017). Gender differences in spousal care across the later life course. Research on Aging, 39(8), 934–959.
Gornick, J. C., & Meyers, M. K. (2003). Families that work: Policies for reconciling parenthood and employment. New York: Russell Sage Foundation.
Grigoryeva, A. (2017). Own gender, sibling’s gender, parent’s gender: The division of elderly parent care among adult children. American Sociological Review, 82(1), 116–146.
Gruber, J., & Wise, D. (2000). Social security programs and retirement around the world. Research in labor economics (pp. 1–40). Bingley: Emerald Group Publishing Limited.
Grundy, E., & Henretta, J. C. (2006). Between elderly parents and adult children: A new look at the intergenerational care provided by the ‘sandwich generation.’ Ageing & Society, 26(5), 707–722.
Haberkern, K., Schmid, T., & Szydlik, M. (2015). Gender differences in intergenerational care in European welfare states. Ageing & Society, 35(2), 298–320.
Hank, K., & Buber, I. (2009). Grandparents caring for their grandchildren: Findings from the 2004 Survey of Health, Ageing, and Retirement in Europe. Journal of Family Issues, 30(1), 53–73.
Hochman, O., & Lewin-Epstein, N. (2013). Determinants of early retirement preferences in Europe: The role of grandparenthood. International Journal of Comparative Sociology, 54(1), 29–47.
Hofäcker, D., Stoilova, R., & Riebling, J. R. (2011). The gendered division of paid and unpaid work in different institutional regimes: Comparing West Germany, East Germany and Bulgaria. European Sociological Review, 29(2), 192–209.
Human Fertility Database. Max Planck Institute for Demographic Research (Germany) and Vienna Institute of Demography (Austria). Available at https://www.humanfertility.org (data downloaded on January 30, 2020).
Human Mortality Database. University of California, Berkeley (USA), and Max Planck Institute for Demographic Research (Germany). Available at https://www.mortality.org or https://www.humanmortality.de (data downloaded on May 23, 2019).
Igel, C., & Szydlik, M. (2011). Grandchild care and welfare state arrangements in Europe. Journal of European Social Policy, 21(3), 210–224.
Jacobs, J. C., Laporte, A., Van Houtven, C. H., & Coyte, P. C. (2014). Caregiving intensity and retirement status in Canada. Social Science & Medicine, 102, 74–82.
Jagger, C., Cox, B., Le Roy, S., Clavel, A., Robine, J., Romieu, I., et al. (1999). Health expectancy calculation by the Sullivan method: A practical guide. Montpellier: EHEMU.
Jagger, C., Gillies, C., Moscone, F., Cambois, E., Van Oyen, H., Nusselder, W., & Robine, J.-M. (2008). Inequalities in healthy life years in the 25 countries of the European Union in 2005: A cross-national meta-regression analysis. The Lancet, 372(9656), 2124–2131.
Jang, S.-N., Avendano, M., & Kawachi, I. (2012). Informal caregiving patterns in Korea and European countries: A cross-national comparison. Asian Nursing Research, 6(1), 19–26.
Jappens, M., & Van Bavel, J. (2012). Regional family norms and child care by grandparents in Europe. Demographic Research, 27, 85.
Johnson-Hanks, J. A. (2015). Populations are composed one event at a time. In P. Kreager, B. Winney, S. Ulijaszek, & C. Capelli (Eds.), Population in the human sciences: Concepts, models, evidence (pp. 238–252). OUP Oxford.
Kahn, J. R., McGill, B. S., & Bianchi, S. M. (2011). Help to family and friends: Are there gender differences at older ages? Journal of Marriage and Family, 73(1), 77–92.
Kalmijn, M., & Saraceno, C. (2008). A comparative perspective on intergenerational support: Responsiveness to parental needs in individualistic and familialistic countries. European Societies, 10(3), 479–508.
Leitner, S. (2003). Varieties of familialism: The caring function of the family in comparative perspective. European Societies, 5(4), 353–375.
Leopold, T., Raab, M., & Engelhardt, H. (2014). The transition to parent care: Costs, commitments, and caregiver selection among children. Journal of Marriage and Family, 76(2), 300–318.
Leopold, T., & Skopek, J. (2015). The demography of grandparenthood: An international profile. Social Forces, 94(2), 801–832.
Lewis, J. (1992). Gender and the development of welfare regimes. Journal of European Social Policy, 2(3), 159–173.
Loichinger, E., & Weber, D. (2016). Trends in working life expectancy in Europe. Journal of Aging and Health, 28(7), 1194–1213.
Lumsdaine, R. L., & Vermeer, S. J. (2015). Retirement timing of women and the role of care responsibilities for grandchildren. Demography, 52(2), 433–454.
Lynch, S. M., & Brown, J. S. (2010). Obtaining multistate life table distributions for highly refined subpopulations from cross-sectional data: A Bayesian extension of Sullivan’s method. Demography, 47(4), 1053–1077.
Margolis, R. (2016). The changing demography of grandparenthood. Journal of Marriage and Family, 78(3), 610–622.
Margolis, R., & Verdery, A. M. (2019). A Cohort perspective on the demography of grandparenthood: Past, present, and future changes in race and sex disparities in the United States. Demography, 56(4), 1495–1518.
Margolis, R., & Wright, L. (2017). Healthy grandparenthood: How long is it, and how has it changed? Demography, 54(6), 2073–2099.
Marks, N. F., Lambert, J. D., & Choi, H. (2002). Transitions to caregiving, gender, and psychological well-being: A prospective US national study. Journal of Marriage and Family, 64(3), 657–667.
Mathers, C. D., & Robine, J.-M. (1997). How good is Sullivan’s method for monitoring changes in population health expectancies? Journal of Epidemiology & Community Health, 51(1), 80–86.
Mathers, C. D., Sadana, R., Salomon, J. A., Murray, C. J. L., & Lopez, A. D. (2001). Healthy life expectancy in 191 countries, 1999. The Lancet, 357(9269), 1685–1691.
McKee, M., & Shkolnikov, V. (2001). Understanding the toll of premature death among men in eastern Europe. BMJ, 323(7320), 1051–1055.
Mills, M., Präg, P., Tsang, F., Begall, K., Derbyshire, J., Kohle, L., et al. (2014). Use of childcare in the EU Member States and progress towards the Barcelona targets: Short Statistical Report No. 1.
Montez, J. K., Sabbath, E., Glymour, M. M., & Berkman, L. F. (2014). Trends in work–family context among US women by education level, 1976 to 2011. Population Research and Policy Review, 33(5), 629–648.
Murphy, M., Martikainen, P., & Pennec, S. (2006). Demographic change and the supply of potential family supporters in Britain, Finland and France in the period 1911–2050/Changements démographiques et disponibilité des soutiens familiaux en Grande-Bretagne, en Finlande et en France entre 1911 et 2050. European Journal of Population/Revue Européenne de Démographie, 22(3), 219–240.
Nusselder, W. J., Looman, C. W. N., Van Oyen, H., Robine, J. M., & Jagger, C. (2010). Gender differences in health of EU10 and EU15 populations: The double burden of EU10 men. European Journal of Ageing, 7(4), 219–227.
Oksuzyan, A., Brønnum-Hansen, H., & Jeune, B. (2010). Gender gap in health expectancy. European Journal of Ageing, 7(4), 213–218.
Orloff, A. (1996). Gender in the welfare state. Annual Review of Sociology, 22(1), 51–78.
Patterson, S. E., & Margolis, R. (2019). The demography of multigenerational caregiving: A critical aspect of the gendered life course. Socius, 5, 2378023119862737.
Pfau-Effinger, B. (2005). Culture and welfare state policies: Reflections on a complex interrelation. Journal of Social Policy, 34(1), 3–20.
Raleigh, V. S. (2019). Trends in life expectancy in EU and other OECD countries: Why are improvements slowing? iIn OECD health working papers, No. 108. Paris: OECD Publishing.
Raley, S., Bianchi, S. M., & Wang, W. (2012). When do fathers care? Mothers’ economic contribution and fathers’ involvement in child care. AJS; American Journal of Sociology, 117(5), 1422.
Romero-Ortuno, R., Fouweather, T., & Jagger, C. (2013). Cross-national disparities in sex differences in life expectancy with and without frailty. Age and Ageing, 43(2), 222–228.
Rupert, P., & Zanella, G. (2018). Grandchildren and their grandparents’ labor supply. Journal of Public Economics, 159, 89–103.
Sanderson, W. C., & Scherbov, S. (2015). Are we overly dependent on conventional dependency ratios? Population and Development Review, 41(4), 687–708.
Santos-Eggimann, B., Cuénoud, P., Spagnoli, J., & Junod, J. (2009). Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. The Journals of Gerontology: Series A, 64A(6), 675–681.
Saraceno, C., & Keck, W. (2008). The institutional framework of intergenerational family obligations in Europe: A conceptual and methodological overview. Multilinks project, WP1. Berlin: WZB Social Science Research Center.
Sarasa, S. (2008). Do welfare benefits affect women’s choices of adult care giving? European Sociological Review, 24(1), 37–51.
Sarkisian, N., & Gerstel, N. (2004). Explaining the gender gap in help to parents: The importance of employment. Journal of Marriage and Family, 66(2), 431–451.
Schmid, T., Brandt, M., & Haberkern, K. (2012). Gendered support to older parents: Do welfare states matter? European Journal of Ageing, 9(1), 39–50.
Skoog, G. R., & Ciecka, J. E. (2010). Measuring years of inactivity, years in retirement, time to retirement, and age at retirement within the Markov model. Demography, 47(3), 609–628.
Sobotka, T. (2004). Is lowest-low fertility in Europe explained by the postponement of childbearing? Population and Development Review, 30(2), 195–220.
Spillman, B. C., & Pezzin, L. E. (2000). Potential and active family caregivers: Changing networks and the ‘Sandwich Generation.’ The Milbank Quarterly, 78(3), 347–374.
Sullivan, D. F. (1971). A single index of mortality and morbidity. HSMHA Health Reports, 86(4), 347.
Swartz, T. T. (2009). Intergenerational family relations in adulthood: Patterns, variations, and implications in the contemporary United States. Annual Review of Sociology, 35, 191–212.
Van Bavel, J., & De Winter, T. (2013). Becoming a grandparent and early retirement in Europe. European Sociological Review, 29(6), 1295–1308.
Vlachantoni, A., Evandrou, M., Falkingham, J., & Gomez-Leon, M. (2019). Caught in the middle in mid-life: Provision of care across multiple generations. Ageing & Society, 40, 1490–1510.
Wakabayashi, C., & Donato, K. M. (2005). The consequences of caregiving: Effects on women’s employment and earnings. Population Research and Policy Review, 24(5), 467–488.
Warner, D. F., & Brown, T. H. (2011). Understanding how race/ethnicity and gender define age-trajectories of disability: An intersectionality approach. Social Science & Medicine, 72(8), 1236–1248.
Watkins, S. C., Menken, J. A., & Bongaarts, J. (1987). Demographic foundations of family change. American Sociological Review, 52, 346–358.
Yang, Y. (2008). Long and happy living: Trends and patterns of happy life expectancy in the US, 1970–2000. Social Science Research, 37(4), 1235–1252.
Acknowledgements
The authors gratefully acknowledge research support from the Center for Demography and Ecology and the Center for the Demography of Health and Aging at the University of Wisconsin-Madison, which, respectively, receive core support from the National Institute of Child Health and Human Development (P2C HD047873) and the National Institute on Aging (P30 AG17266). The second author additionally received support from the NIA (T32 AG00129) and NICHD (T32 HD007014; R21HD101757: PI McDade). An earlier version of this manuscript was presented at the 2018 meeting of the Population Association of America. The authors thank Ashton Verdery, Michal Engelman, James Raymo, Jenna Nobles, Jason Fletcher, Marcy Carlson, and the participants of the FemSem brown bag at the University of Wisconsin-Madison for their helpful comments on various versions of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ophir, A., Polos, J. Care Life Expectancy: Gender and Unpaid Work in the Context of Population Aging. Popul Res Policy Rev 41, 197–227 (2022). https://doi.org/10.1007/s11113-021-09640-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11113-021-09640-z