Abstract
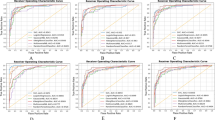
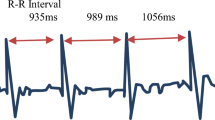
Imbalance in the autonomic nervous system can lead to orthostatic intolerance manifested by dizziness, lightheadedness, and a sudden loss of consciousness (syncope); these are common conditions, but they are challenging to diagnose correctly. Uncertainties about the triggering mechanisms and the underlying pathophysiology have led to variations in their classification. This study uses machine learning to categorize patients with orthostatic intolerance. We use random forest classification trees to identify a small number of markers in blood pressure, and heart rate time-series data measured during head-up tilt to (a) distinguish patients with a single pathology and (b) examine data from patients with a mixed pathophysiology. Next, we use Kmeans to cluster the markers representing the time-series data. We apply the proposed method analyzing clinical data from 186 subjects identified as control or suffering from one of four conditions: postural orthostatic tachycardia (POTS), cardioinhibition, vasodepression, and mixed cardioinhibition and vasodepression. Classification results confirm the use of supervised machine learning. We were able to categorize more than 95% of patients with a single condition and were able to subgroup all patients with mixed cardioinhibitory and vasodepressor syncope. Clustering results confirm the disease groups and identify two distinct subgroups within the control and mixed groups. The proposed study demonstrates how to use machine learning to discover structure in blood pressure and heart rate time-series data. The methodology is used in classification of patients with orthostatic intolerance. Diagnosing orthostatic intolerance is challenging, and full characterization of the pathophysiological mechanisms remains a topic of ongoing research. This study provides a step toward leveraging machine learning to assist clinicians and researchers in addressing these challenges.

Machine learning tools utilized to analyze heart rate (HR) and blood pressure (BP) time-series data from syncope and control patients. Results show that machine learning can provide accurate classification of disease groups for 98% of patients and we identified two subgroups within the control patients differentiated by their BP response.







Similar content being viewed by others
References
Bartoletti A, Alboni P, Ammirati F, Brignole M, Del Rosso A, Manzillo G, Menozzi C, Raviele A, Sutton R (2000) The Italian protocol: a simplified head-up tilt testing potentiated with oral nitroglycerin to assess patients with unexplained syncope. Europace 2(4):339–342
Breiman L (2001) Random forests. Mach Learn 45:5–32
Brennan M, Palaniswami M, Kamen P (2001) Do existing measures of poincaré plot geometry reflect nonlinear features of heart rate variability? Cureus 48(11):1342–1347
Brignole M (2007) Diagnosis and treatment of syncope. Heart 93(1):130–136
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Thomsen PB, van Dijk J, Fitzpatrick A, Hohnloser S, Janousek J, Kapoor W, Kenny R, Kulakowski P, Masotti G, Moya A, Raviele A, Sutton R, Theodorakis G, Ungar A, Wieling W (2004) Guidelines on management (diagnosis and treatment) of syncope. Eurospace 6(6):467–573
Brignole M, Moya A, de Lange F, Deharoa JC, Elliott M, Fanciulli A, Federowski A, Furlan R, Kenny R, Martin A, Probst V, Reed M, Rice C, Sutton R, Ungar A, van Dijk J (2018) 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J 39(21):1883–1948
Brignole M, Ungar A, Casagranda I, Gulizia M, Lunati M, Ammirati F, Del Rosso A, Sasdelli M, Santini M, Maggi R, Vitale E, Morrione A, Francese G, Vecchi M, Giada F (2010) Syncope Unit (SUP) investigators: prospective multicentre systematic guideline-based management of patients referred to the syncope units of general hospitals. Europace 12(1):109–118
Cubera K, Stryjewski P, Kuczaj A, Nessler J, Nowalany-Kozielska E, Pytko-Polonzyk J (2017) The impact of gender on the frequency of syncope provoking factors and prodromal signs in patients with vasovagal syncope. Przeglad Lekarski 74(4):147–149
Ferreira R, da Silva L (2016) The current indication for pacemaker in patients with cardioinhibitory vasovagal syncope. Open Cardiovasc Med J 10:179–187
Fletcher J (2020) What to know about vasovagal syncope. https://www.medicalnewstoday.com/articles/327406
Fu Q, Vangundy T, Galbreath M, Shibata S, Jain M, Hastings J, Bhella P, Levine B (2010) Cardiac origins of the postural orthostatic tachycardia syndrome. J Am Coll Cardiol 55(25):2858–2868
Furlan R, Diedrich A, Rimoldi A, Palazzolo L, Porta C, Diedrich L, Harris P, Sleight P, Biagioni I, Robertson D, Bernardi L (2003) Effects of unilateral and bilateral carotid baroreflex stimulation on cardiac and neural sympathetic discharge oscillatory patterns. Circulation 108(6):717–723
Furlan R, Jacob G, Snell M, Robertson D, Porta A, Parris P, Mosqueda-Garcia R (1998) Chronic orthostatic intolerance: a disorder with discordant cardiac and vascular sympathetic control. Circulation 98(20):2154–2159
Geddes J, Mehlsen J, Olufsen M (2020) Characterization of blood pressure and heart rate oscillations in pots patients via uniform phase empirical mode decomposition. IEEE Trans Biomed Eng 67(11):3016–3025
Greve Y, Geier F, Popp S, Bertsch T, Singler K, Meier F, Smolarsky A, Mang H, Müller C, Christ M (2014) The prevalence and prognostic significance of near syncope and syncope: a prospective study of 395 cases in an emergency department (the speed study). Dtsch Arztebl Int 111(12):197–204
Guyton A, Hall J (2016) Medical physiology, 13th edn. Elsevier, Philadelphia
Hastie T, Tibshirani R, Friedman J (2009) The elements of statistical learning. Springer Series in Statistics. Springer, New York
Jacob G, Barbic F, Glago M, Dipaola F, Porta A, Furlan R (2018) Cardiovascular autonomic profile in women with constitutional hypotension. J Hypertens 36(10):2068–2076
Khodor N (2014) Dynamical analysis of mutivariate time series for the early detection of syncope during head-up tilt test. Ph.D. thesis, Université Rennes 1, Rennes, France
Khodor N, Carrault G, Matelot D, Amoud H, Khalil M, Boullay N, Carré F, Hernandez A (2016) Early syncope detection during head up tilt test by analyzing interactions between cardio-vascular signals. Dig Signal Process 49:86–94
Klemenc M, Strumbelj E (2015) Predicting the outcome of head-up tilt test using heart rate variability and baroreflex sensitivity parameters in patients with vasovagal syncope. Clinical Autonomic Res 25 (6):391–398
Kuran A, Erickson M, Petersen M, Franzen A, Williams T, Sutton R (2000) Respiratory changes in vasovagal syncope. J Cardiovasc Electrophysiol 11(6):607–611
Kurbaan A, Bowker T, Wijesekera N, Heaven D, Itty S, Sutton R (2003) Age and hemodynamic responses to tilt testing in those with syncope of unknown origin. J Am Coll Cardiol 41(6):1004–1007
Li H, Liao Y, Han Z, Wang Y, Liu P, Zhang C, Tang C, Du J, Jin H (2018) Head-up tilt test provokes dynamic alterations in total peripheral resistance and cardiac output in children with vasovagal syncope. Acta Paediatr 107(10):1786–1791
Mark A (1983) The bezold-jarisch reflex revisited: clinical implications of inhibitory reflexes originating in the heart. JAJCC 1(1):69–72
Mehlsen J, Kaijer M, Mehlsen AB (2008) Autonomic and electrocardiographic changes in cardioinhibitory syncope. Europace 10(1):91–95
Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm J, Deharo JC, Gajek J, Gjesdal K, Krahn A, Massin M, Pepi M, Pezawas T, Ruiz Granell R, Sarasin F, Ungar A, van Dijk J, Walma E, Wieling W (2009) Guidelines for the diagnosis and management of syncope (version 2009). Europ Heart J 30:2631–2671
Ocon A, Medow M, Taneja I, Stewart J (2011) Respiration drives phase synchronization between blood pressure and rr interval following loss of cardiovagal baroreflex during vasovagal syncope. Am J Physiol 300(2):H527–H540
Parati G, Bretinieri M, Pomidossi G, Casadei R, Groppeli A, Pedotti A, Zanchetti A, Mancia G (1988) Evaluation of the baroreceptor-heart rate reflex by 24-hour intra-arterial blood pressure monitoring in humans. Hypertension 12(2):214– 222
Parlow J, Viale J, Annat G, Hughson R, Quintin L (1995) Spontaneous cardiac baroreflex in humans: comparison with drug-induced responses. Hypertension 25(5):1058–1068
Probst M, Kanzaria H, Gbedemah M, Richardson L, Sun B (2015) National trends in resource utilization associated with ed visits for syncope. American. J Emergency Med 33(8):998–1001
Randall E, Billeschou A, Brinth L, Mehlsen J, Olufsen M (2019) A model-based analysis of autonomic nervous function in response to the valsalva maneuver. J Appl Physiol 127(5):1386– 1402
Randall E, Randolph N, Olufsen M (2020) Persistent instability in a nonhomogeneous delay differential equation system of the valsalva maneuver. Math Biosci 319:108292
Remmen J, Aengevaeren W, Verheugt F, van ver Werf T, Luijten H, A Bos RJ (2002) Finapres arterial pulse wave analysis with modelflow is not a reliable non-invasive method for assessment of cardiac output. Clin Sci (Lond) 103(2):143–149
Robertson D, Biaggioni I, Low P (2011) Primer on the autonomic nervous system, 3rd edn. Elsevier, London
Romme J, van Dijk N, Boer K, Dekker L, Stam J, Reitsma J, Wieling W (2008) Influence of age and gender on the occurrence and presentation of reflex syncope. Clin Autonom Res 28(3):127–133
Rousseeuw P (1987) Silhouettes: a graphical aid to the interpretation and validation of cluster analysis. J Comp Appl Math 20:53–65
Sander-Jensen K, Mehlsen J, Stadeager C, Christensen N, Fahrenkrug J, Schwartz T, Warberg J, Bie P (1988) Increase in vagal activity during hypotensive lower-body negative pressure in humans. Am J Physiol 255(1 Pt 2):R149–R156
Sheldon R, Grubb B, Olshansky B (2015) 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 12(6):e41–e63
van Dijk J, Thijs R, Benditt D, Wieling W (2009) A guide to disorders causing transient loss of consciousness: focus on syncope. Nat Rev Neurol 5(8):438–448
Virag N, Sutton R, Vetter R, Markowitz T (2007) Prediction of vasovagal syncope from heart rate and blood pressure trend and variability: experience in 1,155 patients. Heart Rhythm 4(11):1375–1382
Vlasta B, Marchi A, De Maria B, Rossato G, Nollo G, Faes L, Porta A (2016) Nonlinear effects of respiration on the crosstalk between cardiovascular and cerebrovascular systems. Philos Trans A Math Phys Eng Sci 374(2067):2015079
Williams N, Wind-Willassen O, Wright A, Program R, Mehlsen J, Ottesen J, Olufsen M (2014) Patient-specific modelling of head-up tilt. Math Med Biol 31(4):365–392
Acknowledgements
The authors would like to thank the Statistical and Applied Mathematical Sciences Institute (SAMSI), where this work was initiated, and Peter Novak, Brigham and Women’s Hospital, Boston, MA 02115, for helpful discussions.
Funding
This work was supported in part by the National Institutes of Health and the National Science Foundation under Grants NSF-DMS 1557761 and NSF-DMS-1745654 and the National Institutes of Health through grant NIH 5P50GM094503-06 VPR sub-award to North Carolina State University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer
This paper describes objective technical results and analysis. Any subjective views or opinions that might be expressed in the paper do not necessarily represent the views of the U.S. Department of Energy or the United States Government. Sandia National Laboratories is a multimission laboratory managed and operated by National Technology and Engineering Solutions of Sandia LLC, a wholly owned subsidiary of Honeywell International, Inc., for the U.S. Department of Energy’s National Nuclear Security Administration under contract DE-NA-0003525. SAND2020-2937 J.
Rights and permissions
About this article
Cite this article
Gilmore, S., Hart, J., Geddes, J. et al. Classification of orthostatic intolerance through data analytics. Med Biol Eng Comput 59, 621–632 (2021). https://doi.org/10.1007/s11517-021-02314-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-021-02314-0