Abstract
Intensity-modulated radiation therapy (IMRT) is a type of external beam radiation therapy used in cancer treatment. In IMRT, the prescribed radiation dose can be administered such that it is maximized on the cancerous tumor while sparing the surrounding healthy tissues. The total dose is divided into fractions across time intervals, called a fractionation scheme. To find the best fractionation scheme and beamlet intensities for total dose, optimization models are used. In this paper, a non-convex mixed-integer nonlinear programming model has been proposed wherein the spatiotemporal changes of the biological properties of the tumor due to tumor cell re-oxygenation, redistribution, and re-population that occur as the treatment progresses have been considered. Also, the dose constraints over both cumulative limits and per-fraction limits have been considered in the model. The output of this model is called the fractionation scheme and beamlet intensities considering biological changes in tumor cells (FBBTs). When the FBBTs are compared with conventional fractionation scheme and beamlet intensities (CFB) which do not include the biological properties of the tumor, it is observed that the FBBTs are more efficacious than the CFBs. To get FBBTs for datasets that resemble realistic tumors, an algorithm based on simulated annealing has been developed and used.



Similar content being viewed by others
References
Aleman D, Kumar A, Ahuja R, Romeijn HE, Dempsey J (2008) Neighborhood search approaches to beam orientation optimization in intensity modulated radiation therapy treatment planning. J Glob Optim 42:587–607
Bertsimas D, Cacchiani V, Craft D, Nohadani O (2013) A hybrid approach to beam angle optimization in intensity-modulated radiation therapy. Comput Oper Res 40:2187–2197
Bortfeld, T, Ramakrishnan J, Tsitsiklis JN, Unkelbach J (2013) Optimization of radiation therapy fractionation schedules in the presence of tumor repopulation. arXiv preprint arXiv:1312.1332
Dink D, Langer M, Orcun S, Pekny J, Rardin R, Reklaitis G, Saka B (2011) IMRT optimization with both fractionation and cumulative constraints. Am J Oper Res 1(3):160–171
Ehrgott M, Güler Ç, Hamacher HW, Shao L (2010) Mathematical optimization in intensity modulated radiation therapy. Ann Oper Res 175(1):309–365
Fowler JF (1989) The linear-quadratic formula and progress in fractionated radiotherapy. Br J Radiol 62(740):679–694
Hall EJ, Giaccia AJ (2005) Radiobiology for the radiologist. Lippincott Williams and Wilkins, Philadelphia
Kim M, Ghate A, Phillips MH (2012) A stochastic control formalism for dynamic biologically conformal radiation therapy. Eur J Oper Res 219(3):541–556
Kirkpatrick S, Gelatt CD, Vecchi MP (1983) Optimization by simulated annealing. Science 220(4598):671–680
Melouk S, Damodaran P, Chang P-Y (2004) Minimizing makespan for single machine batch processing with non-identical job sizes using simulated annealing. Int J Prod Econ 87(2):141–147
Morrill S, Lane R, Rosen I (1990) Constrained simulated annealing for optimized radiation therapy treatment planning. Comput Methods Programs Biomed 33:135–144
Niemierko A (1992) Random search algorithm (RONSC) for optimization of radiation therapy with both physical and biological end points and constraints. Int J Radiat Oncol Biol Phys 23:89–98
Pawlik TM, Keyomarsi K (2004) Role of cell cycle in mediating sensitivity to radiotherapy. Int J Radiat Oncol Biol Phys 59:928–942
Powathil G, Kohandel M, Milosevic M, Sivaloganathan S (2012) Modeling the spatial distribution of chronic tumor hypoxia: implications for experimental and clinical studies. Comput Math Methods Med 2012:410602
Powathil GG, Adamson DJ, Chaplain MA (2013) Towards predicting the response of a solid tumour to chemotherapy and radiotherapy treatments: clinical insights from a computational model. PLoS Comput Biol 9(7):e1003120
Robert Fourer DMG, Kernighan BW (1990) A modeling language for mathematical programming. Manag Sci 36:519–554
Ruggieri R, Naccarato S, Nahum AE (2010) Severe hypofractionation: non-homogeneous tumour dose delivery can counteract tumour hypoxia. Acta Oncol 49(8):1304–1314
Saka B, Rardin RL, Langer MP, Dink D (2011) Adaptive intensity modulated radiation therapy planning optimization with changing tumor geometry and fraction size limits. IIE Trans Healthc Syst Eng 1(4):247–263
Saka B, Rardin RL, Langer MP (2014) Biologically guided IMRT planning optimization. J Oper Res Soc 65(4):557–571
Shepard DM, Ferris MC, Olivera GH, Mackie TR (1999) Optimizing the delivery of radiation therapy to cancer patients. SIAM Rev 41(4):721–744
Stewart BW, Wild CP (eds) (2014) World cancer report. International Agency for Research on Cancer, Lyon
Tawarmalani M, Sahinidis VN (2005) A polyhedral branch-and-cut approach to global optimization. Math Program 103(2):225–249
Webb S (1992) Optimization by simulated annealing of three-dimensional, conformal treatment planning for radiation fields defined by a multileaf collimator: II. Inclusion of two-dimensional modulation of the x-ray intensity. Phys Med Biol 37:1689–1704
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Analysis of the scaling factor s
The instances of small datasets that could be solved to optimality by the BARON solver are used to find the effect of changing values of scaling factor s on the objective function values of the optimal FBBTs (Table 9).
The values of the objective functions do not change for any of the instances with the changes in the s values. This suggests that the optimal FBBTs can be obtained using any value of s.
Appendix 2
Detailed result of instance number 2 in Table 2 of small datasets
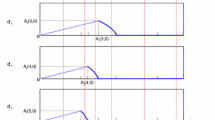
The first attempt was to find the FBBT by the BARON solver and get an exact solution. The dose deposition values and the number of tumor cells left over after every treatment session are given in Table 10. It can be seen that as tumor point T3 is heterogeneous with a higher number of tumor cells at the start, the total dose deposited on the same in the entire treatment is higher than that on the other tumor points.
After the 6th treatment session, there are still tumor cells left that are larger in number than the acceptable limit b. Hence, N is updated to \(N + 5\). But the solver does not give any solution in the computational time limit of 2 h. So the data of the instance are passed to the model based on SA with \(N = 11\). With the parameters mentioned in “FBBT of small datasets” section, a solution is obtained in 1.53 h but with number of tumor cells left over after treatment greater than b. Again the SA model is solved with \(N = 16\). Table 11 gives the dose depositions and the number of tumor cells left over after every treatment session. Although the obtained FBBT is near optimal, the solution time is 1.49 h and number of tumor cells left over after the 14th treatment session is lesser than b which is the actual target of the treatment planning. Hence, only 14 treatment sessions are conducted in all. Here again the total dose deposited on the tumor point T3 is higher than that on the other tumor points.
Rights and permissions
About this article
Cite this article
Ghatkar, S. Optimization of fractionation schemes and beamlet intensities in intensity-modulated radiation therapy with changing cancer tumor properties. Decision 46, 385–407 (2019). https://doi.org/10.1007/s40622-019-00229-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40622-019-00229-2