Published online Dec 26, 2020. doi: 10.4252/wjsc.v12.i12.1474
Peer-review started: June 23, 2020
First decision: July 30, 2020
Revised: August 13, 2020
Accepted: September 25, 2020
Article in press: September 25, 2020
Published online: December 26, 2020
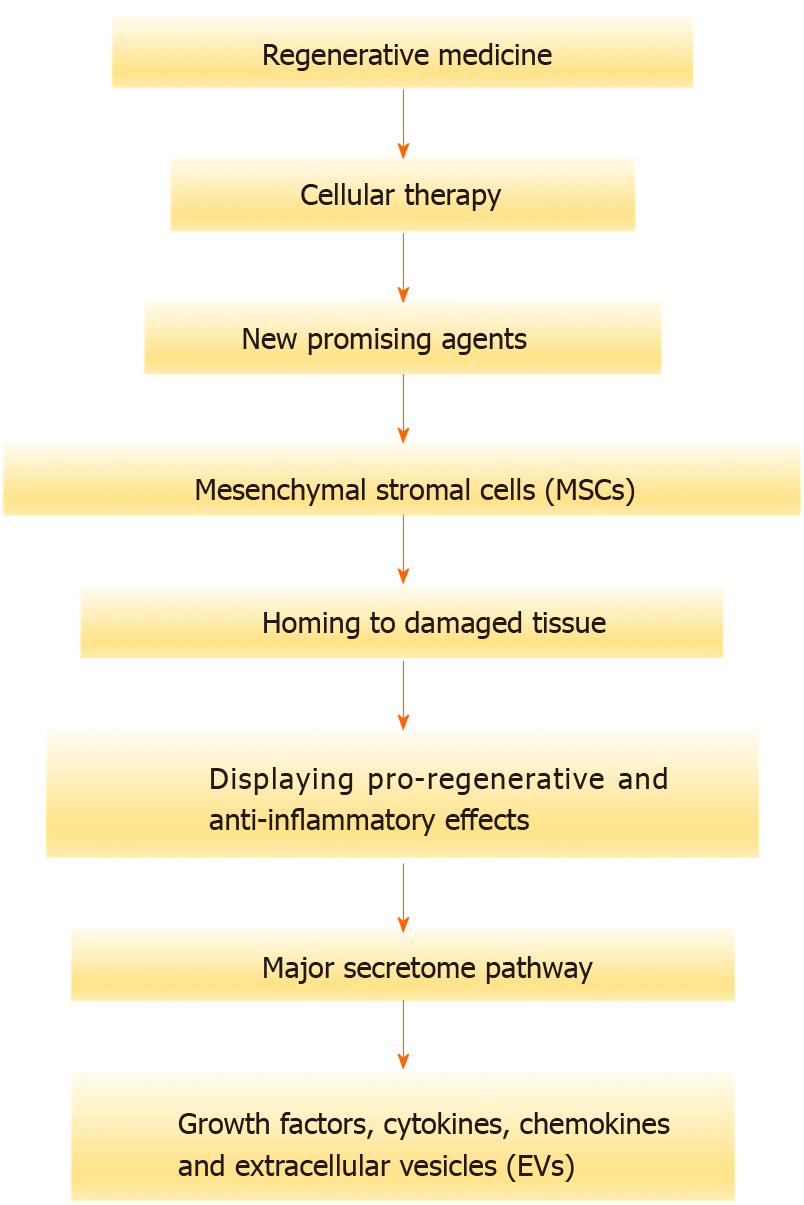
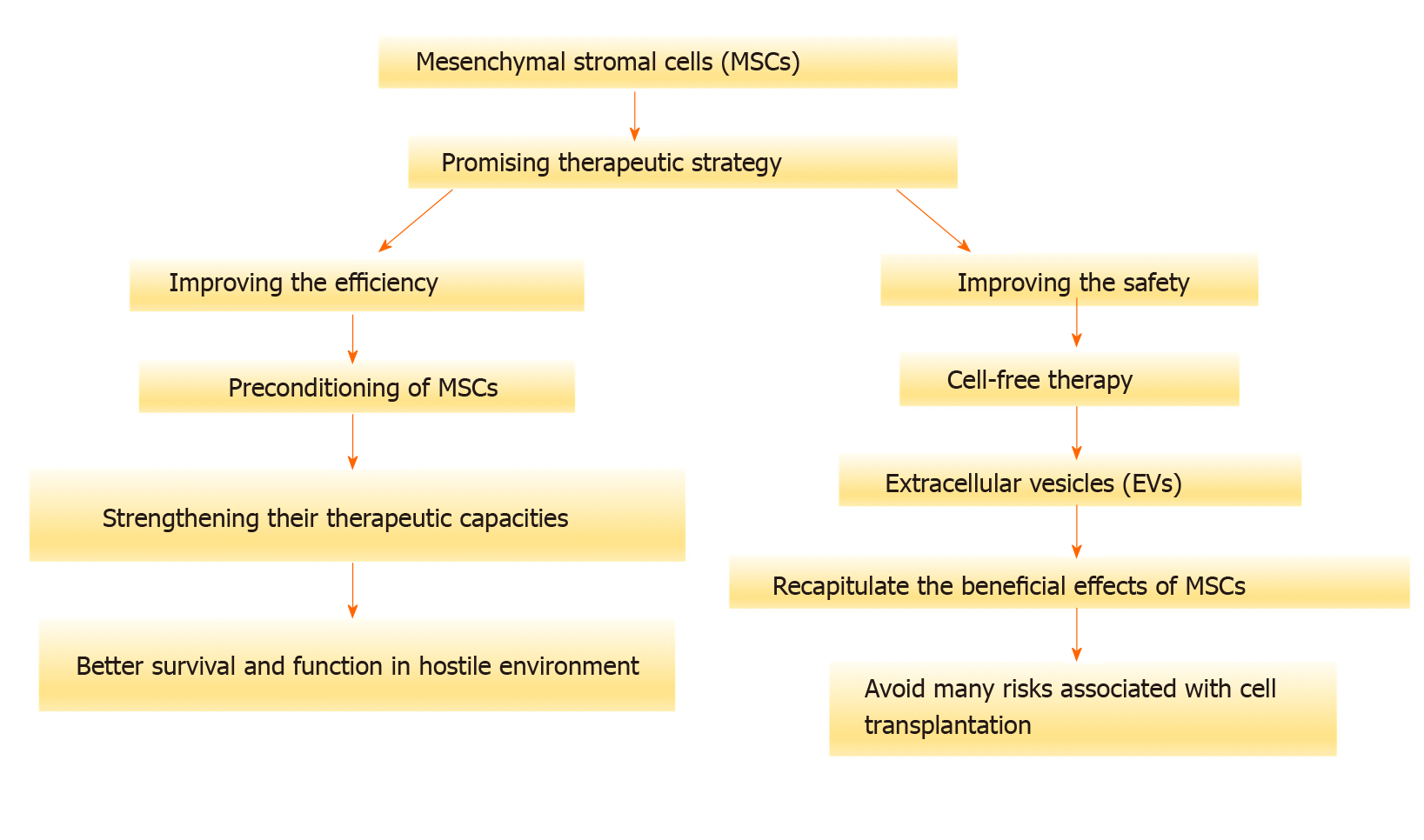
Mesenchymal stromal cells (MSCs) have attracted great interest in the field of regenerative medicine. They can home to damaged tissue, where they can exert pro-regenerative and anti-inflammatory properties. These therapeutic effects involve the secretion of growth factors, cytokines, and chemokines. Moreover, the functions of MSCs could be mediated by extracellular vesicles (EVs) that shuttle various signaling messengers. Although preclinical studies and clinical trials have demonstrated promising therapeutic results, the efficiency and the safety of MSCs need to be improved. After transplantation, MSCs face harsh environmental conditions, which likely dampen their therapeutic efficacy. A possible strategy aiming to improve the survival and therapeutic functions of MSCs needs to be developed. The preconditioning of MSCs ex vivo would strength their capacities by preparing them to survive and to better function in this hostile environment. In this review, we will discuss several preconditioning approaches that may improve the therapeutic capacity of MSCs. As stated above, EVs can recapitulate the beneficial effects of MSCs and may help avoid many risks associated with cell transplantation. As a result, this novel type of cell-free therapy may be safer and more efficient than the whole cell product. We will, therefore, also discuss current knowledge regarding the therapeutic properties of MSC-derived EVs.
Core Tip: Mesenchymal stromal cells (MSCs) have a strong capacity to regenerate injured tissues by displaying trophic and immunomodulatory functions. The tissue environment plays a significant role during the reparative process of MSCs. Preconditioning of MSCs with a specific signal promotes the adequate response. As the therapeutic functions of MSCs are mainly linked to their secretome, the use of extracellular vesicles as an acellular tool is strongly recommended. Thus, new insights on the properties of MSCs as well as their mechanisms of actions will help to develop a safe and efficient therapeutic strategy.
- Citation: Najar M, Martel-Pelletier J, Pelletier JP, Fahmi H. Novel insights for improving the therapeutic safety and efficiency of mesenchymal stromal cells. World J Stem Cells 2020; 12(12): 1474-1491
- URL: https://www.wjgnet.com/1948-0210/full/v12/i12/1474.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v12.i12.1474
Due to the high prevalence of tissue injury and damage, new therapeutic strategies should be considered[1]. Tissue regeneration is a complex process encompassing several interplays between tissue progenitor/stem cells, local environment, and immune cells. The healing ability is generally attributable to a pool of undifferentiated cells capable of replacing damaged cells in order to guarantee the integrity of the tissue[2]. These cells can sense several signals of injury and damage, which can in turn modulate their biological features. However, the pool of tissue-specific stem/stromal and progenitor cells may show functional exhaustion. Depending on the injury and damage, these endogenous cells may display low efficiency regarding their healing mechanism. Impairments of cell self-renewal, function, differentiation capacity, and homing may thus be observed[3].
New therapies using ex vivo-expanded stem/stromal and progenitor cells have been developed to enhance the healing process. In this context, mesenchymal stromal cells (MSCs) have been reported as an attractive candidate for cell therapy. Originally identified within the bone marrow niche, MSCs were subsequently identified in different tissues. Morphologically similar to fibroblasts, MSCs are characterized in vitro by plastic-adherent proliferation, a specific immunophenotype and multipotency as defined by the International Society for Cellular Therapy (ISCT)[4]. They express CD73, CD90 and CD105 and lack the expression of CD14, CD19, CD34, CD45 and human leukocyte antigen (HLA)-DR. To date, their multipotent capabilities have not been clearly demonstrated in vivo, particularly because of the lack of methods to identify and define differentiated populations. However, the trophic and immunomodulatory properties of MSCs are likely the key attributes that mediate tissue repair[5,6].
In parallel, harsh environments within damaged and diseased tissues such as ischemia, inflammatory/immunological reactions, oxidative stress, and infectious episodes may influence the fate and functions of cells[7]. By sensing such signals, MSCs respond by migrating, proliferating, and initiating regenerative mechanisms. MSCs will try to reconstitute the immune microenvironment and empower tissue stem/progenitor cells and other resident cells, thereby facilitating tissue repair[8]. A rapid detection of the primary insult allows to display the adequate response attempting repair[9]. In general, a tight regulation of the balance between the native and activated states of MSCs appears essential for their functional properties during tissue repair. It has been shown that MSCs require specific signals to display adequate therapeutic potential[10]. Such behavior indicates that MSCs possess functional plasticity, and that, under specific conditions, it is possible to polarize their biological response toward an adequate response. Depending on tissue injury or disease conditions, the secretome may change allowing MSCs to exert different effects. These changes generally modulate the type and level of cytokines and growth factors important for the tissue repair process[11]. The results obtained from clinical applications of MSCs indicate that therapeutic outcomes could be improved. The secretome of MSCs is mainly responsible for the modulation of immune responses and the function empowerment of local progenitors. It consists of a diverse range of growth factors, cytokines, chemokines, and extracellular vesicles (EVs) that govern different paracrine signaling. MSCs convey regulatory messages to recipient cells to initiate tissue repair[6]. The release of EVs has emerged as an important mediator of cell-to-cell communication. They have been shown to effectively mimic the effects of MSCs, thus participating in their therapeutic process. In fact, EVs may transfer proteins, lipids, and genetic material, which also contribute to the modulation of the biology and fate of recipient cells, without requiring the presence of MSCs. The use of this cell-free tool would certainly enhance the safety of MSC-based therapy (Figure 1).
The safety and efficiency of MSCs are the two major aspects that need to be managed to improve the therapeutic effects of MSCs[4]. These two goals are closely linked to their acellular component and preconditioning strategy, respectively. A broader understanding of the tissue environment characteristics and components that allow to modulate the plasticity of MSCs and therefore set up more specific MSC responses by using preconditioning strategies. Here, we focus on the influences of inflammatory and infectious signals, mostly found within the injured tissue, on several features of MSCs. The secretome of MSCs, in particular EVs, make them an attractive tool as cell-free based therapy. More insight into the biology, production, composition and role of EVs would increase the quality and safety of the therapy. Of note, preconditioning should be applied to enhance the production of EVs as well as empower their effects by maximizing their contents of regulatory and trophic factors. This deeper understanding would improve the capacity to manipulate MSCs and ultimately lead to safer and more efficient therapeutic effects (Figure 2).
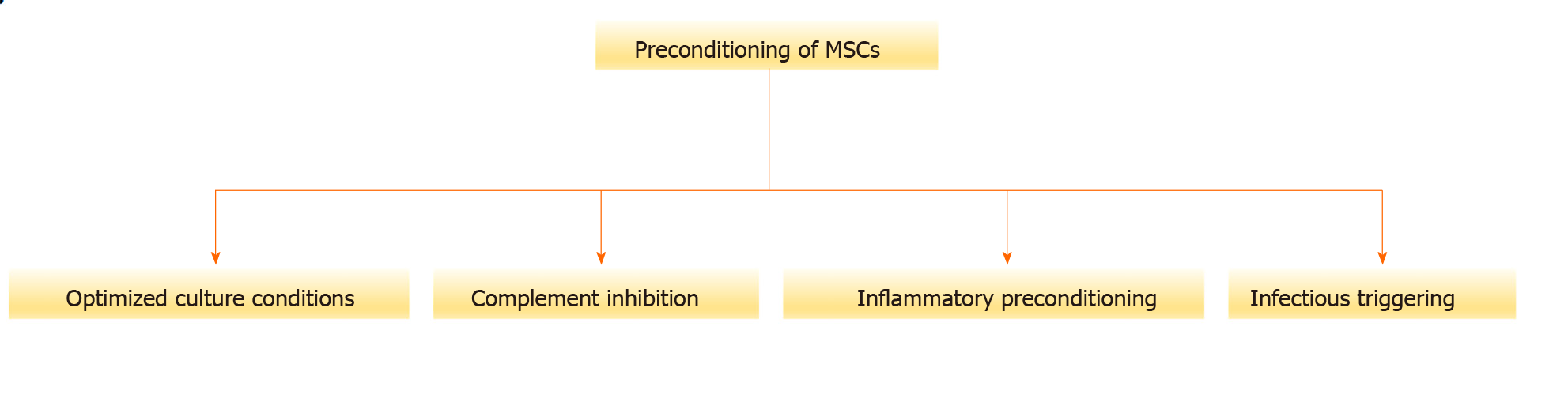
The cellular and molecular tissue microenvironment is a dynamic compartment where several signals can modulate MSC features[12]. The balance between the physiological and pathological states of the tissue critically influences the reparative process. After injection, MSCs can migrate into the injured tissues where they encounter an unfavorable environment coupled with death signals, infections, oxidative stress, and immune/inflammatory responses[13]. Moreover, clinical data suggest that the outcomes of MSC-based therapy are affected by medication or the presence of infections[14]. Hurdles including poor homing, survival, engraftment, and functions may hamper the therapeutic effect of transplanted MSCs[15]. In the quest to circumvent these challenges, several strategies can be utilized including preincubation with growth factors, cytokines, receptor agonists, optimization of culture conditions (e.g., hypoxia, glucose), and the use of bioactive or biomimetic scaffolds[16,17]. Also called licensing or priming, these strategies may be considered as cell preconditioning (Figure 3).
It consists of boosting cells for a specific function in a specific challenging environment[18]. The goal is to not only maintain, but also enhance the inherent biological activities and therapeutics effects of MSCs with respect to migration, homing to target site, tissue engraftment, survival, and improved reparative/trophic functions[19-24]. Thus, these features should be carefully evaluated in vitro and in vivo[24]. Overall, MSCs should withstand the inhospitable environment in the recipient tissue (transplanted cell-preconditioning). At the same time, the damaged tissue becomes more receptive to the transplanted cells favoring their engraftment and interplay (tissue-preconditioning)[21]. Such development may accelerate the process to translate experimental evidence from preclinical studies to daily clinical practice[22].
After isolation, MSC are typically cultured under normoxic conditions (21% oxygen). However, the physiological niches for MSC in the bone marrow and other sites have much lower oxygen tension. When used as a therapeutic tool to repair tissue injuries, MSCs cultured in standard conditions must adapt from 21% oxygen in culture to less than 1% oxygen in the ischemic tissue[23]. Several data suggest that preculturing MSCs under hypoxic conditions prior to transplantation improves their tissue regenerative potential. Interestingly, hypoxia pretreatment significantly increased the proliferation and chondrogenic differentiation of adipose tissue-derived stem cells but decreased their osteogenic differentiation in a vascular endothelial growth factor (VEGF)-dependent manner[25]. In parallel, hypoxia-preconditioned olfactory mucosa mesenchymal stem cells inhibits pyroptotic and apoptotic death of microglial cell in response to cerebral ischemia/reperfusion insult by activating hypoxia-inducible factor-1 (HIF-1) in vitro[26]. Hypoxia preconditioning of human dental MSCs empowers their immunoregulatory functions. Overexpression of HIF-1α leads to the modulation of the adaptive and innate immune responses. Following an increase of C-C motif chemokine ligand 2 (CCL2, also referred to as monocyte chemoattractant protein-1) production, monocytes are significantly recruited and induced to acquire M2 macrophage phenotypes known for their immunosuppressive properties[27]. These effects could be linked to the expression of interleukin (IL)-10 and Fas-ligand. Indeed, the IL-10/CD210 axis is functionally relevant during immunomodulation by regulating several features of T cell response[28].
Because melatonin exhibits antioxidant and anti-inflammatory properties, it has been used as a preconditioning tool to optimize the response of MSCs within a unreceptive microenvironment[29]. Preconditioning of rat bone marrow (BM)-MSCs by omentin-1, a fat depot-specific secretory adipokine, allowed to display improved therapeutic functions. Such a condition promotes proliferation, inhibits apoptosis, increases secretion of angiogenic factors, and enhances the ability to stimulate tube formation by human umbilical vein endothelial cells via the PI3K/AKT signaling pathway[30]. In line with this, ex vivo antioxidant preconditioning by using n-acetylcysteine and ascorbic acid 2-phosphate improved the viability of MSCs and protected them in the presence of diabetic wound fluid[31]. The preconditioning of MSCs by glutathione-allylsulfur conjugates can enhance their survival after post-ischaemic myocardial implantation. In a concentration dependent manner, such treatment increased the proliferation, migration, and differentiation of cardiac lineage marker-negative/stem cell antigen-1-positive human mesenchymal stem cells. These beneficial effects are consecutive to the upregulation of proteins involved in oxidative stress protection, cell-cell adhesion, and commitment to differentiation[32].
Recently, treatment of human decidua basalis MSCs with a high level of glucose was shown to enhance the engraftment and therapeutic potential of MSCs. Preconditioning with glucose increased gene expression related to survival, proliferation, migration, invasion, and immunomodulatory properties[33]. Glutamine (GLUT) is a nonessential amino acid that can become conditionally essential under stress conditions, being able to participate in the modulation of the immune responses in several ways. GLUT has been reported to enhance the immunosuppressive properties of MSCs. In a dose dependent manner, the addition of GLUT augmented the proliferation of MSCs, reduced lymphocyte and macrophage proliferation. This effect was probably reached by decreasing levels of pro-inflammatory cytokines and by increasing levels of anti-inflammatory cytokines[34].
The use of biomaterial scaffolds may lead to higher clinical benefits in patients treated by MSCs. Triggering the expression of cytoprotective genes that aim at enhancing the longevity of MSCs and the duration of their regulatory effects is a very promising strategy[10]. MSC-biomaterial constructs retain MSCs in situ and prolong their survival. Moreover, biomaterial scaffolds can both preserve the tissue architecture and provide a three-dimensional biomimetic milieu for embedded MSCs, which enhance their paracrine functions[35]. In accordance with these achievements, our group accomplished a cutting-edge feat by developing a feasible, safe and physiological process that increases the level of MSCs in the BM niche with a specific commitment[36]. Injection of autologous platelet-rich plasma activated by the recombinant human soluble tissue factor in the iliac crest, enhanced the production of autologous MSCs. This strategy avoids the use of allogeneic MSCs and the need of their expansion through ex vivo culture with the accompanying risks of contamination and cell differentiation.
The viability and/or function of MSCs seems to be altered as they may undergo a complement-dependent lysis. Results indicate that the complement system is integrally involved in recognizing and injuring MSCs after their infusion[37]. MSCs activate the complement system, which triggers complement-mediated lymphoid and myeloid effector cell activation in blood. MSCs were found to present complement component (C3)-derived fragments inactivated C3b (iC3b) and C3dg and to generate complement-derived anaphylatoxins (C3a and C5a) with chemotactic activity[38]. It has been suggested that complement anaphylatoxins C3a and C5a participate in activation and recruitment of MSCs to sites of tissue damage and repair[39]. Of importance, complement bound to MSC enhanced their phagocytosis by classical and intermediate monocytes which may explain, at least in part, why MSCs are not found in the blood circulation after infusion[40]. The inhibition of complement activation has been proposed for improving the outcome of MSC-based therapy. Thus, cell-surface engineering of MSCs with heparin has been shown to improve their viability and enhance their function after infusion. Heparin by directly inhibiting the complement protein and by recruiting factor H inhibited complement activation on MSCs[41]. Of note, treatment of MSCs with all-trans retinoic acid protected them from immune thrombocytopenia by regulating the complement-IL-1β loop. All-trans retinoic acid increased the number and improved the function of the complement-positive MSCs by upregulating DNA hypermethylation of the IL-1β promoter[42].
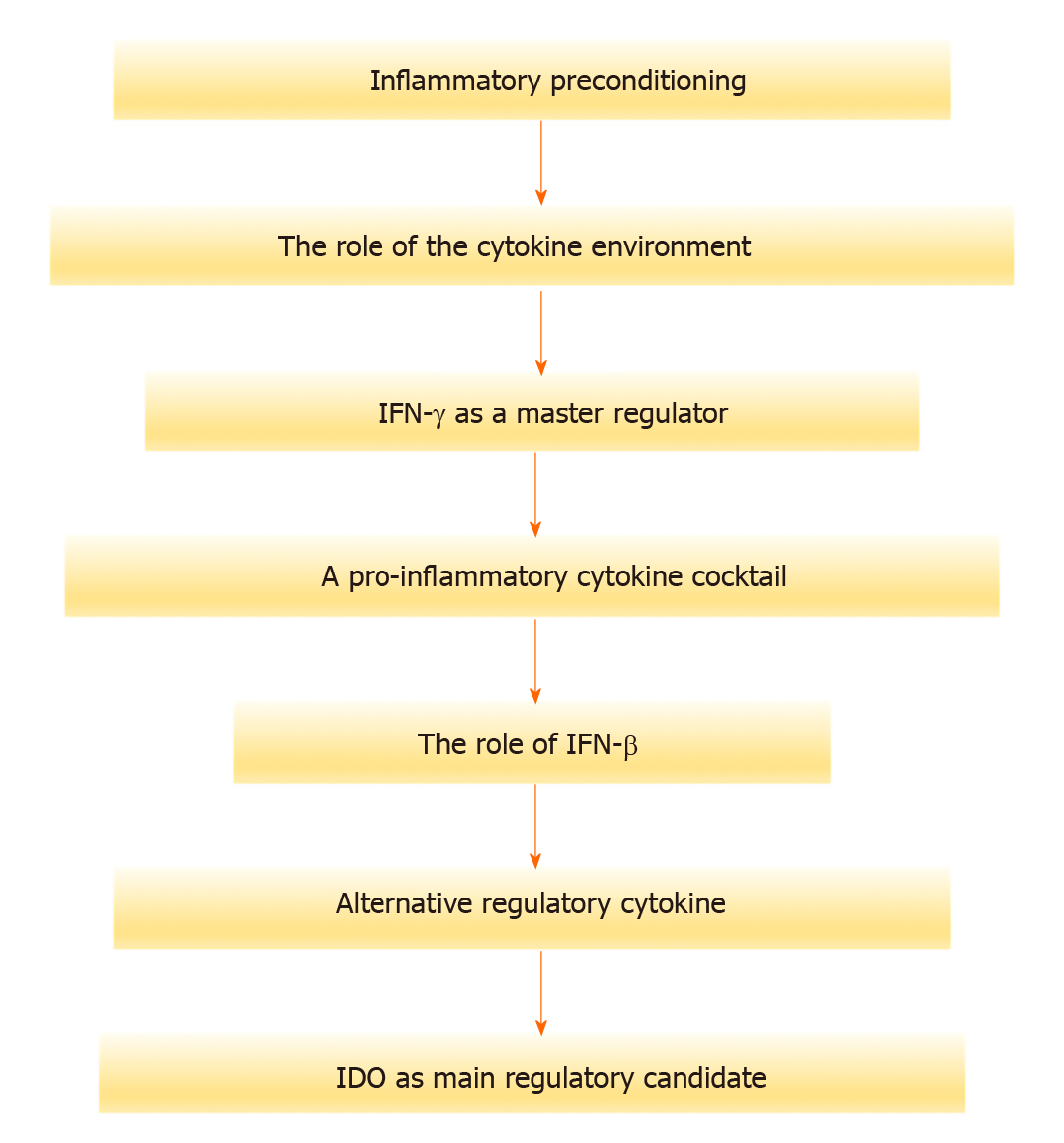
The role of the cytokine environment: Tissue injury is usually associated with inflammation, cell-damage products release and subsequent infiltration of neutrophils and macrophages. The inflammatory response is thought to act as a regulator of tissue stemness either by directly affecting tissue stem cells or by shifting differentiated cells toward a stem-like cell character. During the phagocytosis of damaged cells, pro-inflammatory cytokines mainly interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α), and IL-1 are secreted[43]. Other pro-inflammatory mediators (e.g., various chemokines, leukotrienes, and free radicals) are released by immune cells and may contribute to inflammation. In this context, MSCs are known to preferentially migrate to the sites of inflammation and tissue damage which are typically characterized by cytokine outburst[44]. The specific cytokine milieu is pivotal in determining the fate and behaviors of MSCs (Figure 4).
Accordingly, we reported that inflammation may induce critical changes in the phenotype, multilineage potential, hematopoietic support, and immunomodulatory capacity of MSCs[45].
IFN-γ as a master regulator: One of the most used strategy for this purpose has been the IFN-γ preconditioning of MSCs prior to clinical application. This approach enhances both the immunomodulatory properties and viability of MSCs[46]. In depth proteomic analysis of IFN-γ treated BM-MSCs indicated that approximately 30% of the altered proteins were linked to immunoregulation[47]. The expression levels of selected candidates including indoleamine 2,3-dioxygenase 1 (IDO-1), programmed death ligand 1 (PD-L1), vascular cell adhesion molecule 1, intercellular adhesion molecule 1 (ICAM-1) and bone marrow stromal antigen 2 (BST-2) were markedly increased following IFN-γ treatment. These factors may contribute to the immunoregulatory activities of MSCs. In addition, there are significant immunological and immunoregulatory mediators that are not currently described as IFN-γ responsive [e.g., prostaglandin-endoperoxide synthase 2, prostaglandin I2 synthase, FAM20A (FAM20A golgi-associated secretory pathway pseudokinase), FAM20C (FAM20C golgi-associated secretory pathway kinase) and glycoprotein A repetitions predominant (GARP)/leucine rich repeat containing 32] that were upregulated. Moreover, MSCs isolated from the dental pulp of human exfoliated deciduous teeth and fragments of the orbicularis oris muscle showed enhanced immunomodulatory properties probably linked to increased HLA-G expression[48] in the presence of IFN-γ. Indeed, a recent study highlighted the key role of the HLA-G gene in modulating the immune response, and the importance of its polymorphisms and alleles associated with the outcome of the transplants[49].
A pro-inflammatory cytokine cocktail: INF-γ has also been used in combination with other potent inflammatory cytokines namely TNF-α and IL-1-β. We have shown that preconditioning BM-MSCs with a pro-inflammatory cytokine cocktail increased the expression of cyclooxygenase (COX)-2, leukemia inhibitory factor (LIF), hepatocyte growth factor (HGF), IL-11, IL-8, and IL-6, while it reduced that of COX-1, galectin-1, and transforming growth factor-beta (TGF-β)[50]. BM-MSCs may inhibit complement activation by producing factor H, which could be another mechanism underlying the broad immunosuppressive capabilities of MSCs. Of note, the production of factor H by MSCs is upregulated by inflammatory cytokines TNF-α and IFN-γ in both a dose- and a time-dependent manner[51]. Using such a preconditioning strategy may empower the immune fate of MSCs and, as a result, enhance their value for cell-based immunotherapy. Under IFN-γ and TNF-α preconditioning, BM-MSCs have been shown to synergistically express PD-L1 and PD-L2, which suppress T-cell activation and functions[52]. Interaction of PD-L1 with its known ligands, PD-L1/B7-H1 and PD-L2/B7-DC, provides an inhibitory signal in regulating cellular activation and proliferation. MSCs also secrete significantly higher levels of sPD-L2 compared to sPD-L1 in preconditioning conditions, indicating the potential importance of sPD-L2 in MSC immunomodulation. In line with this, we have shown that the percentage of adipose tissue-derived MSCs expressing PD-L1 (i.e., CD274) significantly increased upon pro-inflammatory stimulation reaching around 90% of the whole cell population[53]. CD274 is known to downregulate T-lymphocyte proliferation and cytokine secretion by binding to the PD-L1 receptor. Interestingly, IFN-γ priming of human amnion-derived MSCs boosted their immunomodulatory potential through different mechanisms. They induced a remodeling of the immune response toward an anti-inflammatory phenotype. In this context, a significant production of chemokines such as C-X-C motif ligand 10 [CXCL10, also known as IFN-γ-induced protein 10 (IP-10) or small-inducible cytokine B10], CXCL9 [also known as monokine induced by gamma interferon (MIG)], C-C motif ligand 3 [CCL3, also known as macrophage inflammatory protein 1-alpha (MIP-1-α)] and CCL4 (i.e., MIP-1-β) was involved in the chemotaxis of innate immune cells. The suppression of the immune response was linked to the expression of PD-L1, IL-10, IDO, and prostaglandin E2 (PGE2), as well as release of different immunomodulatory exosome-derived miRNAs[54]. Within these exosomes, 46 miRNAs were upregulated and 114 were downregulated. Moreover, a miRNA-target network analysis revealed that these miRNAs were associated with immune and inflammatory responses/regulation pathways. Indeed, they were involved in the regulation of both T cell activation/anergy and monocyte differentiation pathways.
In order to increase the efficiency of the preconditioning, encapsulated MSCs with IFN-γ was thus developed. Tethering IFN-γ to the hydrogel increased the retention of IFN-γ within the biomaterial while increasing their immunomodulatory functions[55]. However, such strategy does not work universally as some progenitor cells showing immune-modulatory activities are less responsive to TNF-α and IFN-γ[56]. In comparison to BM-MSCs, human fetal cartilage progenitor cells preconditioned with either TNF-α or IFN-γ did not affect the expression LIF, TNF-stimulated gene-6 (TSG-6), IDO, and HGF known for their immunoregulatory roles. In contrast, adult-derived human liver stem/progenitor cells significantly induced the expression of pro-inflammatory cytokines (IL-1β, IL-6, IL-8, TNFα, CCL5, IL-12a, IL-12b, IL-23p19, IL-27p28, and EBI-3) as well as immunoregulatory cytokines (IL1-RA, IDO-1, and TDO-1) under an inflammatory setting[57]. Within this context, liver derived stem/progenitor cells demonstrate marked immunological plasticity that has main importance for future cell therapy application.
The role of IFN-β: On the other hand, IFN-β was reported to enhance the immunomodulatory functions of MSCs isolated from mouse BM. This increase was linked to the induction of secretory leukocyte protease inhibitor and HGF following a rapid and transient phosphorylation of the transcription factors of signal transducer and activator of transcription (STAT) 1 and 3[58]. In a recent study, a long-lasting induction of mammalian target of rapamycin signaling supported by IFN-β was associated with an increased glycolytic capacity in umbilical cord blood-derived MSCs (UCB-MSCs). These UCB-MSCs also showed an improved ability to control T-cell proliferation[59].
Alternative regulatory cytokine: The preconditioning of BM-MSCs with macrophage-derived soluble factors, either TNF-α or IL-10, enhanced their immunomodulatory potential through increased PGE2 secretion[60]. Cell-to-cell contact with pro-inflammatory macrophages increased TSG-6 production by MSCs, thereby enhancing the suppressive regulation of T cells and switching macrophages to M2. Both cells are associated with wound healing and tissue repair by reducing immune inflammation and infiltration.
Moreover, the expression of CD200 was increased on MSCs thus facilitating the reprogramming of macrophages towards an anti-inflammatory skew through the interaction of CD200 with CD200 receptor on pro-inflammatory macrophages[61]. CD200 is differentially expressed and modulated on MSCs depending on their tissue of origin and culture conditions. A high constitutive expression of CD200 by Wharton's jelly (WJ)-MSCs may represent a distinctive marker of MSCs[62]. In parallel, GARP is proposed as a novel biomarker and new target to improve the therapeutic efficiency of MSCs. Results showed that GARP is constitutively expressed on mouse BM-MSCs and is required to activate locally produced latent TGF-β1, thus inhibiting the proliferation of T-cells and inflammatory cytokine production[63]. However, the presence or absence of GARP on adipose-derived MSCs (ASCs) was noted to display distinct TGF-β responses with diametrically opposing effects on ASC proliferation and survival[64]. Inflammation induces the balance towards a more pronounced tissue regenerative and anti-inflammatory phenotype. Indeed, IFN-γ preconditioning of ASCs enhanced their anti-inflammatory potency. Within the secretome, sixty miRNAs accounted for > 95% of the genetic message that resulted to be chondroprotective and M2 macrophage polarizing[65].
IDO as the main regulatory candidate: IDO is seemingly the most convincing candidate for a crucial role in T-cell inhibition by MSCs. The induction of IDO, which converts tryptophan to kynurenine, is substantially dependent on the preconditioning of MSCs with IFN-γ. Decreased concentration of tryptophan and increased kynurenine, both interfere with effective immune response[66]. It was demonstrated that IDO-mediated tryptophan starvation triggered by MSCs inhibited T-cell activation and proliferation through induction of cellular stress[67]. Both BM-MSCs and dental pulp MSCs were shown to inhibit T-cell activation and proliferation through IDO-mediated tryptophan starvation[67]. Also, preconditioned-adipose tissue-derived MSCs by INF-γ presented a higher immunosuppressive potential probably due to an elevated expression of IDO and ICAM-1[68]. An important immunoregulatory link between IDO and TSG-6 expression was observed in human umbilical cord-derived MSCs. Kynurenic, a metabolite of IDO, controls the TSG-6-mediated anti-inflammatory therapeutic effects of MSCs[69]. In agreement with these observations, we recently demonstrated that pro-inflammatory cytokines-stimulated skin-derived precursors (SKP) were able to suppress the graft-vs-host response when co-transplanted with human peripheral blood mononuclear cells in severe-combined immune deficient mice[70]. Significant changes in the expression and secretion profile of chemo/cytokines and growth factors involved in the immunomodulatory effects of SKP were also reported. Of importance, IFN-γ-preconditioned MSCs were shown to take up and process antigens as well as upregulate HLA class II expression, thus granting the conditions necessary to transform BM-MSCs into unconventional antigen-presenting cells. These MSCs maintained their ability to inhibit lymphocyte proliferation in an antigen-specific manner, without overtly increasing the immunogenicity of allogeneic MSCs[71]. These encouraging findings pave the way to use activated HLA-haplotype matched allogeneic MSCs as a cellular immune intervention therapy by combining their immunomodulatory properties with their antigen-presenting features.
Toll-like receptors as active sentinels: Infection of the wound triggers the body's immune response, causing inflammation and tissue damage, as well as slowing the healing process. In parallel to innate cells, there are other cells spread within the tissue that may be involved in pathogen detection. These may express sensors and transducers that can actively monitor invasion by viruses and bacteria[72]. The presence of microorganisms could be detected by germline-encoded pattern recognition receptors (PRRs) such as toll-like receptors (TLRs). These receptors are responsible for the sensing of structures conserved among microbial species called pathogen-associated molecular patterns. After this recognition, these PRRs may activate different signaling pathways resulting in the secretion of different cytokines and chemokines involved in the immune response against the present infection[73]. PRR ligation may also trigger the activation of phagocytic cells and the phagocytosis of damaged cells. TLRs represent one of the bridges that regulate the crosstalk between the innate and adaptive immune systems. TLRs interact with molecules shared and preserved by the pathogens of origin but also with endogenous molecules (damage/danger-associated molecular patterns) that derive from injured tissues[74]. By being in the surrounding area, MSCs will act as sensors of various signals and accordingly regulate the tissue repair process[75]. We have extensively described how infections such as obtained following TLR-agonist engagement may modulate MSCs at different levels. The phenotype, multilineage potential, hematopoietic support and immunomodulatory capacity of MSCs may thus present relevant changes, which could further affect their therapeutic potential[76]. Moreover, several environmental conditions modulate the pattern and function of TLRs expressed by MSCs (Figure 5).
Specific effects of TLRs: TLR activation may affect MSCs immunomodulatory functions by modulating their cytokine profile. Indeed, a decrease in the immunosuppressive capabilities of BM-MSCs is observed following TLR3 and TLR4 activation by poly(I:C) and lipopolysaccharides (LPS), respectively. Moreover, TLR3 activation augmented IL-6, IL-12p35, IL-23p19, and IL-27p28 transcription, whereas TLR4 activation increased IL-23p19 and IL-27p28 transcription[77]. In a comparative study, TLR3 [poly(I:C)] and TLR4 (LPS) ligation have differentially affected the suppressive functions of BM-, WJ- and adipose tissue (AT)-MSCs[54]. Remarkably, the immunosuppressive potential of WJ- and AT-MSC was not affected while BM-MSC showed reduced ability to inhibit lymphocyte activation. Differences in the levels of HGF and PGE2 secreted by MSCs following TLR activation have been hypothesized to underline these changes[78]. Similarly, the expression profile and function of TLR3 and TLR4 in human olfactory ecto (OE)- and AT-MSCs were reported to be different[79]. Both cell types differentially responded to their agonist engagement by presenting distinct cytokine and chemokine profiles. OE-MSCs exhibited significantly higher levels of chemokine CCL5, IL-8, and TGF-β production, in comparison with AT-MSCs. IL-6 secretion by AT-MSCs was considerably more elevated than that by OE-MSCs. These changes may explain why OE-MSCs exhibited a high proliferative potential and AT-MSCs a more immunomodulatory function. In parallel, injection of LPS-preconditioned MSCs into wounds resulted in a significant acceleration of wound closure. Sensing an infected microenvironment and subsequently activating several innate immune cells by adipose MSCs is linked to TLR4 expression which are triggered by LPS[80]. Preconditioned MSCs with LPS not only trigger innate immune cells by recruiting and activating neutrophils and macrophages, but also initiate a cascade of cellular events which contribute to accelerated repair of skin injury. A network of genes mediating the adaptive immune response including chemokine CXCL6 [also known as granulocyte chemotactic protein 2 (GCP-2)], IL-8, and IL-1β was upregulated through the TLR4 pathway and may be responsible for the acceleration of wound healing. Of note, MSCs isolated from the mouse's abdominal adipose tissues presented a secretome with a dipeptidyl peptidase-IV (DPP-IV)/CD26 and aminopeptidase N/CD13 activity that was decreased following stimulation of MSCs by TLR4 agonist. The DPP-IV/CD26 are ubiquitous ectoenzymes, which can digest various substrates including some chemokines and neuropeptides that are involved in inflammatory conditions[81].
Paradoxically, another study showed that TLR3 is predominantly upregulated in UCB-MSC and its activation leads to their senescence. Additionally, Janus kinase 1 (JAK1) was identified as a key regulatory factor linked to the cellular senescence triggered by TLR3 activation in MSCs. JAK1 activation mediates the IFN-β increased-TLR3 expression, thereby reinforcing TLR3-mediated MSC senescence[59]. In a separate study, TLR ligation was reported to differentially affect the in vitro osteogenic potential of MSCs depending on their tissue origin. Indeed, TLR3 [Poly(I:C)] or TLR4 (LPS) triggering increased the osteogenesis in AT-MSCs and, to a lesser extent, in BM-MSCs. However, WJ-MSCs constitutively disclosed a lower osteogenic potential as compared with other MSCs, which is not affected by TLR[82]. Further findings support that triggering TLR2 may enhance the proliferation and immunomodulatory functions of BM-MSCs. More specifically, the increased immunomodulatory capacity of MSCs was associated with an increased expression of anti-inflammatory cytokine expression and diminution of pro-inflammatory cytokine expression[83]. MSCs can potently regulate the functions of immune cells by attracting them or by migration to inflammatory sites. TLR3-stimulated MSCs exhibit increased migration and chemotaxis within and toward damaged tissues through the expression of forkhead box protein O1-activated genes[84]. The understanding of TLR involvement in the response of stem/progenitor cell to specific tissue damage and in the reparative processes is decisive for the development of new therapeutic strategies[75].
In line with this, we reported approaches using empowered MSCs for the treatment or prevention of different immunological diseases. Preconditioning by new licensing stimuli will empower the immune fate of MSCs and, therefore, promote a better and more efficient biological response[50]. We reported several new pathways induced by inflammatory signals such as fibrinogen-like 2, GAL, semaphorin (SEMA) 4D, SEMA7A, and IDO-1 and can contribute to immunomodulation. These pathways allow distinct MSC populations to display enhanced immunomodulatory effects, particularly during inflammation[85]. Our data also demonstrated that MSCs depending on their tissue-source, may present several relevant receptors potentially involved in the regulation of inflammatory and immunological responses. The expression of advanced glycation end-product receptors, C-type lectin receptors (including DECTIN-1, DECTIN-2 and MINCLE), leukotriene B4 receptors (BLT1 and BLT2) and cysteinyl leukotrienes receptors (CYSLTR1 and CYSLTR2) was substantially influenced by inflammatory conditions[86]. These data strongly support that inflammatory signals are important for the immunological plasticity of MSCs allowing them to display specific responses.
It is important to increase our knowledge about these preconditioning methods and better understand the molecular and cellular mechanisms underlying their effects. It is noteworthy that inadequate manipulation of MSC plasticity may lead to aberrant immune hemostasis and tissue regeneration[87]. The development of the most suitable strategy should not only aim at enhancing the therapeutic value of MSCs but also confirm the absence of any potential adverse effect.
The therapeutic potential of MSCs for tissue repair and wound healing is essentially based on their paracrine effects[88]. The secretome is defined as series of factors including chemokines, cytokines, extracellular matrix molecules and growth factors that are secreted into extracellular space. Once collected, the secretome is considered as “сell-free therapeutics” because it is derived from MSCs and devoid of cells[89]. Moreover, some advantages such as the easy storage/thaw process with a preserved quality and function of the factors are associated with the use of the secretome[90]. The deep analysis of the secretome composition will enable us to evaluate its utility as a new therapeutic option[91]. Thus, advances in the characterization of the secretome composition pointed out the presence of EVs with functional activities.
EVs are small lipid membrane-enclosed particles released by cells into the extracellular space. EVs are very heterogeneous in size and content and can be released naturally or after specific induction. They contain a variety of bioactive components which promote cell-to-cell communication both in a healthy and diseased state[92]. EVs facilitate intracellular communication by carrying and delivering biological materials, such as proteins, lipids, and nucleic acids[93]. Depending on their cellular origin, EVs cover different structures such as exosomes, microvesicles (MVs), and apoptotic bodies[94]. Exosomes are the smallest secreted vesicles (40-140 nm) which are formed by the invagination of the membrane of the multivesicular bodies and fusion with the plasma membrane, to be finally released into the extracellular environment. MVs (50-1000 nm) are budded directly off the plasma membrane and apoptotic bodies (1-5 µm) released from cells undergoing apoptosis[95]. More specifically, MSCs may secrete at least three types of EVs based on their affinities for membrane lipid-binding ligands. As their cargo load are different for each EV type, they are likely to have a different biogenesis pathway and possibly different functions[96]. Several scientific societies (such as SOCRATES, International Society For Extracellular Vesicles, ISCT and International Society of Blood Transfusion) propose to optimize the methods and harmonize the criteria that identify and characterize MSC-derived EVs[97]. These preparations should be defined physically, biochemically, and functionally by quantifiable features and using reproducible and standardized assays[97].
Donor-to-donor variability and heterogeneity of MSC therapeutics are significant factors that interfere with their sustainable translation to the clinic. The use of EVs has multiple advantages in overcoming the limitations and adverse events observed with cell-based therapy[98]. Moreover, the use of MSCs may raise some concerns regarding the purity, viability, identity, recovery after cryopreservation, functional and genomic stability of the cellular product. The choice of the cell source, phenotype, infusion-related toxicities and immunological complication (donor graft-vs-host disease and recipient graft rejection), ectopic tissue formation represent risks associated with the use of MSCs[99]. Thus, MSC-derived EVs can be evaluated as cell-free based therapeutics. EVs have been shown to effectively mimic the therapeutic effects of MSCs, in several preclinical models[100]. Indeed, MSC-derived EVs exert both immunomodulatory as well as pro-regenerative effects[101]. Several observations indicate that EVs may suppress pro-inflammatory processes and reduce oxidative stress. By switching the pro-inflammatory response into a tolerogenic one, MSC-derived EVs are likely to promote tissue regeneration by creating a pro-regenerative environment allowing endogenous stem and progenitor cells to successfully repair affected tissues[102]. Accumulating evidence indicates that MSC-derived EVs exhibit immunomodulatory effects by delivering biologically active nucleic acid and proteins. There is a strong correlation between the expression levels of TGF-β1, pentraxin-related protein-3 (also known as TNF-inducible gene 14 protein), let-7b-5p, or miR-21-5p in MSC-derived EVs and their suppressive function[103]. Moreover, a recent study demonstrated that BM-MSC-derived EVs were incorporated by lymphocytes and decreased their proliferation and differentiation. Interestingly, MSC-derived EVs, by increasing forkhead box P3 expression and reducing the production of IFN-γ, generated a subpopulation of regulatory T cells with suppressive properties. Mechanistically, MSC-derived EVs decreased miR-23a-3p expression and increased expression of its target gene, transforming growth factor beta receptor 2, suggesting active participation of TGF-β pathway in this regulation[104]. Furthermore, early indications suggest that the favorable effects of MSC-derived EVs could be further enhanced by modifying the way in which the donor MSCs are cultured[105]. In general, the preconditioning of MSCs by an inflammatory milieu is the most used method to increase the immunotherapeutic function of MSC-derived EVs[106]. Exosomes derived from BM-MSCs preconditioned with a low dose of dimethyloxaloylglycine (DMOG) were reported to exert enhanced proangiogenic activity during bone regeneration[107]. Several classical pathways related to proliferation and osteogenic and angiogenic differentiations, including yes-associated protein of the Hippo pathway, JAK of the JAK/STAT pathway, p65 of the NF-κB pathway, and β-catenin of the wnt pathway were significantly elevated. In contrast, PTEN and key factors that regulate apoptosis such as p53 and p21 were significantly downregulated[107]. To mimic hypoxic conditions, DMOG degrades peroxisomes by selectively activating pexophagy in a HIF-2α dependent manner involving autophagy receptor p62[108]. In addition, thrombin preconditioning of human UCB-MSCs significantly accelerated EV biogenesis and enriched their cargo contents largely via protease-activated receptor-1-mediated pathways[109]. Recently, MSCs from rat BM were preconditioned with melatonin resulting in an improved therapeutic potential for acute liver ischemic injury[110].
Depending on both MSC origin and environment, EVs may display stimulatory or suppressive immune functions. It is likely that the composition of EVs is a critical determinant of their functions. As previously reported, both the immunomodulatory capabilities of distinct vesicle preparations and the responsiveness of individual patients towards MSC-derived EVs are critical factors for a successful therapeutic application of MSC-derived EVs preparations[111]. Previous studies reported that EVs derived from hypoxic-primed MSCs are packaged with numerous metabolites that are directly associated with immunomodulation, including M2 macrophage polarization and regulatory T lymphocyte induction[112]. The expression of some cytokines, chemokines, and chemokine receptors such as IL-10, HGF, LIF, CCL2, VEGF-C, CCL20, chemokine CXCL2, CXCL8, CXCL16, defensin alpha 1, human hect domain and RLD 5, and interferon induced transmembrane protein 2 were reported to underline the interplay between EVs and their cellular targets[112]. These mediators may participate in migration to the site of injury, regulation of inflammation/immune response and modulation of the repair and regeneration process[113,114]. As we discussed, both pro- and anti-inflammatory signals are present during tissue healing. A critical requisite of MSC-derived EVs is their capacity to support the diametrically opposite pro- and anti-inflammatory functions at the appropriate time. Recently, preconditioned MSC-derived EVs were described as a novel cell-free strategy for expanding hematopoietic stem cells (HSCs) in vitro[115]. Therefore, MSC-derived EVs contribute to the BM homeostasis but may also display multiple roles in the induction and maintenance of abnormal hematopoiesis[116].
Currently, the number of clinical trials involving MSC-derived EVs as listed in www.clinicaltrials.gov is substantially limited. Future experimental designs are still required to deeply understand the therapeutic effects of EVs and their mechanisms of action[100]. Of importance, the current coronavirus disease 2019 (COVID-19) pandemic, which leads to severe and increased worldwide morbidity and mortality, has rapidly promoted MSCs as potential therapeutic agents to suppress COVID-19. In this context, some registered clinical trials using EVs from MSCs are now under investigations. The rationale for these approaches is supported by a growing body of evidence showing that MSC-derived EV preparations are therapeutically safe and efficient in a wide range of diseases[117].
More highlights on optimal production, isolation, storage, therapeutic dose, and schedule of EV administration, will increase the safety and efficiency of the therapy[118]. We also need to consider the state of health of the patient before injection, the immune-biology of MSCs and adequate pre-clinical models[99]. The use of a cell-free preparation based on EVs makes MSCs an important material for the development of new approaches for non-cell-based therapies. Moreover, modulating or preconditioning MSCs to achieve a specific composition of the EV cargo for the ex vivo expansion of HSCs is, therefore, a promising strategy that can overcome several challenges associated with the use of naïve/unprimed MSCs.
The research field of MSCs is innovating but needs more studies to address optimal therapeutic efficiency and safety. MSCs hold great promise in the field of immunotherapy and regenerative medicine. Accordingly, a better understanding of MSC immune biology will improve their therapeutic value and use[4]. The development of a cell-free product derived from MSCs such as EVs is the most promising tool to increase the safety of such therapy. EVs should be well-identified in terms of phenotype, functions, and effects. In parallel, enhancing the survival and functions by evaluating the optimal preconditioning strategy, will improve the therapeutic beneficial actions of MSCs. It is of the utmost importance that this feature, which is closely dependent on disease environment and patient health status, be identified and understood. The development of both features should enhance the value of MSCs by providing a therapeutic product with high quality, safety, and efficiency.
Manuscript source: Invited manuscript
Specialty type: Cell and tissue engineering
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gao BL S-Editor: Yan JP L-Editor: A P-Editor: Ma YJ
| 1. | Giri TK, Alexander A, Agrawal M, Saraf S, Saraf S, Ajazuddin. Current Status of Stem Cell Therapies in Tissue Repair and Regeneration. Curr Stem Cell Res Ther. 2019;14:117-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | De Francesco F. Editorial: Mesenchymal Stem Cells and Interactions With Scaffolds - Biomaterials in Regenerative Medicine: From Research to Translational Applications. Front Cell Dev Biol. 2019;7:193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Lim JE, Son Y. Endogenous Stem Cells in Homeostasis and Aging. Tissue Eng Regen Med. 2017;14:679-698. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Najar M, Bouhtit F, Melki R, Afif H, Hamal A, Fahmi H, Merimi M, Lagneaux L. Mesenchymal Stromal Cell-Based Therapy: New Perspectives and Challenges. J Clin Med. 2019;8:626. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 5. | Loebel C, Burdick JA. Engineering Stem and Stromal Cell Therapies for Musculoskeletal Tissue Repair. Cell Stem Cell. 2018;22:325-339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 6. | Zhou Y, Yamamoto Y, Xiao Z, Ochiya T. The Immunomodulatory Functions of Mesenchymal Stromal/Stem Cells Mediated via Paracrine Activity. J Clin Med. 2019;8:1025. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 128] [Cited by in F6Publishing: 168] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 7. | Li L, Chen X, Wang WE, Zeng C. How to Improve the Survival of Transplanted Mesenchymal Stem Cell in Ischemic Heart? Stem Cells Int. 2016;2016:9682757. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 143] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 8. | Qi K, Li N, Zhang Z, Melino G. Tissue regeneration: The crosstalk between mesenchymal stem cells and immune response. Cell Immunol. 2018;326:86-93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 9. | Michael S, Achilleos C, Panayiotou T, Strati K. Inflammation Shapes Stem Cells and Stemness during Infection and Beyond. Front Cell Dev Biol. 2016;4:118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Guerrouahen BS, Sidahmed H, Al Sulaiti A, Al Khulaifi M, Cugno C. Enhancing Mesenchymal Stromal Cell Immunomodulation for Treating Conditions Influenced by the Immune System. Stem Cells Int. 2019;2019:7219297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Shi Y, Cao J, Wang Y. Rethinking regeneration: empowerment of stem cells by inflammation. Cell Death Differ. 2015;22:1891-1892. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Sobacchi C, Palagano E, Villa A, Menale C. Soluble Factors on Stage to Direct Mesenchymal Stem Cells Fate. Front Bioeng Biotechnol. 2017;5:32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | García-Sánchez D, Fernández D, Rodríguez-Rey JC, Pérez-Campo FM. Enhancing survival, engraftment, and osteogenic potential of mesenchymal stem cells. World J Stem Cells. 2019;11:748-763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 14. | Durand N, Russell A, Zubair AC. Effect of Comedications and Endotoxins on Mesenchymal Stem Cell Secretomes, Migratory and Immunomodulatory Capacity. J Clin Med. 2019;8:497. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Chen Z, Chen L, Zeng C, Wang WE. Functionally Improved Mesenchymal Stem Cells to Better Treat Myocardial Infarction. Stem Cells Int. 2018;2018:7045245. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 16. | Saparov A, Ogay V, Nurgozhin T, Jumabay M, Chen WC. Preconditioning of Human Mesenchymal Stem Cells to Enhance Their Regulation of the Immune Response. Stem Cells Int. 2016;2016:3924858. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 90] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | Hu C, Li L. Preconditioning influences mesenchymal stem cell properties in vitro and in vivo. J Cell Mol Med. 2018;22:1428-1442. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 268] [Cited by in F6Publishing: 235] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 18. | Zhao L, Hu C, Han F, Cai F, Wang J, Chen J. Preconditioning is an effective strategy for improving the efficiency of mesenchymal stem cells in kidney transplantation. Stem Cell Res Ther. 2020;11:197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Ocansey DKW, Pei B, Yan Y, Qian H, Zhang X, Xu W, Mao F. Improved therapeutics of modified mesenchymal stem cells: an update. J Transl Med. 2020;18:42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 88] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 20. | Lee S, Choi E, Cha MJ, Hwang KC. Cell adhesion and long-term survival of transplanted mesenchymal stem cells: a prerequisite for cell therapy. Oxid Med Cell Longev. 2015;2015:632902. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 168] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 21. | Ezquer FE, Ezquer ME, Vicencio JM, Calligaris SD. Two complementary strategies to improve cell engraftment in mesenchymal stem cell-based therapy: Increasing transplanted cell resistance and increasing tissue receptivity. Cell Adh Migr. 2017;11:110-119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 22. | Noronha NC, Mizukami A, Caliári-Oliveira C, Cominal JG, Rocha JLM, Covas DT, Swiech K, Malmegrim KCR. Priming approaches to improve the efficacy of mesenchymal stromal cell-based therapies. Stem Cell Res Ther. 2019;10:131. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 211] [Cited by in F6Publishing: 294] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 23. | Rosová I, Dao M, Capoccia B, Link D, Nolta JA. Hypoxic preconditioning results in increased motility and improved therapeutic potential of human mesenchymal stem cells. Stem Cells. 2008;26:2173-2182. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 514] [Cited by in F6Publishing: 513] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 24. | Zhao L, Hu C, Zhang P, Jiang H, Chen J. Preconditioning strategies for improving the survival rate and paracrine ability of mesenchymal stem cells in acute kidney injury. J Cell Mol Med. 2019;23:720-730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Hwang OK, Noh YW, Hong JT, Lee JW. Hypoxia Pretreatment Promotes Chondrocyte Differentiation of Human Adipose-Derived Stem Cells via Vascular Endothelial Growth Factor. Tissue Eng Regen Med. 2020;17:335-350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 26. | Huang Y, Tan F, Zhuo Y, Liu J, He J, Duan D, Lu M, Hu Z. Hypoxia-preconditioned olfactory mucosa mesenchymal stem cells abolish cerebral ischemia/reperfusion-induced pyroptosis and apoptotic death of microglial cells by activating HIF-1α. Aging. 12:10931-10950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 27. | Martinez VG, Ontoria-Oviedo I, Ricardo CP, Harding SE, Sacedon R, Varas A, Zapata A, Sepulveda P, Vicente A. Overexpression of hypoxia-inducible factor 1 alpha improves immunomodulation by dental mesenchymal stem cells. Stem Cell Res Ther. 2017;8:208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 28. | Najar M, Raicevic G, Fayyad-Kazan H, De Bruyn C, Bron D, Toungouz M, Lagneaux L. Bone Marrow Mesenchymal Stromal Cells Induce Proliferative, Cytokinic and Molecular Changes During the T Cell Response: The Importance of the IL-10/CD210 Axis. Stem Cell Rev Rep. 2015;11:442-452. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 29. | Zhao L, Hu C, Zhang P, Jiang H, Chen J. Melatonin preconditioning is an effective strategy for mesenchymal stem cell-based therapy for kidney disease. J Cell Mol Med. 2020;24:25-33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 30. | Yin L, Huang D, Liu X, Wang Y, Liu J, Liu F, Yu B. Omentin-1 effects on mesenchymal stem cells: proliferation, apoptosis, and angiogenesis in vitro. Stem Cell Res Ther. 2017;8:224. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 31. | Mehrbani Azar Y, Niesler CU, van de Vyver M. Ex vivo antioxidant preconditioning improves the survival rate of bone marrow stem cells in the presence of wound fluid. Wound Repair Regen. 2020;28:506-516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Di Giovanni E, Buonvino S, Amelio I, Melino S. Glutathione-Allylsulfur Conjugates as Mesenchymal Stem Cells Stimulating Agents for Potential Applications in Tissue Repair. Int J Mol Sci. 2020;21:1638. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Basmaeil Y, Rashid MA, Khatlani T, AlShabibi M, Bahattab E, Abdullah ML, Abomaray F, Kalionis B, Massoudi S, Abumaree M. Preconditioning of Human Decidua Basalis Mesenchymal Stem/Stromal Cells with Glucose Increased Their Engraftment and Anti-diabetic Properties. Tissue Eng Regen Med. 2020;17:209-222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Dos Santos GG, Hastreiter AA, Sartori T, Borelli P, Fock RA. L-Glutamine in vitro Modulates some Immunomodulatory Properties of Bone Marrow Mesenchymal Stem Cells. Stem Cell Rev Rep. 2017;13:482-490. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Chen Y, Shu Z, Qian K, Wang J, Zhu H. Harnessing the Properties of Biomaterial to Enhance the Immunomodulation of Mesenchymal Stem Cells. Tissue Eng Part B Rev. 2019;25:492-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 36. | Philippart P, Meuleman N, Stamatopoulos B, Najar M, Pieters K, De Bruyn C, Bron D, Lagneaux L. In vivo production of mesenchymal stromal cells after injection of autologous platelet-rich plasma activated by recombinant human soluble tissue factor in the bone marrow of healthy volunteers. Tissue Eng Part A. 2014;20:160-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 37. | Li Y, Lin F. Mesenchymal stem cells are injured by complement after their contact with serum. Blood. 2012;120:3436-3443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 115] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 38. | Moll G, Jitschin R, von Bahr L, Rasmusson-Duprez I, Sundberg B, Lönnies L, Elgue G, Nilsson-Ekdahl K, Mougiakakos D, Lambris JD, Ringdén O, Le Blanc K, Nilsson B. Mesenchymal stromal cells engage complement and complement receptor bearing innate effector cells to modulate immune responses. PLoS One. 2011;6:e21703. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 39. | Schraufstatter IU, Discipio RG, Zhao M, Khaldoyanidi SK. C3a and C5a are chemotactic factors for human mesenchymal stem cells, which cause prolonged ERK1/2 phosphorylation. J Immunol. 2009;182:3827-3836. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in F6Publishing: 149] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 40. | Gavin C, Meinke S, Heldring N, Heck KA, Achour A, Iacobaeus E, Höglund P, Le Blanc K, Kadri N. The Complement System Is Essential for the Phagocytosis of Mesenchymal Stromal Cells by Monocytes. Front Immunol. 2019;10:2249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 41. | Li Y, Fung J, Lin F. Local Inhibition of Complement Improves Mesenchymal Stem Cell Viability and Function After Administration. Mol Ther. 2016;24:1665-1674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 42. | Zhu X, Wang Y, Jiang Q, Jiang H, Lu J, Wang Y, Kong Y, Chang Y, Xu L, Peng J, Hou M, Huang X, Zhang X. All-trans retinoic acid protects mesenchymal stem cells from immune thrombocytopenia by regulating the complement-interleukin-1β loop. Haematologica. 2019;104:1661-1675. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 43. | Abdulkhaleq LA, Assi MA, Abdullah R, Zamri-Saad M, Taufiq-Yap YH, Hezmee MNM. The crucial roles of inflammatory mediators in inflammation: A review. Vet World. 2018;11:627-635. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 370] [Cited by in F6Publishing: 292] [Article Influence: 48.7] [Reference Citation Analysis (0)] |
| 44. | Zachar L, Bačenková D, Rosocha J. Activation, homing, and role of the mesenchymal stem cells in the inflammatory environment. J Inflamm Res. 2016;9:231-240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 121] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 45. | Najar M, Krayem M, Merimi M, Burny A, Meuleman N, Bron D, Raicevic G, Lagneaux L. Insights into inflammatory priming of mesenchymal stromal cells: functional biological impacts. Inflamm Res. 2018;67:467-477. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 46. | Carvalho AÉS, Sousa MRR, Alencar-Silva T, Carvalho JL, Saldanha-Araujo F. Mesenchymal stem cells immunomodulation: The road to IFN-γ licensing and the path ahead. Cytokine Growth Factor Rev. 2019;47:32-42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 47. | Guan Q, Ezzati P, Spicer V, Krokhin O, Wall D, Wilkins JA. Interferon γ induced compositional changes in human bone marrow derived mesenchymal stem/stromal cells. Clin Proteomics. 2017;14:26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 48. | Junior AL, Pinheiro CCG, Tanikawa DYS, Ferreira JRM, Amano MT, Bueno DF. Mesenchymal Stem Cells from Human Exfoliated Deciduous Teeth and the Orbicularis Oris Muscle: How Do They Behave When Exposed to a Proinflammatory Stimulus? Stem Cells Int. 2020;2020:3670412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 49. | Zoehler B, Fracaro L, Senegaglia AC, Bicalho MDG. Infusion of Mesenchymal Stem Cells to Treat Graft Versus Host Disease: the Role of HLA-G and the Impact of its Polymorphisms. Stem Cell Rev Rep. 2020;16:459-471. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 50. | Najar M, Ouhaddi Y, Bouhtit F, Melki R, Afif H, Boukhatem N, Merimi M, Fahmi H. Empowering the immune fate of bone marrow mesenchymal stromal cells: gene and protein changes. Inflamm Res. 2019;68:167-176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 51. | Tu Z, Li Q, Bu H, Lin F. Mesenchymal stem cells inhibit complement activation by secreting factor H. Stem Cells Dev. 2010;19:1803-1809. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 52. | Davies LC, Heldring N, Kadri N, Le Blanc K. Mesenchymal Stromal Cell Secretion of Programmed Death-1 Ligands Regulates T Cell Mediated Immunosuppression. Stem Cells. 2017;35:766-776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 180] [Cited by in F6Publishing: 230] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 53. | Buyl K, Merimi M, Rodrigues RM, Moussa Agha D, Melki R, Vanhaecke T, Bron D, Lewalle P, Meuleman N, Fahmi H, Rogiers V, Lagneaux L, De Kock J, Najar M. The Impact of Cell-Expansion and Inflammation on The Immune-Biology of Human Adipose Tissue-Derived Mesenchymal Stromal Cells. J Clin Med. 2020;9:696. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 54. | Bulati M, Miceli V, Gallo A, Amico G, Carcione C, Pampalone M, Conaldi PG. The Immunomodulatory Properties of the Human Amnion-Derived Mesenchymal Stromal/Stem Cells Are Induced by INF-γ Produced by Activated Lymphomonocytes and Are Mediated by Cell-To-Cell Contact and Soluble Factors. Front Immunol. 2020;11:54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 55. | García JR, Quirós M, Han WM, O'Leary MN, Cox GN, Nusrat A, García AJ. IFN-γ-tethered hydrogels enhance mesenchymal stem cell-based immunomodulation and promote tissue repair. Biomaterials. 2019;220:119403. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 56. | Lee SJ, Kim J, Choi WH, Park SR, Choi BH, Min BH. Immunophenotype and Immune-Modulatory Activities of Human Fetal Cartilage-Derived Progenitor Cells. Cell Transplant. 2019;28:932-942. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 57. | Najar M, Crompot E, Raicevic G, Sokal EM, Najimi M, Lagneaux L. Cytokinome of adult-derived human liver stem/progenitor cells: immunological and inflammatory features. Hepatobiliary Surg Nutr. 2018;7:331-344. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 58. | Vigo T, La Rocca C, Faicchia D, Procaccini C, Ruggieri M, Salvetti M, Centonze D, Matarese G, Uccelli A; MSRUN Network. IFNβ enhances mesenchymal stromal (Stem) cells immunomodulatory function through STAT1-3 activation and mTOR-associated promotion of glucose metabolism. Cell Death Dis. 2019;10:85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 59. | Lee HJ, Choi B, Kim Y, Lee SE, Jin HJ, Lee HS, Chang EJ, Kim SW. The Upregulation of Toll-Like Receptor 3 via Autocrine IFN-β Signaling Drives the Senescence of Human Umbilical Cord Blood-Derived Mesenchymal Stem Cells Through JAK1. Front Immunol. 2019;10:1659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 60. | Saldaña L, Bensiamar F, Vallés G, Mancebo FJ, García-Rey E, Vilaboa N. Immunoregulatory potential of mesenchymal stem cells following activation by macrophage-derived soluble factors. Stem Cell Res Ther. 2019;10:58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 105] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 61. | Li Y, Zhang D, Xu L, Dong L, Zheng J, Lin Y, Huang J, Zhang Y, Tao Y, Zang X, Li D, Du M. Cell-cell contact with proinflammatory macrophages enhances the immunotherapeutic effect of mesenchymal stem cells in two abortion models. Cell Mol Immunol. 2019;16:908-920. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 62. | Najar M, Raicevic G, Jebbawi F, De Bruyn C, Meuleman N, Bron D, Toungouz M, Lagneaux L. Characterization and functionality of the CD200-CD200R system during mesenchymal stromal cell interactions with T-lymphocytes. Immunol Lett. 2012;146:50-56. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 63. | Niu J, Yue W, Le-Le Z, Bin L, Hu X. Mesenchymal stem cells inhibit T cell activation by releasing TGF-β1 from TGF-β1/GARP complex. Oncotarget. 2017;8:99784-99800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 64. | Carrillo-Gálvez AB, Gálvez-Peisl S, González-Correa JE, de Haro-Carrillo M, Ayllón V, Carmona-Sáez P, Ramos-Mejía V, Galindo-Moreno P, Cara FE, Granados-Principal S, Muñoz P, Martin F, Anderson P. GARP is a key molecule for mesenchymal stromal cell responses to TGF-β and fundamental to control mitochondrial ROS levels. Stem Cells Transl Med. 2020;9:636-650. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 65. | Ragni E, Perucca Orfei C, De Luca P, Mondadori C, Viganò M, Colombini A, de Girolamo L. Inflammatory priming enhances mesenchymal stromal cell secretome potential as a clinical product for regenerative medicine approaches through secreted factors and EV-miRNAs: the example of joint disease. Stem Cell Res Ther. 2020;11:165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 62] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 66. | Wang M, Yuan Q, Xie L. Mesenchymal Stem Cell-Based Immunomodulation: Properties and Clinical Application. Stem Cells Int. 2018;2018:3057624. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 256] [Cited by in F6Publishing: 297] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 67. | Laing AG, Fanelli G, Ramirez-Valdez A, Lechler RI, Lombardi G, Sharpe PT. Mesenchymal stem cells inhibit T-cell function through conserved induction of cellular stress. PLoS One. 2019;14:e0213170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 68. | Serejo TRT, Silva-Carvalho AÉ, Braga LDCF, Neves FAR, Pereira RW, Carvalho JL, Saldanha-Araujo F. Assessment of the Immunosuppressive Potential of INF-γ Licensed Adipose Mesenchymal Stem Cells, Their Secretome and Extracellular Vesicles. Cells. 2019;8:22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 69. | Wang G, Cao K, Liu K, Xue Y, Roberts AI, Li F, Han Y, Rabson AB, Wang Y, Shi Y. Kynurenic acid, an IDO metabolite, controls TSG-6-mediated immunosuppression of human mesenchymal stem cells. Cell Death Differ. 2018;25:1209-1223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 130] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 70. | De Kock J, Rodrigues RM, Branson S, Verhoye L, Colemonts-Vroninks H, Rombaut M, Boeckmans J, Neuckermans J, Lequeue S, Buyl K, Merimi M, Moussa Agha D, De Boe V, Lagneaux L, Meuleman P, Vanhaecke T, Najar M. Inflammation Alters the Secretome and Immunomodulatory Properties of Human Skin-Derived Precursor Cells. Cells. 2020;9:914. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 71. | van Megen KM, van 't Wout ET, Lages Motta J, Dekker B, Nikolic T, Roep BO. Activated Mesenchymal Stromal Cells Process and Present Antigens Regulating Adaptive Immunity. Front Immunol. 2019;10:694. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 72. | Reis e Sousa C. Sensing infection and tissue damage. EMBO Mol Med. 2017;9:285-288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 73. | Kawai T, Akira S. The roles of TLRs, RLRs and NLRs in pathogen recognition. Int Immunol. 2009;21:317-337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1094] [Cited by in F6Publishing: 1117] [Article Influence: 74.5] [Reference Citation Analysis (0)] |
| 74. | Sallustio F, Curci C, Stasi A, De Palma G, Divella C, Gramignoli R, Castellano G, Gallone A, Gesualdo L. Role of Toll-Like Receptors in Actuating Stem/Progenitor Cell Repair Mechanisms: Different Functions in Different Cells. Stem Cells Int. 2019;2019:6795845. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 75. | Bernardo ME, Fibbe WE. Mesenchymal stromal cells: sensors and switchers of inflammation. Cell Stem Cell. 2013;13:392-402. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 903] [Cited by in F6Publishing: 971] [Article Influence: 97.1] [Reference Citation Analysis (0)] |
| 76. | Najar M, Krayem M, Meuleman N, Bron D, Lagneaux L. Mesenchymal Stromal Cells and Toll-Like Receptor Priming: A Critical Review. Immune Netw. 2017;17:89-102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 77. | Raicevic G, Rouas R, Najar M, Stordeur P, Boufker HI, Bron D, Martiat P, Goldman M, Nevessignsky MT, Lagneaux L. Inflammation modifies the pattern and the function of Toll-like receptors expressed by human mesenchymal stromal cells. Hum Immunol. 2010;71:235-244. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 125] [Cited by in F6Publishing: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 78. | Raicevic G, Najar M, Stamatopoulos B, De Bruyn C, Meuleman N, Bron D, Toungouz M, Lagneaux L. The source of human mesenchymal stromal cells influences their TLR profile as well as their functional properties. Cell Immunol. 2011;270:207-216. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 79. | Jafari M, Asghari A, Delbandi AA, Jalessi M, Jazayeri MH, Samarei R, Tajik N. Priming TLR3 and TLR4 in human adipose- and olfactory mucosa-derived mesenchymal stromal cells and comparison of their cytokine secretions. Cytotechnology. 2020;72:57-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 80. | Munir S, Basu A, Maity P, Krug L, Haas P, Jiang D, Strauss G, Wlaschek M, Geiger H, Singh K, Scharffetter-Kochanek K. TLR4-dependent shaping of the wound site by MSCs accelerates wound healing. EMBO Rep. 2020;21:e48777. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 81. | Ramezani Ali Akbari K, Fathollahi A, Hashemi SM, Pouriran R, Yeganeh F. Activity of Dipeptidyl Peptidase-IV/CD26 and Aminopeptidase N/CD13 in Secretome of Mesenchymal Stem Cells after Treatment with LPS and PMA. Iran J Immunol. 2020;17:41-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 82. | Raicevic G, Najar M, Pieters K, De Bruyn C, Meuleman N, Bron D, Toungouz M, Lagneaux L. Inflammation and Toll-like receptor ligation differentially affect the osteogenic potential of human mesenchymal stromal cells depending on their tissue origin. Tissue Eng Part A. 2012;18:1410-1418. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 83. | Silveira GDP, Ishimura ME, Teixeira D, Galindo LT, Sardinha AA, Porcionatto M, Longo-Maugéri IM. Improvement of Mesenchymal Stem Cell Immunomodulatory Properties by Heat-Killed Propionibacterium acnes via TLR2. Front Mol Neurosci. 2018;11:489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 84. | Hwa Kim S, Das A, In Choi H, Hoon Kim K, Choul Chai J, Ran Choi M, Binas B, Sun Park K, Seek Lee Y, Jung KH, Gyu Chai Y. Forkhead box O1 (FOXO1) controls the migratory response of Toll-like receptor (TLR3)-stimulated human mesenchymal stromal cells. J Biol Chem. 2019;294:8424-8437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 85. | Fayyad-Kazan M, Najar M, Fayyad-Kazan H, Raicevic G, Lagneaux L. Identification and Evaluation of New Immunoregulatory Genes in Mesenchymal Stromal Cells of Different Origins: Comparison of Normal and Inflammatory Conditions. Med Sci Monit Basic Res. 2017;23:87-96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 86. | Najar M, Fayyad-Kazan M, Raicevic G, Fayyad-Kazan H, Meuleman N, Bron D, Lagneaux L. Advanced Glycation End-Products-, C-Type Lectin- and Cysteinyl/ Leukotriene-Receptors in Distinct Mesenchymal Stromal Cell Populations: Differential Transcriptional Profiles in Response to Inflammation. Cell J. 2018;20:250-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 87. | Poggi A, Varesano S, Zocchi MR. Corrigendum: How to Hit Mesenchymal Stromal Cells and Make the Tumor Microenvironment Immunostimulant Rather Than Immunosuppressive. Front Immunol. 2018;9:1342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 88. | Gomzikova MO, James V, Rizvanov AA. Therapeutic Application of Mesenchymal Stem Cells Derived Extracellular Vesicles for Immunomodulation. Front Immunol. 2019;10:2663. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 73] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 89. | Linero I, Chaparro O. Paracrine effect of mesenchymal stem cells derived from human adipose tissue in bone regeneration. PLoS One. 2014;9:e107001. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 197] [Cited by in F6Publishing: 217] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 90. | Abbasi-Malati Z, Roushandeh AM, Kuwahara Y, Roudkenar MH. Mesenchymal Stem Cells on Horizon: A New Arsenal of Therapeutic Agents. Stem Cell Rev Rep. 2018;14:484-499. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 91. | L PK, Kandoi S, Misra R, S V, K R, Verma RS. The mesenchymal stem cell secretome: A new paradigm towards cell-free therapeutic mode in regenerative medicine. Cytokine Growth Factor Rev. 2019;46:1-9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 227] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 92. | Carpintero-Fernández P, Fafián-Labora J, O'Loghlen A. Technical Advances to Study Extracellular Vesicles. Front Mol Biosci. 2017;4:79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 93. | Joo HS, Suh JH, Lee HJ, Bang ES, Lee JM. Current Knowledge and Future Perspectives on Mesenchymal Stem Cell-Derived Exosomes as a New Therapeutic Agent. Int J Mol Sci. 2020;21:727. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 87] [Cited by in F6Publishing: 154] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 94. | Seo Y, Kim HS, Hong IS. Stem Cell-Derived Extracellular Vesicles as Immunomodulatory Therapeutics. Stem Cells Int. 2019;2019:5126156. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 97] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 95. | Varderidou-Minasian S, Lorenowicz MJ. Mesenchymal stromal/stem cell-derived extracellular vesicles in tissue repair: challenges and opportunities. Theranostics. 2020;10:5979-5997. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 122] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 96. | Lai RC, Tan SS, Yeo RW, Choo AB, Reiner AT, Su Y, Shen Y, Fu Z, Alexander L, Sze SK, Lim SK. MSC secretes at least 3 EV types each with a unique permutation of membrane lipid, protein and RNA. J Extracell Vesicles. 2016;5:29828. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 166] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 97. | Witwer KW, Van Balkom BWM, Bruno S, Choo A, Dominici M, Gimona M, Hill AF, De Kleijn D, Koh M, Lai RC, Mitsialis SA, Ortiz LA, Rohde E, Asada T, Toh WS, Weiss DJ, Zheng L, Giebel B, Lim SK. Defining mesenchymal stromal cell (MSC)-derived small extracellular vesicles for therapeutic applications. J Extracell Vesicles. 2019;8:1609206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 340] [Cited by in F6Publishing: 351] [Article Influence: 70.2] [Reference Citation Analysis (0)] |
| 98. | Bieback K, Kuçi S, Schäfer R. Production and quality testing of multipotent mesenchymal stromal cell therapeutics for clinical use. Transfusion. 2019;59:2164-2173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 99. | Mendt M, Rezvani K, Shpall E. Mesenchymal stem cell-derived exosomes for clinical use. Bone Marrow Transplant. 2019;54:789-792. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 193] [Cited by in F6Publishing: 274] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 100. | Maacha S, Sidahmed H, Jacob S, Gentilcore G, Calzone R, Grivel JC, Cugno C. Paracrine Mechanisms of Mesenchymal Stromal Cells in Angiogenesis. Stem Cells Int. 2020;2020:4356359. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 122] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 101. | Giebel B, Kordelas L, Börger V. Clinical potential of mesenchymal stem/stromal cell-derived extracellular vesicles. Stem Cell Investig. 2017;4:84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 108] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 102. | Börger V, Bremer M, Ferrer-Tur R, Gockeln L, Stambouli O, Becic A, Giebel B. Mesenchymal Stem/Stromal Cell-Derived Extracellular Vesicles and Their Potential as Novel Immunomodulatory Therapeutic Agents. Int J Mol Sci. 2017;18:1450. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 191] [Cited by in F6Publishing: 256] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 103. | Kim H, Lee MJ, Bae EH, Ryu JS, Kaur G, Kim HJ, Kim JY, Barreda H, Jung SY, Choi JM, Shigemoto-Kuroda T, Oh JY, Lee RH. Comprehensive Molecular Profiles of Functionally Effective MSC-Derived Extracellular Vesicles in Immunomodulation. Mol Ther. 2020;28:1628-1644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 66] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 104. | Franco da Cunha F, Andrade-Oliveira V, Candido de Almeida D, Borges da Silva T, Naffah de Souza Breda C, Costa Cruz M, Faquim-Mauro EL, Antonio Cenedeze M, Ioshie Hiyane M, Pacheco-Silva A, Aparecida Cavinato R, Torrecilhas AC, Olsen Saraiva Câmara N. Extracellular Vesicles isolated from Mesenchymal Stromal Cells Modulate CD4+ T Lymphocytes Toward a Regulatory Profile. Cells. 2020;9:1059. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 105. | Tsiapalis D, O'Driscoll L. Mesenchymal Stem Cell Derived Extracellular Vesicles for Tissue Engineering and Regenerative Medicine Applications. Cells. 2020;9:991. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 177] [Cited by in F6Publishing: 154] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 106. | Martin-Rufino JD, Espinosa-Lara N, Osugui L, Sanchez-Guijo F. Targeting the Immune System With Mesenchymal Stromal Cell-Derived Extracellular Vesicles: What Is the Cargo's Mechanism of Action? Front Bioeng Biotechnol. 2019;7:308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 107. | Liang B, Liang JM, Ding JN, Xu J, Xu JG, Chai YM. Dimethyloxaloylglycine-stimulated human bone marrow mesenchymal stem cell-derived exosomes enhance bone regeneration through angiogenesis by targeting the AKT/mTOR pathway. Stem Cell Res Ther. 2019;10:335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 108. | Mu Y, Maharjan Y, Dutta RK, Kim H, Wei X, Kim JH, Kim D, Park C, Park R. Dimethyloxaloylglycine induces pexophagy in a HIF-2α dependent manner involving autophagy receptor p62. Biochem Biophys Res Commun. 2020;525:46-52. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 109. | Sung DK, Sung SI, Ahn SY, Chang YS, Park WS. Thrombin Preconditioning Boosts Biogenesis of Extracellular Vesicles from Mesenchymal Stem Cells and Enriches Their Cargo Contents via Protease-Activated Receptor-Mediated Signaling Pathways. Int J Mol Sci. 2019;20:2899. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 110. | Alzahrani FA. Melatonin improves therapeutic potential of mesenchymal stem cells-derived exosomes against renal ischemia-reperfusion injury in rats. Am J Transl Res. 2019;11:2887-2907. [PubMed] [Cited in This Article: ] |
| 111. | Kordelas L, Schwich E, Dittrich R, Horn PA, Beelen DW, Börger V, Giebel B, Rebmann V. Individual Immune-Modulatory Capabilities of MSC-Derived Extracellular Vesicle (EV) Preparations and Recipient-Dependent Responsiveness. Int J Mol Sci. 2019;20:1642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 112. | Showalter MR, Wancewicz B, Fiehn O, Archard JA, Clayton S, Wagner J, Deng P, Halmai J, Fink KD, Bauer G, Fury B, Perotti NH, Apperson M, Butters J, Belafsky P, Farwell G, Kuhn M, Nolta JA, Anderson JD. Primed mesenchymal stem cells package exosomes with metabolites associated with immunomodulation. Biochem Biophys Res Commun. 2019;512:729-735. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 113. | Mardpour S, Hamidieh AA, Taleahmad S, Sharifzad F, Taghikhani A, Baharvand H. Interaction between mesenchymal stromal cell-derived extracellular vesicles and immune cells by distinct protein content. J Cell Physiol. 2019;234:8249-8258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 114. | Carreras-Planella L, Monguió-Tortajada M, Borràs FE, Franquesa M. Immunomodulatory Effect of MSC on B Cells Is Independent of Secreted Extracellular Vesicles. Front Immunol. 2019;10:1288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 115. | Budgude P, Kale V, Vaidya A. Mesenchymal stromal cell-derived extracellular vesicles as cell-free biologics for the ex vivo expansion of hematopoietic stem cells. Cell Biol Int. 2020;44:1078-1102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 116. | Batsali AK, Georgopoulou A, Mavroudi I, Matheakakis A, Pontikoglou CG, Papadaki HA. The Role of Bone Marrow Mesenchymal Stem Cell Derived Extracellular Vesicles (MSC-EVs) in Normal and Abnormal Hematopoiesis and Their Therapeutic Potential. J Clin Med. 2020;9:856. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 117. | Börger V, Weiss DJ, Anderson JD, Borràs FE, Bussolati B, Carter DRF, Dominici M, Falcón-Pérez JM, Gimona M, Hill AF, Hoffman AM, de Kleijn D, Levine BL, Lim R, Lötvall J, Mitsialis SA, Monguió-Tortajada M, Muraca M, Nieuwland R, Nowocin A, O'Driscoll L, Ortiz LA, Phinney DG, Reischl I, Rohde E, Sanzenbacher R, Théry C, Toh WS, Witwer KW, Lim SK, Giebel B. International Society for Extracellular Vesicles and International Society for Cell and Gene Therapy statement on extracellular vesicles from mesenchymal stromal cells and other cells: considerations for potential therapeutic agents to suppress coronavirus disease-19. Cytotherapy. 2020;22:482-485. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 86] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 118. | Rohde E, Pachler K, Gimona M. Manufacturing and characterization of extracellular vesicles from umbilical cord-derived mesenchymal stromal cells for clinical testing. Cytotherapy. 2019;21:581-592. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 114] [Article Influence: 22.8] [Reference Citation Analysis (0)] |