Abstract
Purpose
To assess the therapeutic efficacy of external ventricular draining (EVD) and to predict the need for permanent shunts in infants with postinfective hydrocephalus (PIHC).
Methods
This is a retrospective study of infants diagnosed with PIHC and treated by EVD between January 2013 and December 2017 at the Children’s Hospital of Fudan University. Clinical, laboratory, and imaging data were collected and analyzed to identify independent risk factors by logistic regression analyses. The predictor was evaluated using the area under the curve (AUC) of the receiver operating characteristic (ROC) curves.
Results
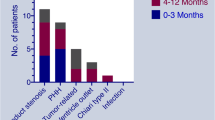
In total, 48 patients were identified, and 31 cases (64.5%) had a permanent shunt. EVD was effective in accelerating cerebrospinal fluid purification. In the permanent shunt group, the duration of EVD was significantly longer (28.5 ± 5.2 vs 14.9 ± 3.0 P < 0.05) and the frontal and occipital horn ratio (FOHR) at 7–10 days after EVD was significantly higher (0.57 ± 0.01 vs 0.48 ± 0.01 P < 0.001). The FOHR at 7–10 days after EVD predicts the need for a permanent shunt with an area under the ROC curve of 0.818.
Conclusion
EVD was effective for purification of CSF, whereas a permanent shunt was needed for more than half of the patients. The FOHR at 7–10 days after EVD may be a strong predictor for a permanent shunt.


Similar content being viewed by others
Data availability
All data were available.
References
Hsu M-H, Hsu J-F, Kuo H-C, Lai MY, Chiang MC, Lin YJ, Huang HR, Chu SM, Tsai MH (2018) Neurological complications in young infants with acute bacterial meningitis. Front Neurol 9:903. https://doi.org/10.3389/fneur.2018.00903
Chu S-M, Hsu J-F, Lee C-W, Lien R, Huang HR, Chiang MC, Fu RH, Tsai MH (2014) Neurological complications after neonatal bacteremia: the clinical characteristics, risk factors, and outcomes. PLoS One 9:e105294. https://doi.org/10.1371/journal.pone.0105294
Peros T, van Schuppen J, Bohte A, Hodiamont C, Aronica E, de Haan T (2020) Neonatal bacterial meningitis versus ventriculitis: a cohort-based overview of clinical characteristics, microbiology and imaging. Eur J Pediatr 179:1969–1977. https://doi.org/10.1007/s00431-020-03723-3
Chatterjee S, Chatterjee U (2011) Overview of post-infective hydrocephalus. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 27:1693–1698. https://doi.org/10.1007/s00381-011-1557-z
Gaderer C, Schaumann A, Schulz M, Thomale UW (2018) Neuroendoscopic lavage for the treatment of CSF infection with hydrocephalus in children. Childs Nerv Syst ChNS Off J Int Soc Pediatr Neurosurg 34:1893–1903. https://doi.org/10.1007/s00381-018-3894-7
George T, Moorthy RK, Rajshekhar V (2019) Long tunnel external ventricular drain: an adjunct in the management of patients with infection associated hydrocephalus. Br J Neurosurg 33:659–663. https://doi.org/10.1080/02688697.2019.1667483
Dorresteijn KRIS, Jellema K, van de Beek D, Brouwer MC (2019) Factors and measures predicting external CSF drain-associated ventriculitis: a review and meta-analysis. Neurology 93:964–972. https://doi.org/10.1212/WNL.0000000000008552
McAllister JP, Williams MA, Walker ML et al (2015) An update on research priorities in hydrocephalus: overview of the third National Institutes of Health-sponsored symposium “Opportunities for Hydrocephalus Research: Pathways to Better Outcomes.”. J Neurosurg 123:1427–1438. https://doi.org/10.3171/2014.12.JNS132352
Simon TD, Kronman MP, Whitlock KB et al (2016) Variability in management of first cerebrospinal fluid shunt infection: a prospective multi-institutional observational cohort study. J Pediatr 179:185–191.e2. https://doi.org/10.1016/j.jpeds.2016.08.094
van de Beek D, Brouwer M, Hasbun R, Koedel U, Whitney CG, Wijdicks E (2016) Community-acquired bacterial meningitis. Nat Rev Dis Primer 2:16074. https://doi.org/10.1038/nrdp.2016.74
van de Beek D, de Gans J, Tunkel AR, Wijdicks EFM (2006) Community-acquired bacterial meningitis in adults. N Engl J Med 354:44–53. https://doi.org/10.1056/NEJMra052116
O’Hayon BB, Drake JM, Ossip MG, Tuli S, Clarke M (1998) Frontal and occipital horn ratio: a linear estimate of ventricular size for multiple imaging modalities in pediatric hydrocephalus. Pediatr Neurosurg 29:245–249. https://doi.org/10.1159/000028730
van de Beek D, Brouwer MC, Thwaites GE, Tunkel AR (2012) Advances in treatment of bacterial meningitis. Lancet Lond Engl 380:1693–1702. https://doi.org/10.1016/S0140-6736(12)61186-6
Patra DP, Bir SC, Maiti TK, Kalakoti P, Cuellar H, Guthikonda B, Sun H, Notarianni C, Nanda A (2016) Role of radiological parameters in predicting overall shunt outcome after ventriculoperitoneal shunt insertion in pediatric patients with obstructive hydrocephalus. Neurosurg Focus 41:E4. https://doi.org/10.3171/2016.8.FOCUS16263
Radhakrishnan R, Brown BP, Kralik SF, Bain D, Persohn S, Territo PR, Jea A, Karmazyn B (2019) Frontal occipital and frontal temporal horn ratios: comparison and validation of head ultrasound-derived indexes with MRI and ventricular volumes in infantile ventriculomegaly. AJR Am J Roentgenol 213:925–931. https://doi.org/10.2214/AJR.19.21261
Oushy S, Parker JJ, Campbell K, Palmer C, Wilkinson C, Stence NV, Handler MH, Mirsky DM (2017) Frontal and occipital horn ratio is associated with multifocal intraparenchymal hemorrhages in neonatal shunted hydrocephalus. J Neurosurg Pediatr 20:432–438. https://doi.org/10.3171/2017.6.PEDS16481
Anania P, Battaglini D, Balestrino A, D’Andrea A, Prior A, Ceraudo M, Rossi DC, Zona G, Fiaschi P (2020) The role of external ventricular drainage for the management of posterior cranial fossa tumours: a systematic review. Neurosurg Rev. https://doi.org/10.1007/s10143-020-01325-z
Sorinola A, Buki A, Sandor J, Czeiter E (2019) Risk factors of external ventricular drain infection: proposing a model for future studies. Front Neurol 10:226. https://doi.org/10.3389/fneur.2019.00226
Lewis A, Kimberly TW (2016) A retrospective analysis of cerebrospinal fluid drainage volume in subarachnoid hemorrhage and the need for early or late ventriculoperitoneal shunt placement. J Neurosurg Sci 60:289–295
Wang JY, Amin AG, Jallo GI, Ahn ES (2014) Ventricular reservoir versus ventriculosubgaleal shunt for posthemorrhagic hydrocephalus in preterm infants: infection risks and ventriculoperitoneal shunt rate. J Neurosurg Pediatr 14:447–454. https://doi.org/10.3171/2014.7.PEDS13552
Pedersen EMJ, Köhler-Forsberg O, Nordentoft M, Christensen RHB, Mortensen PB, Petersen L, Benros ME (2020) Infections of the central nervous system as a risk factor for mental disorders and cognitive impairment: a nationwide register-based study. Brain Behav Immun 88:668–674. https://doi.org/10.1016/j.bbi.2020.04.072
Tan J, Kan J, Qiu G, Zhao D, Ren F, Luo Z, Zhang Y (2015) Clinical prognosis in neonatal bacterial meningitis: the role of cerebrospinal fluid protein. PLoS One 10:e0141620. https://doi.org/10.1371/journal.pone.0141620
Peng H-L, Hu Y, Chen H-J, Song PP, Jiang L (2018) Risk factors for poor prognosis in children with refractory purulent meningitis and the discharge criteria. J Infect Public Health 11:238–242. https://doi.org/10.1016/j.jiph.2017.07.007
Materials availability
All materials were available.
Funding
There is no funding support for this research.
Author information
Authors and Affiliations
Contributions
Yi Zhang:
• Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
• Drafting the article or revising it critically for important intellectual content;
• Final approval of the version to be published.
Rui Zhao:
• Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
• Drafting the article or revising it critically for important intellectual content;
• Final approval of the version to be published.
Wei Shi:
• Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
• Drafting the article or revising it critically for important intellectual content;
JiCui Zheng:
• Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
• Drafting the article or revising it critically for important intellectual content;
Hao Li:
• Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
• Final approval of the version to be published.
ZhiHua Li
• Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data;
• Drafting the article or revising it critically for important intellectual content;
• Final approval of the version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval and consent to participate
This study was a clinical research. This study was approved by the institutional review board of Children’s Hospital of Fudan University. Patient consent was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, Y., Zhao, R., Shi, W. et al. Predictor of a permanent shunt after treatment of external ventricular draining in pediatric postinfective hydrocephalus—a retrospective cohort study. Childs Nerv Syst 37, 1877–1882 (2021). https://doi.org/10.1007/s00381-021-05054-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05054-6