Abstract
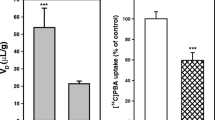
Thiamine deficiency (TD) results in focal lesions in several regions of the rat brain including the thalamus and inferior colliculus. Since alterations in blood-brain barrier (BBB) integrity may play a role in this damage, we have examined the influence of TD on the unidirectional blood-to-brain transfer constant (Ki) of the low molecular weight species α-aminoisobutyric acid (AIB) in vulnerable and non-vulnerable brain regions at different stages during progression of the disorder, and following its reversal with thiamine. Analysis of the regional distribution of Ki values showed early (day 10) increased transfer of [14C]-AIB across the BBB in the vulnerable medial thalamus as well as the non-vulnerable caudate and hippocampus. At the acute symptomatic stage (day 14), more widespread BBB permeability changes were detected in most areas including the lateral thalamus, inferior colliculus, and non-vulnerable cerebellum and pons. Twenty-four hours following thiamine replenishment, a heterogeneous pattern of increased BBB permeability was observed in which many structures maintained increased uptake of [14C]-AIB. No increase in the [3H]-dextran space, a marker of intravascular volume, was detected in brain regions during the progress of TD, suggesting that BBB permeability to this large tracer was unaffected. These results indicate that BBB opening i) occurs early during TD, ii) is not restricted to vulnerable areas of the brain, iii) is progressive, iv) persists for at least 24 h following treatment with thiamine, and v) is likely selective in nature, depending on the molecular species being transported.

Similar content being viewed by others
References
Abbott NJ (2002) Astrocyte-endothelial interactions and blood-brain barrier permeability. J Anat 200:629–638
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ (2010) Structure and function of the blood-brain barrier. Neurobiol Dis 37:13–25
Abdou E, Hazell AS (2015) Thiamine deficiency: an update of pathophysiologic mechanisms and future therapeutic considerations. Neurochem Res 40:353–361
Aikawa H, Watanabe IS, Furuse T, Iwasaki Y, Satoyoshi E, Sumi T, Moroji T (1984) Low energy levels in thiamine-deficient encephalopathy. J Neuropathol Exp Neurol 43:276–287
Au AM, Chan PH, Fishman RA (1985) Stimulation of phospholipase A2 activity by oxygen-derived free radicals in isolated brain capillaries. J Cell Biochem 27:449–453
Ballabh P, Braun A, Nedergaard M (2004) The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis 16:1–13
Beauchesne E, Desjardins P, Hazell AS, Butterworth RF (2009a) Altered expression of tight junction proteins and matrix metalloproteinases in thiamine-deficient mouse brain. Neurochem Int 55:275–281
Beauchesne E, Desjardins P, Hazell AS, Butterworth RF (2009b) eNOS gene deletion restores blood-brain barrier integrity and attenuates neurodegeneration in the thiamine-deficient mouse brain. J Neurochem 111:452–459
Beauchesne E, Desjardins P, Butterworth RF, Hazell AS (2010) Up-regulation of caveolin-1 and blood-brain barrier breakdown are attenuated by N-acetylcysteine in thiamine deficiency. Neurochem Int 57:830–837
Blasberg RG, Fenstermacher JD, Patlak CS (1983) Transport of α-aminoisobutyric acid across brain capillary and cellular membranes. J Cereb Blood Flow Metab 3:8–32
Brightman MW (1977) Morphology of blood-brain interfaces. Exp Eye Res (Suppl) 25:1–25
Butterworth RF (1986) Cerebral thiamine-dependent enzyme changes in experimental Wernicke’s encephalopathy. Metab Brain Dis 1:165–175
Butterworth RF (1993) Pathophysiologic mechanisms responsible for the reversible (thiamine responsive) and irreversible (thiamine non-responsive) neurological signs of Wernicke’s encephalopathy. Drug Alcohol Rev 12:317–324
Calingasan N, Baker H, Sheu K-FR, Gibson GE (1995) Blood-brain abnormalities in vulnerable brain regions during thiamine deficiency. Exp Neurol 134:64–72
Chan PH, Schmidley JW, Fishman RA, Longar SM (1984) Brain injury, edema, and vascular permeability changes induced by oxygen-derived free radicals. Neurology 34:315–320
Chan H, Butterworth RF, Hazell AS (2004) Primary cultures of rat astrocytes respond to thiamine deficiency-induced swelling by downregulating aquaporin-4 levels. Neurosci Lett 366:231–234
Crone C (1963) The permeability of capillaries in various organs as determined by use of the ‘indicator diffusion’ method. Acta Physiol Scand 52:292–305
De Bock M, Van Haver V, Vandenbroucke RE, Decrock E, Wang N, Leybaert L (2016) Into rather unexplored terrain-transcellular transport across the blood-brain barrier. Glia 64:1097–1123
Del Maestro RF, Bjork J, Arfors K-E (1981) Increase in microvascular permeability induced by enzymatically generated free radicals. Microvasc Res 22:255–270
Dobbin J, Crockard A, Ross-Russell R (1989) Transient blood-brain barrier permeability following profound temporary global ischaemia: an experimental study using 14C-AIB. J Cereb Blood Flow Metab 9:71–78
Doll DN, Hu H, Sun J, Lewis SE, Simpkins JW, Ren X (2015) Mitochondrial crisis in cerebrovascular endothelial cells opens the blood-brain barrier. Stroke 46:1681–1689
Ellison MD, Povlishock JT, Hayes RL (1986) Examination of the blood-to-brain transfer of α-aminoisobutyric acid and horseradish peroxidase: regional alterations in blood-brain barrier function following acute hypertension. J Cereb Blood Flow Metab 6:471–480
Gibson GE, Ksiezak-Reding H, Sheu K-FR, Mykytyn V, Blass JP (1984) Correlation of enzymatic, metabolic, and behavioural deficits in thiamin deficiency and its reversal. Neurochem Res 9:803–814
Gregoire N (1989) The blood-brain barrier. J Neuroradiol 16:238–250
Hakim AM (1984) The induction and reversibility of cerebral acidosis in thiamine deficiency. Ann Neurol 16:673–679
Hakim AM (1986) Effect of thiamine deficiency and its reversal on cerebral blood flow in the rat. Observations on the phenomena of hyperperfusion, "no reflow", and delayed hypoperfusion. J Cereb Blood Flow Metab 6:79–85
Hakim AM, Carpenter S, Pappius HM (1983) Metabolic and histological reversibility of thiamine deficiency. J Cereb Blood Flow Metab 3:468–477
Harata N, Iwasaki Y (1995) Evidence for early blood-brain barrier breakdown in experimental thiamine deficiency in the mouse. Metab Brain Dis 10:565–576
Hazell AS (2009) Astrocytes are a major target in thiamine deficiency and Wernicke's encephalopathy. Neurochem Int 55:129–135
Hazell AS, Butterworth RF, Hakim AM (1993) Cerebral vulnerability is associated with selective increase in extracellular glutamate concentration in experimental thiamine deficiency. J Neurochem 61:1155–1158
Hazell AS, Rao KV, Danbolt NC, Pow DV, Butterworth RF (2001) Selective down-regulation of the astrocyte glutamate transporters GLT-1 and GLAST within the medial thalamus in experimental Wernicke's encephalopathy. J Neurochem 78:560–568
Hazell AS, Faim S, Wertheimer G, Silva VR, Marques CS (2013) The impact of oxidative stress in thiamine deficiency: a multifactorial targeting issue. Neurochem Int 62:796–802
Hirano A, Kawanami T, Llena J (1994) Electron microscopy of the blood-brain barrier in disease. Microvasc Res Tech 27:543–556
Janzer RC, Raff MC (1987) Astrocytes induce blood–brain-barrier properties in endothelial-cells. Nature 325:253–257
Joó F (1971) Increased production of coated vesicles in the brain capillaries during enhanced permeability of the blood-brain barrier. Br J Exp Pathol 52:646–649
Karuppagounder SS, Shi Q, Xu H, Gibson GE (2007) Changes in inflammatory processes associated with selective vulnerability following mild impairment of oxidative metabolism. Neurobiol Dis 26:353–362
Kniesel U, Wolburg H (2000) Tight junctions of the blood–brain barrier. Cell Mol Neurobiol 20:57–76
Kruse M, Navarro D, Desjardins P, Butterworth RF (2004) Increased brain endothelial nitric oxide synthase expression in thiamine deficiency: relationship to selective vulnerability. Neurochem Int 45:49–56
Langlais PJ, Zhang SX (1993) Extracellular glutamate is increased in thalamus during thiamine deficiency-induced lesions and is blocked by MK-801. J Neurochem 61:2175–2182
Lee S, Kang BM, Kim JH, Min J, Kim HS, Ryu H, Park H, Bae S, Oh D, Choi M, Suh M (2018) Real-time in vivo two-photon imaging study reveals decreased cerebro-vascular volume and increased blood-brain barrier permeability in chronically stressed mice. Sci Rep 8:13064
Manz HJ, Robertson DM (1972) Vascular permeability to horseradish peroxidase in brainstem lesions of thiamine-deficient rats. Am J Pathol 66:565–576
Matsushima K, MacManus P, Hakim AM (1997) Apoptosis is restricted to the thalamus in thiamine-deficient rats. Neuro Report 8:867–870
Mayhan WG, Heistad DD (1985) Permeability of blood-brain barrier to various sized molecules. Am J Phys 248(5 Pt 2):H712–H718
Moncada S, Palmer RM, Higgs EA (1991) Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol Rev 43:109–142
Murphy S, Minor RL, Welk G, Harrison DG (1990) Evidence for an astrocyte-derived vasorelaxing factor with properties similar to nitric oxide. J Neurochem 55:349–351
Ohno K, Pettigrew KO, Rapoport ST (1978) Lower limits of cerebrovascular permeability to nonelectrolytes in the conscious rat. Am J Phys 253:H299–H307
Pan W, Banks WA, Kennedy MK, Gutierrez EG, Kastin AJ (1996) Differential permeability of the BBB in acute EAE: enhanced transport of TNF-alpha. Am J Phys 271:E636–E642
Phillips SC, Cragg BG (1984) Blood-brain barrier dysfunction in thiamine-deficient, alcohol-treated rats. Acta Neuropathol (Berl) 62:235–241
Pincus JH, Wells K (1972) Regional distribution of thiamine-dependent enzymes in normal and thiamine-deficient brain. Exp Neurol 37:495–501
Prat A, Biernacki K, Wosik K, Antel JP (2001) Glial cell influence on the human blood–brain barrier. Glia 36:145–155
Reese TS, Karnovsky MJ (1967) Fine structural localization of a blood-brain barrier to exogenous peroxidase. J Cell Biol 34:207–217
Renkin EM (1959) Transport of potassium-42 from blood to tissue in isolated mammalian skeletal muscle. Am J Phys 197:1205–1210
Robertson DM, Manz HJ (1971) Effect of thiamine deficiency on the competence of the blood-brain barrier to albumin labeled with fluorescent dyes. Am J Pathol 63:393–402
Rubin LL, Barbu K, Bard F, Cannon C, Hall DE, Horner H, Janatpour M, Liaw C, Manning K, Morales J, Porter S, Tanner L, Tomaselli K, Yednock T (1991) Differentiation of brain endothelial cells in cell culture. Ann N Y Acad Sci 633:420–425
Sacks T, Moldow CF, Craddock PR, Bowers TK, Jacob HS (1978) Oxygen radicals mediate endothelial cell damage by complement-stimulated granulocytes. J Clin Invest 61:1161–1167
Sarkar S, Liachenko S, Paule MG, Bowyer J, Hanig JP (2016) Brain endothelial dysfunction following pyrithiamine induced thiamine deficiency in the rat. Neurotoxicology 57:298–309
Sisson WB, Oldendorf WH (1971) Brain distribution spaces of mannitol-3H, inulin-14C, and dextran-14C in the rat. Am J Phys 221:214–217
Sobue K, Yamamoto N, Yoneda K, Hodgson ME, Yamashiro K, Tsuruoka N, Tsuda T, Katsuya H, Miura Y, Asai K, Kato T (1999) Induction of blood-brain barrier properties in immortalized bovine brain endothelial cells by astrocytic factors. Neurosci Res 35:155–164
Troncoso JC, Johnston MV, Hess KM, Griffin JW, Price DL (1981) Model of Wernicke's encephalopathy. Arch Neurol 38:350–354
Tyson GW, Teasdale GM, Graham DI, McCulloch J (1982) Cerebrovascular permeability following MCA occlusion in the rat. The effect of halothane-induced hypotension. J Neurosurg 57:186–196
Vortmeyer AO, Colmant HJ (1988) Differentiation between brain lesions in experimental thiamine deficiency. Virchows Archiv A Pathol Anat 414:61–67
Warnock LG, Burkhalter VJ (1968) Evidence of malfunctioning blood-brain barrier in experimental thiamine deficiency in rats. J Nutr 94:256–260
Watanabe I (1978) Pyrithiamine-induced acute thiamine-deficient encephalopathy in the mouse. Exp Mol Pathol 28:381–394
Westergaard E, Brightman MW (1973) Transport of proteins across cerebral arterioles. J Comp Neurol 152:17–44
Westergaard E, van Deurs B, Brφndsted HE (1977) Increased vesicular transfer of horseradish peroxidase across cerebral endothelium, evoked by acute hypertension. Acta Neuropathol (Berl) 37:141–152
Willis CL (2011) Glia-induced reversible disruption of blood-brain barrier integrity and neuropathological response of the neurovascular unit. Toxicol Pathol 39:172–185
Witt ED (1985) Neuroanatomical consequences of thiamine deficiency: a comparative analysis. Alcohol Alcohol 20:201–222
Wolburg H, Lippoldt A (2002) Tight junctions of the blood–brain barrier: development, composition and regulation. Vasc Pharmacol 38:323–337
Yang Y, Estrada EY, Thompson JF, Liu W, Rosenberg GA (2007) Matrix metalloproteinase-mediated disruption of tight junction proteins in cerebral vessels is reversed by synthetic matrix metalloproteinase inhibitor in focal ischemia in rat. J Cereb Blood Flow Metab 27:697–709
Acknowledgements
Financial support for this study was provided by the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Contributions
ASH designed and performed all experiments. Data analysis was performed by ASH. ASH and RFB jointly contributed to the writing of the manuscript.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hazell, A.S., Butterworth, R.F. Region-selective permeability of the blood-brain barrier to α-aminoisobutyric acid during thiamine deficiency and following its reversal. Metab Brain Dis 36, 239–246 (2021). https://doi.org/10.1007/s11011-020-00644-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-020-00644-w