Abstract
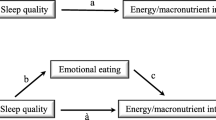
There is a relationship between extreme sleep duration and increased food intake. Some studies have reported that there was no change in the homeostatic aspects of energy balance, despite the increased nutrient intake, and in this case, the hedonic aspects may be effective. The purpose of this study was to examine the associations of hedonic hunger with sleep quality and duration among university students. This cross-sectional study was carried out on university students. An online questionnaire was applied in the study, in which 1144 participants were included. The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality and duration, and the Power of Food Scale (PFS) and Palatable Eating Motives Scale (PEMS) for detecting hedonic hunger states. Multiple linear regression analysis was performed to evaluate the relationship between sleep quality and duration and hedonic hunger by modelling. Total PFS and PEMS scores were positively associated with PSQI scores after controlling for all possible confounding factors [β (95%CI) = 0.04 (0.03–0.05), p < 0.05; 0.06 (0.05–0.07), p < 0.05, respectively). The relationship between the subdimensions of the PFS, PEMS and PSQI remained statistically significant, except for food availability (PFS) and social motive (PEMS).After fully adjusting, the odds of having a high PEMS score increased in individuals with short or long sleep duration, but not PFS score [OR (95%CI) = 1.40 (1.09–1.83), p = 0.012; 0.98 (0.70–1.21), p = 0.878, respectively]. While a positive relationship was found between increased hedonic hunger and poor sleep quality, an inverse relationship was observed between ideal sleep duration and hedonic hunger. The findings suggest that improving sleep quality and duration can help reduce hedonic hunger, which increases the tendency to unhealthy and delicious foods and plays a role in weight gain.
Similar content being viewed by others
References
Hobson JA. Sleep is of the brain, by the brain and for the brain. Nature. 2005;437:1254–6.
Singh M, Hall KA, Reynolds A, Palmer LJ, Mukherjee S. The relationship of sleep duration with ethnicity and chronic disease in a canadian general population cohort. Nat Sci Sleep. 2020;12:239–51.
Liu Y, Wheaton AG, Chapman DP, Croft JB. Sleep duration and chronic diseases among US adults age 45 years and older: evidence from the 2010 Behavioral Risk Factor Surveillance System. Sleep. 2013;36:1421–7.
Chien K-L, Chen P-C, Hsu H-C, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. 2010;33:177–84.
Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15:1456–62.
Sperry SD, Scully ID, Gramzow RH, Jorgensen RS. Sleep duration and waist circumference in adults: a meta analysis. Sleep. 2015;38:1269–76.
Capers PL, Fobian AD, Kaiser KA, Borah R, Allison DB. A systematic review and meta- analysis of randomized controlled trials of the impact of sleep duration on adiposity and components of energy balance. Obes Rev. 2015;16:771–82.
Morselli L, Leproult R, Balbo M, Spiegel K. Role of sleep duration in the regulation of glucose metabolism and appetite. Best Pract Res Clin Endocrinol Metab. 2010;24:687–702.
Kim S, DeRoo LA, Sandler DP. Eating patterns and nutritional characteristics associated with sleep duration. Public Health Nutr. 2011;14:889–95.
Xiao RS, Simas TAM, Pagoto SL, Person SD, Rosal MC, Waring ME. Sleep duration and diet quality among women within 5 years of childbirth in the United States: a cross-sectional study. Matern Child Health J. 2016;20:1869–77.
Chaput JP, Després JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obesity. 2007;15:253–61.
Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:19–34.
Calvin AD, Carter RE, Adachi T, et al. Effects of experimental sleep restriction on caloric intake and activity energy expenditure. Chest. 2013;144:79–86.
Gissoni NB, dos Santos Quaresma MVL. Short sleep duration and food intake: an overview and analysis of the influence of the homeostatic and hedonic system. Nutrire. 2020;45:1–8.
Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. Am J Clin Nutr. 2009;89:126–33.
Tan X, Chapman CD, Cedernaes J, Benedict C. Association between long sleep duration and increased risk of obesity and type 2 diabetes: a review of possible mechanisms. Sleep Med Rev. 2018;40:127–34.
Espel- Huynh H, Muratore A, Lowe M. A narrative review of the construct of hedonic hunger and its measurement by the Power of Food Scale. Obesity Sci Practice. 2018;4:238–49.
Lutter M, Nestler EJ. Homeostatic and hedonic signals interact in the regulation of food intake. J Nutr. 2009;139:629–32.
Stice E, Burger KS, Yokum S. Reward region responsivity predicts future weight gain and moderating effects of the TaqIA allele. J Neurosci. 2015;35:10316–24.
Avena NM, Rada P, Hoebel BG. Sugar and fat bingeing have notable differences in addictive-like behavior. J Nutr. 2009;139:623–8.
Benedict C, Brooks SJ, O’Daly OG, et al. Acute sleep deprivation enhances the brain’s response to hedonic food stimuli: an fMRI study. J Clin Endocrinol Metab. 2012;97:E443–7.
St-Onge M-P, O’Keeffe M, Roberts AL, RoyChoudhury A, Laferrère B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and women. Sleep. 2012;35:1503–10.
Chaput J-P, Després J-P, Bouchard C, Tremblay A. The association between short sleep duration and weight gain is dependent on disinhibited eating behavior in adults. Sleep. 2011;34:1291–7.
Blumfield ML, Bei B, Zimberg IZ, Cain SW. Dietary disinhibition mediates the relationship between poor sleep quality and body weight. Appetite. 2018;120:602–8.
Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
Öztürk M. Üniversitede eğitim-öğretim gören öğrencilerde uluslararası fiziksel aktivite anketinin geçerliliği ve güvenirliği ve fiziksel aktivite düzeylerinin belirlenmesi. Yayımlanmamış Yüksek Lisans Tezi), Ankara: Hacettepe Üniversitesi; 2005.
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry res. 1989;28:193–213.
Ağargün M, Kara H, Anlar O. Pittsburgh uyku kalitesi indeksinin geçerliği ve güvenirliği. Türk Psikiyatri Dergisi. 1996;7:107–15.
Cappelleri JC, Bushmakin AG, Gerber RA, et al. Evaluating the Power of Food Scale in obese subjects and a general sample of individuals: development and measurement properties. Internat J Obesity. 2009;33:913–22.
Hayzaran M. Üniversite öğrencilerinin hedonik açlık durumlarının farklı ölçekler ile belirlenmesi. Başkent Üniv Sağlık Bilimleri Enstitüsü. 2018;12(20):45.
Burgess E, Turan B, Lokken KL, Morse A, Boggiano MM. Profiling motives behind hedonic eating. Preliminary validation of the palatable eating motives scale. Appetite. 2014;72:66–72.
Chao AM, Grilo CM, Sinha R. Food cravings, binge eating, and eating disorder psychopathology: exploring the moderating roles of gender and race. Eat Behav. 2016;21:41–7.
Killgore WD, Yurgelun-Todd DA. Sex differences in cerebral responses to images of high vs low calorie food. NeuroReport. 2010;21:354.
Burton P, Smit HJ, Lightowler HJ. The influence of restrained and external eating patterns on overeating. Appetite. 2007;49:191–7.
Novelle MG, Diéguez C. Updating gender differences in the control of homeostatic and hedonic food intake: Implications for binge eating disorder. Mole Cell Endocrinol. 2019;3:110508.
Aliasghari F, Jafarabadi MA, Yaghin NL, Mahdavi R. Psychometric properties of power of food scale in iranian adult population: gender-related differences in hedonic hunger. Eating Weight Disorders Studies Anorexia, Bulimia Obesity. 2020;25:185–93.
Schultes B, Ernst B, Wilms B, Thurnheer M, Hallschmid M. Hedonic hunger is increased in severely obese patients and is reduced after gastric bypass surgery. Am J Clin Nutr. 2010;92:277–83.
Ullrich J, Ernst B, Wilms B, Thurnheer M, Hallschmid M, Schultes B. The hedonic drive to consume palatable foods appears to be lower in gastric band carriers than in severely obese patients who have not undergone a bariatric surgery. Obes Surg. 2013;23:474–9.
Yoshikawa T, Orita K, Watanabe Y, Tanaka M. Validation of the Japanese version of the power of food scale in a young adult population. Psychol Rep. 2012;111:253–65.
Vainik U, Neseliler S, Konstabel K, Fellows LK, Dagher A. Eating traits questionnaires as a continuum of a single concept. Uncontrolled eating Appetite. 2015;90:229–39.
Lipsky L, Nansel T, Haynie D, Liu D, Eisenberg M, Simons-Morton B. Power of food scale in association with weight outcomes and dieting in a nationally representative cohort of US young adults. Appetite. 2016;105:385–91.
Bilici S, Ayhan B, Karabudak E, Koksal E. Factors affecting emotional eating and eating palatable food in adults. Nutr Res Practice. 2020;14:70–5.
Quick V, Shoff S, Lohse B, White A, Horacek T, Greene G. Relationships of eating competence, sleep behaviors and quality, and overweight status among college students. Eat Behav. 2015;19:15–9.
Bos SC, Soares MJ, Marques M, et al. Disordered eating behaviors and sleep disturbances. Eat Behav. 2013;14:192–8.
Prospéro-García O, Amancio-Belmont O, Meléndez ALB, Ruiz-Contreras AE, Méndez-Díaz M. Endocannabinoids and sleep. Neurosci Biobehav Rev. 2016;71:671–9.
Pava MJ, Makriyannis A, Lovinger DM. Endocannabinoid signaling regulates sleep stability. PLoS ONE. 2016;11:e0152473.
Almoosawi S, PallaL WI, Vingeliene S, Ellis JG. Long Sleep Duration and social jetlag are associated ınversely with a healthy dietary pattern in adults: results from the UK national diet and nutrition survey rolling programme Y1–4. Nutrients. 2018;10:1131–50.
Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36:981–90.
Hart CN, Carskadon MA, Demos KE, et al. Acute changes in sleep duration on eating behaviors and appetite-regulating hormones in overweight/obese adults. Behav Sleep Med. 2015;13:424–36.
Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality. Nutr Res. 2012;32:309–19.
Chaput J-P. Sleep patterns, diet quality and energy balance. Physiol Behav. 2014;134:86–91.
Acknowledgments
This study was not supported by any institution or organization. We would like to express our gratitude to Ankara University students for their help in data collection. I also make a present of this article to my Hayal baby. So glad I have you, Hayal!
Author information
Authors and Affiliations
Contributions
MA and ANBS contributed in conception, search, statistical analyses and manuscript drafting. MA, ANBS and FPÇ contributed in data interpretation and design. All authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Açik, M., Bozdağ, A.N.S. & Çakiroğlu, F.P. The quality and duration of sleep are related to hedonic hunger: a cross-sectional study in university students. Sleep Biol. Rhythms 19, 163–172 (2021). https://doi.org/10.1007/s41105-020-00303-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-020-00303-8