Abstract
Introduction
Drooling is characterized by an excessive pooling of saliva in the oral cavity. The exact pathophysiological mechanism of drooling in Parkinson’s disease (PD) is not yet fully understood.
Objective
To identify the relationship between drooling and other clinical features in people diagnosed with PD.
Method
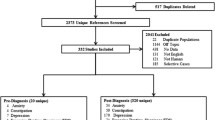
Research on the topic was carried out on the PubMed and ScienceDirect electronic databases. Articles published between March 2015 and March 2020 were selected. Search terms and inclusion and exclusion criteria were previously defined. The articles included met those requirements.
Results
Sixteen articles were included for analysis. The prevalence of drooling varies between 9.26 and 70% and can occur at any stage of the disease. Higher prevalence of drooling is related to disease duration, disease severity, older age, male, levodopa equivalent dose, hypomimia, dysphagia, dysarthria, cognition, sleep, non-dominant tremor, motor fluctuations, bradykinesia, more symmetric pattern, gastrointestinal and urinary problems, sexual dysfunction, obstipation, and orthostatic hypotension. However, it is not related to hallucinations, rapid eye movement sleep behavior disorder, akinetic-rigid PD, mixed, nor dyskinesias.
Conclusion
Drooling is not caused by a single factor; it is influenced and related to several clinical features. Some clinical factors participate in the onset of drooling while others are concomitant.

Similar content being viewed by others
References
Fasano A, Visanji NP, Liu LWC, Lang AE, Pfeiffer RF (2015) Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol 14:625–639
Nicaretta DH, Rosso AL, de Mattos JP, Maliska C, Costa MMB (2013) Dysphagia and sialorrhea: the relationship to Parkinson’s disease. Arq Gastroenterol 50:42–49
Damian A, Adler CH, Hentz JG, Sabbagh M, Evidente VG, Beach TG et al (2012) Autonomic function, as self-reported on the SCOPA-autonomic questionnaire, is normal in essential tremor but not in Parkinson’s disease. Parkinsonism Relat Disord 18:1089–1093
Scott B, Borgman A, Engler H, Johnels B, Aquilonius SM (2000) Gender differences in Parkinson’s disease symptom profile. Acta Neurol Scand 102:37–43
Skelly R, Lindop F, Johnson C (2012) Multidisciplinary care of patients with Parkinson’s disease. Prog Neurol Psychiatry 16:10–14
Srivanitchapoom P, Pandey S, Hallett M (2014) Drooling in Parkinson’s disease: a review. Parkinsonism Relat Disord. Elsevier ltd;20:1109–18. Available from: https://doi.org/10.1016/j.parkreldis.2014.08.013
Tumilasci OR, Cersósimo MG, Belforte JE, Micheli FE, Benarroch EE, Pazo JH (2006) Quantitative study of salivary secretion in Parkinson’s disease. Mov Disord 21:660–667
Karakoc M, Yon MI, Cakmakli GY, Ulusoy EK, Gulunay A, Oztekin N, Ak F (2016) Pathophysiology underlying drooling in Parkinson’s disease: oropharyngeal bradykinesia. Neurol Sci 37:1987–1991
Nóbrega AC, Rodrigues B, Melo A (2008) Silent aspiration in Parkinson’s disease patients with diurnal sialorrhea. Clin Neurol Neurosurg 110:117–119
Yoritaka A, Shimo Y, Takanashi M, Fukae J, Hatano T, Nakahara T, et al (2013) Motor and non-motor symptoms of 1453 patients with Parkinson’s disease: prevalence and risks. Parkinsonism Relat Disord. Elsevier ltd;19:725–31. Available from: https://doi.org/10.1016/j.parkreldis.2013.04.001
Leopold NA, Kagel MC (1997) Laryngeal deglutition movement in Parkinson’s disease. Neurology. 48:373–375
Leopold NA, Kagel MC (1997) Pharyngo-esophageal dysphagia in Parkinson’s disease. Dysphagia. 18:11–18
Merello M (2008) Sialorrhoea and drooling in patients with Parkinson’s disease: epidemiology and management. Drugs Aging 25:1007–1019
Miller N, Walshe M, Walker RW (2019) Sialorrhea in Parkinson’s disease : prevalence, impact and management strategies. Res Rev Park 9:17–28
National Institute for Health and Care Excellence. Parkinson’s Disease in Adults: NICE Guideline NG71. NICE. 2017;
Mao CJ, Xiong YT, Wang F, Yang YP, Yuan W, Zhu C, Chen J, Liu CF (2018) Motor subtypes and other risk factors associated with drooling in Parkinson’s disease patients. Acta Neurol Scand 137:509–514
van Wamelen DJ, Leta V, Johnson J, Ocampo CL, Podlewska AM, Rukavina K et al (2020) Drooling in Parkinson’s disease: prevalence and progression from the non-motor international longitudinal study. Dysphagia. Springer US; Available from:. https://doi.org/10.1007/s00455-020-10102-5
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Ou R, Guo X, Wei Q, Cao B, Yang J, Song W, et al (2015) Diurnal drooling in Chinese patients with Parkinson’s disease. J Neurol Sci. Elsevier B.V.;353:74–8. Available from: https://doi.org/10.1016/j.jns.2015.04.007
Barbe AG, Bock N, Derman SHM, Felsch M, Timmermann L, Noack MJ (2017) Self-assessment of oral health, dental health care and oral health-related quality of life among Parkinson’s disease patients. Gerodontology. 34:135–143
Malek N, Lawton MA, Grosset KA, Bajaj N, Barker RA, Burn DJ, Foltynie T, Hardy J, Morris HR, Williams NM, Ben-Shlomo Y, Wood NW, Grosset DG, the PRoBaND Clinical Consortium (2017) Autonomic dysfunction in early Parkinson’s disease: results from the United Kingdom tracking Parkinson’s study. Mov Disord Clin Pract 4:509–516
Reynolds H, Miller N, Walker R (2018) Drooling in Parkinson’s disease: evidence of a role for divided attention. Dysphagia. Springer US;33:809–17. Available from: https://doi.org/10.1007/s00455-018-9906-7
Fereshtehnejad SM, Skogar Ö, Lökk J (2017) Evolution of Orofacial symptoms and disease progression in idiopathic Parkinson’s disease: longitudinal data from the Jönköping Parkinson registry. Parkinsons Dis. 2017
Nienstedt JC, Buhmann C, Bihler M, Niessen A, Plaetke R, Gerloff C et al (2018) Drooling is no early sign of dysphagia in Parkinson′s disease. Neurogastroenterol Motil 30:1–6
Uludag IF, Tiftikcioglu BI, Ertekin C (2016) Spontaneous swallowing during all-night sleep in patients with Parkinson disease in comparison with healthy control subjects. Sleep. 39:847–854
Stanković I, Petrović I, Pekmezović T, Marković V, Stojković T, Dragašević-Mišković N, Svetel M, Kostić V (2019) Longitudinal assessment of autonomic dysfunction in early Parkinson’s disease. Parkinsonism Relat Disord 66:74–79
Sánchez-Martínez CM, Choreño-Parra JA, Placencia-Álvarez N, Nuñez-Orozco L, Guadarrama-Ortiz P (2019) Frequency and dynamics of non-motor symptoms presentation in Hispanic patients with Parkinson disease. Front Neurol 10:1–13
Leclair-Visonneau L, Magy L, Volteau C, Clairembault T, Le Dily S, Préterre C, et al (2018) Heterogeneous pattern of autonomic dysfunction in Parkinson’s disease. J Neurol. Springer Berlin Heidelberg;265:933–41. Available from: https://doi.org/10.1007/s00415-018-8789-8
Durcan R, Wiblin L, Lawson RA, Khoo TK, Yarnall AJ, Duncan GW, Brooks DJ, Pavese N, Burn DJ, the ICICLE-PD Study Group (2019) Prevalence and duration of non-motor symptoms in prodromal Parkinson’s disease. Eur J Neurol 26:979–985
Qin X, Li X, Xin Z, Li Z (2019) Gastrointestinal dysfunction in Chinese patients with Parkinson’s disease. Parkinsons Dis 2019
Zhang G, Zhang Z, Liu L, Yang J, Huang J, Xiong N et al (2014) Impulsive and compulsive behaviors in Parkinson’s disease. Front Aging Neurosci 6:1–11
Zhang TM, Yu SY, Guo P, Du Y, Hu Y, Piao YS et al (2016) Nonmotor symptoms in patients with Parkinson disease: a cross-sectional observational study. Medicine (United States) 95:e5400
Luchesi KF, Kitamura S, Mourão LF (2015) Dysphagia progression and swallowing management in Parkinson’s disease: an observational study. Braz J Otorhinolaryngol 81:24–30 Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1808-86942015000100024
Kalf JG, Munneke M, van den Engel-Hoek L, de Swart BJ, Borm GF, Bloem BR, Zwarts MJ (2011) Pathophysiology of diurnal drooling in Parkinson’s disease. Mov Disord 26:1670–1676
Rana AQ, Yousuf MS, Awan N, Fattah A (2012) Impact of progression of Parkinson’s disease on drooling in various ethnic groups. Eur Neurol 67:312–314
Proulx M, de Courval FP, Wiseman MA, Panisset M (2005) Salivary production in Parkinson’s disease. Mov Disord 20:204–207
Zlotnik Y, Balash Y, Korczyn AD, Giladi N, Gurevich T (2015) Disorders of the oral cavity in Parkinson’s disease and parkinsonian syndromes. Parkinsons Dis 2015
Cantuti-Castelvetri I, Keller-McGandy C, Bouzou B, Asteris G, Clark TW, Frosch MP, Standaert DG (2007) Effects of gender on nigral gene expression and Parkinson disease. Neurobiol Dis 26:606–614
Haaxma CA, Bloem BR, Borm GF, Oyen WJG, Leenders KL, Eshuis S, Booij J, Dluzen DE, Horstink MWIM (2007) Gender differences in Parkinson’s disease. J Neurol Neurosurg Psychiatry 78:819–824
De Lau L, Breteler M (2011) Epidemiology of Parkinson’s disease. Rev Neurol (Paris) 5:525–535
Conforti R, Capasso R, Negro A, Della Gatta L, De Cristofaro M, Amato M, Giganti M, Genovese EA (2013) Diagnostic tools in neurodegenerative disorders of adult-elderly. Recenti Prog Med 7:295–298
Morgan J, Sethi KD (2005) Levodopa and the progression of Parkinson’s disease. Curr Neurol Neurosci Rep 5:261–262
Kalf JG, Smit AM, Bloem BR, Zwarts MJ, Munneke M (2007) Impact of drooling in Parkinson’s disease. J Neurol 254:1227–1232
Cotzias GC, Van Woert MH, Schiffer LM (1967) Aromatic amino acids and modification of parkinsonism. N Engl J Med 276:374–379
Pandey S, Srivanitchapoom P (2017) Levodopa-induced dyskinesia: clinical features, pathophysiology, and medical management. Ann Indian Acad Neurol 20:190–198
Calabresi P, Di Filippo M, Ghiglieri V, Tambasco N, Picconi B (2010) Levodopa-induced dyskinesias in patients with Parkinson’s disease: filling the bench-to-bedside gap. Lancet Neurol:1106–1117
Santens P, de Noordhout AM, Cras P, Dethy S, Flamez A, Gonce M et al (2006) Detection of motor and non-motor symptoms of end-of dose wearing-off in Parkinson’s disease using a dedicated questionnaire: a Belgian multicenter survey. Acta Neurol Belg 106:137–141
Rana AQ, Khondker S, Kabir A, Owalia A, Khondker S, Emre M (2013) Impact of cognitive dysfunction on drooling in Parkinson’s disease. Eur Neurol 70:42–45
Troche MS, Okun MS, Rosenbek JC, Altmann LJ, Sapienza CM (2014) Attentional resource allocation and swallowing safety in Parkinson’s disease: a dual task study. Parkinsonism Relat Disord. Elsevier ltd;20:439–43. Available from: https://doi.org/10.1016/j.parkreldis.2013.12.011
Politis M, Wu K, Molloy S, Bain PG, Chaudhuri KR, Piccini P (2010) Parkinson’s disease symptoms: the patient’s perspective. Mov Disord 25:1646–1651
Leibner J, Ramjit A, Sedig L, Dai Y, Wu SS, Jacobson C, et al (2010) The impact of and the factors associated with drooling in Parkinsons disease. Parkinsonism Relat Disord. Elsevier ltd ;16:475–7. Available from: https://doi.org/10.1016/j.parkreldis.2009.12.003
Merello A, Colosimo C, Hoffman M, Starkstein S, Leiguarda R (1997) Sleep benefit in Parkinson’s disease. Mov Disord 12:506–508
Ding C, Palmer CJ, Hohwy J, Youssef GJ, Paton B, Tsuchiya N, et al (2017) Parkinson’s disease alters multisensory perception: insights from the rubber hand illusion. Neuropsychologia. Elsevier ltd; 97:38–45. Available from: https://doi.org/10.1016/j.neuropsychologia.2017.01.031
Bushmann M, Dobmeyer SM, Leeker L, Perlmutter JS (1989) Swallowing abnormalities and their response to treatment in Parkinson’s disease. Neurology 39
Meningaud JP, Pitak-Arnnop P, Chikhani L, Bertrand JC (2006) Drooling of saliva: a review of the etiology and management options. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:48–57
Leopold NA, Kagel MC (1996) Prepharyngeal dysphagia in Parkinson’s disease. Dysphagia. 22:14–22
Baijens LWJ, Speyer R, Passos VL, Pilz W, Roodenburg N, Clave P (2011) Swallowing in Parkinson patients versus healthy controls: reliability of measurements in videofluoroscopy. Gastroenterol Res Pract 2011:1–9
Rosenberg-Katz K, Herman T, Jacob Y, Giladi N, Hendler T, Hausdorff JM (2013) Gray matter atrophy distinguishes between Parkinson disease motor subtypes. Neurology. 80:1476–1484
Selikhova M, Williams DR, Kempster PA, Holton JL, Revesz T, Lees AJ (2009) A clinico-pathological study of subtypes in Parkinson’s disease. Brain. 132:2947–2957
Umemoto G, Furuya H, Tsuboi Y, Fujioka S, Arahata H, Sugahara M et al (2017) Dysphagia in multiple system atrophy of cerebellar and Parkinsonian types. J Neurol Neurosci 08:1–8 Available from: http://www.jneuro.com/neurology-neuroscience/dysphagia-in-multiple-system-atrophy-of-cerebellar-and-parkinsonian-types.php?aid=18113
Marinus J, van Hilten JJ (2015) The significance of motor (A)symmetry in Parkinson’s disease. Mov Disord 30:379–385
Schiffman SS, Miletic ID (1996) Effect of taste and smell on secretion rate of salivary IgA in elderly and young persons. Physiol Behav. Elsevier Inc.;60:243–8
Proserpio C, de Graaf C, Laureati M, Pagliarini E, Boesveldt S (2017) Impact of ambient odors on food intake, saliva production and appetite ratings. Physiol Behav. Elsevier Inc.;174:35–41
Kashihara K, Hanaoka A, Imamura T (2011) Frequency and characteristics of taste impairment in patients with Parkinson’s disease: results of a clinical interview. Intern Med 50:2311–2315 Available from: https://pubmed.ncbi.nlm.nih.gov/22001456/
Ruiz-Roca J, Pons-Fuster E, Lopez-Jornet P (2019) Effectiveness of the botulinum toxin for treating sialorrhea in patients with Parkinson’s disease: a systematic review. J Clin Med. MDPI AG; [cited 2020 Oct 27];8:317. Available from: /pmc/articles/PMC6463012/?report=abstract
Hyson HC, Johnson AM, Jog MS (2002) Sublingual atropine for sialorrhea secondary to parkinsonism: a pilot study. Mov Disord; [cited 2020 Oct 27];17:1318–20. Available from: https://pubmed.ncbi.nlm.nih.gov/12465075/
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there is no conflict of interest.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nascimento, D. Clinical features associated with drooling in Parkinson’s disease. Neurol Sci 42, 895–903 (2021). https://doi.org/10.1007/s10072-020-05005-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-05005-0