Abstract
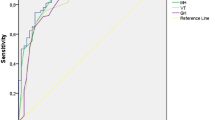
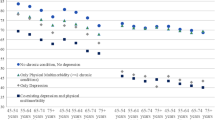
This study aimed to present normative data of Quality of life (QoL) and to evaluate the relationship between sociodemographic factors, multidimensional QoL and depression. A questionnaire including the Short Form-12 (SF-12) for physical and mental health-related QOL (HRQOL), the McGill Quality of Life questionnaire (MQOL) for existential well-being and social support-related QOL, and the Patient Health Questionnaire-9 (PHQ-9) for depressive symptoms was designed and administered to 1200 Korean participants as part of a population-based survey. The MQOL of the entire and female population decreased notably with age (p < 0.001 for both), and women, 40-years-old individuals, and religious individuals had higher physical HRQOL (adjusted odds ratio [aOR] = 1.67, 2.14, and 1.31), and persons older than 40 years of age and with an income of >$3000 reported a better mental HRQOL (aOR = 1.42 and 1.38). Those who were educated at higher than college level or were religious reported a worse mental HRQOL (aOR = 0.70 and 0.69). Unlike QOL measured by the SF-12, MQOL was lower among women (aOR = 0.77) and participants who were divorced or separated (aOR = 0.23 for existential well-being and 0.40 for social support). Participants who were educated at higher than college level (aOR = 1.51) and those living in a city/country reported a better MQOL (aOR = 1.50 for existential well-being and 1.60 for social support). Among the QOL scores that were significantly related to depression, existential well-being-related QOL had the highest aOR (aOR = 38.15), followed by physical HRQOL score (aOR = 4.52). Further consideration is needed to raise awareness of the need for evaluating multidimensional QOL in the general population.
Similar content being viewed by others
References
Akosile, C. O., Mgbeojedo, U. G., Maruf, F. A., Okoye, E. C., Umeonwuka, I. C., & Ogunniyi, A. (2018). Depression, functional disability and quality of life among Nigerian older adults: Prevalences and relationships. Archives of Gerontology and Geriatrics, 74, 39–43.
Arber, S., & Cooper, H. (1999). Gender differences in health in later life: the new paradox? Social Science & Medicine, 48(1), 61–76.
Bjornnes, A. K., Parry, M., Falk, R., Watt-Watson, J., Lie, I., & Leegaard, M. (2017). Impact of marital status and comorbid disorders on health-related quality of life after cardiac surgery. Quality of Life Research, 26(9), 2421–2434. https://doi.org/10.1007/s11136-017-1589-2.
Brazier, J. E., & Roberts, J. (2004). The estimation of a preference-based measure of health from the SF-12. Medical Care, 851–859.
Carr, A. J., Gibson, B., & Robinson, P. G. (2001). Is quality of life determined by expectations or experience? British Medical Journal, 322(7296), 1240–1243.
Charles, S. T., & Carstensen, L. L. (2010). Social and emotional aging. Annual Review of Psychology, 61, 383–409.
Cherepanov, D., Palta, M., Fryback, D. G., Robert, S. A., Hays, R. D., & Kaplan, R. M. (2011). Gender differences in multiple underlying dimensions of health-related quality of life are associated with sociodemographic and socioeconomic status. Medical Care, 49(11), 1021.
Chung, L., Pan, A.-W., & Hsiung, P.-C. (2009). Quality of life for patients with major depression in Taiwan:A model-based study of predictive factors. Psychiatry Research, 168(2), 153–162. https://doi.org/10.1016/j.psychres.2008.04.003.
Cohen, S. R., Mount, B. M., Strobel, M. G., & Bui, F. (1995). The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliative Medicine, 9(3), 207–219.
Ferrans, C. E. (2010). Advances in measuring quality-of-life outcomes in cancer care. Seminars in Oncology Nursing, 26(1), 2–11. https://doi.org/10.1016/j.soncn.2009.11.002.
Fleishman, J. A., & Lawrence, W. F. (2003). Demographic variation in SF-12 scores: true differences or differential item functioning? Medical Care, 41(7 Suppl), III75–III86. https://doi.org/10.1097/01.mlr.0000076052.42628.cf.
Galenkamp, H., Stronks, K., Mokkink, L. B., & Derks, E. M. (2018). Measurement invariance of the SF-12 among different demographic groups: The HELIUS study. PLoS One, 13(9), e0203483. https://doi.org/10.1371/journal.pone.0203483.
Group, T. W. (1998). The World Health Organization quality of life assessment (WHOQOL): development and general psychometric properties. Social Science & Medicine, 46(12), 1569–1585.
Gutierrez-Vega, M., Esparza-Del Villar, O. A., Carrillo-Saucedo, I. C., & Montanez-Alvarado, P. (2018). The Possible Protective Effect of Marital Status in Quality of Life Among Elders in a U.S.-Mexico Border City. Community Mental Health Journal, 54(4), 480–484. https://doi.org/10.1007/s10597-017-0166-z.
Kim, S.-H., Jo, M.-W., Ahn, J., Ock, M., Shin, S., & Park, J. (2014). Assessment of psychometric properties of the Korean SF-12 v2 in the general population. BMC Public Health, 14, 1086–1086. https://doi.org/10.1186/1471-2458-14-1086.
Kontis, V., Bennett, J. E., Mathers, C. D., Li, G., Foreman, K., & Ezzati, M. (2017). Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. The Lancet, 389(10076), 1323–1335.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613.
Leach, L. S., Christensen, H., Mackinnon, A. J., Windsor, T. D., & Butterworth, P. (2008). Gender differences in depression and anxiety across the adult lifespan: the role of psychosocial mediators. Social Psychiatry and Psychiatric Epidemiology, 43(12), 983–998.
Mackenbach, J. P., Stirbu, I., Roskam, A.-J. R., Schaap, M. M., Menvielle, G., Leinsalu, M., et al. (2008). Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine, 358(23), 2468–2481.
Maruish, M. E., & DeRosa, M. A. (2009). A guide to the integration of certified Short Form survey scoring and data quality evaluation capabilities. Lincoln: Quality Metric Incorporated.
Otto, C., Haller, A.-C., Klasen, F., Hölling, H., Bullinger, M., Ravens-Sieberer, U., et al. (2017). Risk and protective factors of health-related quality of life in children and adolescents: Results of the longitudinal BELLA study. PLoS One, 12(12), e0190363–e0190363. https://doi.org/10.1371/journal.pone.0190363.
Park, H., & Kim, K. (2018). Depression and Its Association with Health-Related Quality of Life in Postmenopausal Women in Korea. International Journal of Environmental Research and Public Health, 15(11), E2327. https://doi.org/10.3390/ijerph15112327.
Perkins, A. J., Stump, T. E., Monahan, P. O., & McHorney, C. A. (2006). Assessment of differential item functioning for demographic comparisons in the MOS SF-36 health survey. Quality of Life Research, 15(3), 331–348.
Priebe, S., Reininghaus, U., McCabe, R., Burns, T., Eklund, M., Hansson, L., et al. (2010). Factors influencing subjective quality of life in patients with schizophrenia and other mental disorders: a pooled analysis. Schizophrenia Research, 121(1–3), 251–258.
Prince, M., Patel, V., Saxena, S., Maj, M., Maselko, J., Phillips, M. R., et al. (2007). No health without mental health. The Lancet, 370(9590), 859–877.
Ravindran, A. V., Matheson, K., Griffiths, J., Merali, Z., & Anisman, H. (2002). Stress, coping, uplifts, and quality of life in subtypes of depression: a conceptual frame and emerging data. Journal of Affective Disorders, 71(1–3), 121–130.
Rayan, A., & Mahroum, M. H. (2016). The correlates of quality of life among Jordanian patients with major depressive disorder. Research in Psychology and Behavioral Sciences, 4(2), 28–33.
Shumye, S., Belayneh, Z., & Mengistu, N. (2019). Health related quality of life and its correlates among people with depression attending outpatient department in Ethiopia: a cross sectional study. Health and Quality of Life Outcomes, 17(1), 169–169. https://doi.org/10.1186/s12955-019-1233-7.
Silva, M. T., Caicedo Roa, M., & Galvao, T. F. (2017). Health-related quality of life in the Brazilian Amazon: a population-based cross-sectional study. Health and Quality of Life Outcomes, 15(1), 159–159. https://doi.org/10.1186/s12955-017-0734-5.
Sivertsen, H., Bjorklof, G. H., Engedal, K., Selbaek, G., & Helvik, A. S. (2015). Depression and Quality of Life in Older Persons: A Review. Dementia and Geriatric Cognitive Disorders, 40(5–6), 311–339. https://doi.org/10.1159/000437299.
Skevington, S. M., & McCrate, F. M. (2012). Expecting a good quality of life in health: assessing people with diverse diseases and conditions using the WHOQOL-BREF. Health Expectations : an International Journal of Public Participation in Health Care and Health Policy, 15(1), 49–62. https://doi.org/10.1111/j.1369-7625.2010.00650.x.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Group, P. H. Q. P. C. S. (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Journal of the American Medical Association, 282(18), 1737–1744.
Sun, Y., Yang, Z., Wan, C., Xu, C., Chen, L., Xu, L., et al. (2018). Development and validation of the pulmonary tuberculosis scale of the system of Quality of Life Instruments for Chronic Diseases (QLICD-PT). Health and Quality of Life Outcomes, 16(1), 137. https://doi.org/10.1186/s12955-018-0960-5.
van Leeuwen, M., Husson, O., Alberti, P., Arraras, J. I., Chinot, O. L., Costantini, A., et al. (2018). Understanding the quality of life (QOL) issues in survivors of cancer: towards the development of an EORTC QOL cancer survivorship questionnaire. Health and Quality of Life Outcomes, 16(1), 114. https://doi.org/10.1186/s12955-018-0920-0.
Ware, J. E., Keller, S. D., & Kosinski, M. (1995). SF-12: How to score the SF-12 physical and mental health summary scales: Health Institute, New England Medical Center.
Availability of Data and Materials
The raw data are being kept in the custody of Seoul National University Medical College and are available upon request.
Funding
This study was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) and by the Ministry of Health & Welfare, Republic of Korea (Grant number: HI16C0455). None of the funding organizations had any role in the design of the study, analysis, or interpretation of the data, or in the preparation, review, and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
YHY contributed to the ideas in this paper. EKK contributed the writing and analyses. YHY, EKK, YER, SK, JL contributed to the design, interpretation of the data and analyses and had valuable critics of the draft. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no competing interests to declare.
Ethics Approval and Consent to Participate
Informed consent to participate in this public survey is obtained from all participants. Interested and eligible participants receive information about the study of verbal recording.
Consent to Publish
Not Applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, E., Rhee, Y.E., Kim, S. et al. Quality of Life and Depression in the General Korean Population: Normative Data and Associations of the 12-Item Short Form Health Survey (SF-12) and the McGill Quality of Life Questionnaire (MQOL) with Depression (Patient Health Questionnaire-9) and Socioeconomic Status. Applied Research Quality Life 16, 1673–1687 (2021). https://doi.org/10.1007/s11482-020-09838-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-020-09838-x