Abstract
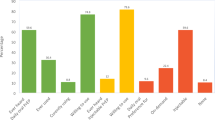
Pre-exposure prophylaxis (PrEP) represents a viable HIV prevention tool for black men who have sex with men (BMSM). However, aggregated evidence regarding the presentations and determinants of the PrEP continuum (e.g., awareness, willingness, intention, uptake and adherence) remains absent to empirically inform future intervention efforts. We meta-analytically summarized the prevalence and qualitatively synthesized key barriers/facilitators of the stages of the PrEP continuum among a pooled sample of 42,870 BMSM aggregated from 56 published studies. Our random-effect models indicated a pooled prevalence of PrEP awareness (50.8%, 95% CI: 43.6–58.0%, willingness/intention (58.2%, 95% CI: 52.0–68.1%) and uptake (15.5%, 95% CI: 12.8–18.2%). Qualitative summary revealed that perception of HIV risk, intersectional/PrEP-related stigma and medical mistrust were among the most quoted factors that influence PrEP use. BMSM remain underrepresented in key stages of the PrEP continuum. Futures interventions are continuously needed to target multilevel barriers/facilitators to enhance the PrEP continuum among BMSM.


Similar content being viewed by others
References
Singh S. HIV care outcomes among men who have sex with men with diagnosed HIV infection — United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:969–74.
Kanny D. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men — 23 urban areas, 2017. MMWR Morb Mortal Wkly Rep. 2019;68:2706.
HIV Surveillance Report 2018 (Preliminary) Available from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-preliminary-vol-30.pdf. Accessed 17 July 2020.
Antoni G, Tremblay C, Delaugerre C, Charreau I, Cua E, Rojas Castro D, Raffi F, Chas J, Huleux T, Spire B, Capitant C, Cotte L, Meyer L, Molina JM, ANRS IPERGAY study group. On-demand pre-exposure prophylaxis with tenofovir disoproxil fumarate plus emtricitabine among men who have sex with men with less frequent sexual intercourse: a post-hoc analysis of the ANRS IPERGAY trial. Lancet HIV. 2020;7(2):e113–20. https://doi.org/10.1016/S2352-3018(19)30341-8.
US Food and Drug Administration. Truvada approved to reduce the risk of sexually transmitted HIV in people who are infected with the virus.2012 Available from http://www.fda.gov/ForConsumers/ByAudience/ForPatientAdvocates/HIVandAIDSActivities/ucm312264.htm. Accessed 17 July 2020
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Elion RA, Kabiri M, Mayer KH, Wohl DA, Cohen J, Beaubrun AC, et al. Estimated impact of targeted pre-exposure prophylaxis: strategies for men who have sex with men in the United States. Int J Environ Res Public Health. 2019;16(9):1592.
Kasaie P, Pennington J, Shah MS, Berry SA, German D, Flynn CP, et al. The impact of pre-exposure prophylaxis among men who have sex with men: an individual-based model. J Acquir Immune Defic Syndr. 2017;75(2):175–83.
Huang YA, Zhu W, Smith DK, Harris N, Hoover KW. HIV preexposure prophylaxis, by race and ethnicity — United States, 2014–2016. MMWR Morb Mortal Wkly Rep. 2018;67(41):1147–50.
Hoots BE, Finlayson T, Nerlander L, Paz-Bailey G. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men—20 US cities, 2014. Clin Infect Dis. 2016;63(5):672–7.
Finlayson T, Cha S, Xia M, Trujillo L, Denson D, Prejean J, et al. Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men — 20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68(27):597–603.
Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of pre-exposure prophylaxis (prep) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDS. 2015;29(8):423–30.
Caponi M, Burgess C, Leatherwood A, Molano LF. Demographic characteristics associated with the use of HIV pre-exposure prophylaxis (PrEP) in an urban, community health center. Prev Med Rep. 2019;14:15.
Garcia J, Parker RG, Parker C, Wilson PA, Philbin M, Hirsch JS. The limitations of ‘Black MSM’ as a category: why gender, sexuality, and desire still matter for social and biomedical HIV prevention methods. Glob Public Health. 2016;11(7–8):1026–48.
Sanders RA, Morgan A, Oidtman J, Qian I, Celentano D, Beyrer C. A medical care missed opportunity: pre-exposure prophylaxis and young black men who have sex with men (ybmsm). J Adolesc Health. 2016;59(6):725–8.
Garcia J, Parker C, Parker RG, Wilson PA, Philbin M, Hirsch JS. Psychosocial implications of family and religious homophobia: insights for HIV combination prevention among black men who have sex with men. Health Educ Behav. 2016;43(2):217–25.
Rogers BG, Whiteley L, Haubrick KK, Mena LA, Brown LK. Intervention messaging about pre-exposure prophylaxis use among young, black sexual minority men. AIDS Patient Care and STDs. 2019;33(11):473–81.
Brooks RA, Nieto O, Landrian A, Fehrenbacher A, Cabral A. Experiences of pre-exposure prophylaxis (prep)–related stigma among black MSM PrEP users in Los Angeles. J Urban Health. 2019;97(5):679–91.
Elopre L, McDavid C, Brown A, Shurbaji S, Mugavero MJ, Turan JM. Perceptions of HIV pre-exposure prophylaxis among young, black men who have sex with men. AIDS Patient Care STDS. 2018;32(12):511–8.
Quinn K, Bowleg L, Dickson-Gomez J. “The fear of being black plus the fear of being gay”: the effects of intersectional stigma on PrEP use among young black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2019;232:86–93.
Mutchler MG, McDavitt B, Ghani MA, Nogg K, Winder TJA, Soto JK. Getting PrEPared for HIV prevention navigation: young black gay men talk about HIV prevention in the biomedical era. AIDS Patient Care STDS. 2015;29(9):490–502.
Thomann M, Zapata R, Grosso A, Chiasson MA. “WTF is PrEP?”: attitudes towards pre-exposure prophylaxis among men who have sex with men and transgender women in New York city. Cult Health Sex. 2018;20(7):772–86.
Smith DK, Toledo L, Smith DJ, Adams MA, Rothenberg R. Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PrEP). AIDS Educ Prev. 2012;24(5):408–21.
Fields EL, Thornton N, Long A, Morgan A, Uzzi M, Arrington-Sanders R, et al. Young black MSM’s exposures to and discussions about prep while navigating geosocial networking apps. J LGBT Youth. 2019;18(1):23–39.
Quinn K, Dickson-Gomez J, Zarwell M, Pearson B, Lewis M. “A gay man and a doctor are just like, a recipe for destruction”: how racism and homonegativity in healthcare settings influence PrEP uptake among young black MSM. AIDS Behav. 2019;23(7):1951–63.
Khanna AS, Michaels S, Skaathun B, Morgan E, Green K, Young L, et al. Pre-exposure prophylaxis (PrEP) awareness and use in a population-based sample of young black men who have sex with men. JAMA Intern Med. 2016;176(1):136–8.
Misra K, Udeagu CC. Disparities in awareness of HIV postexposure and preexposure prophylaxis among notified partners of HIV-positive individuals, New York city 2015–2017. JAIDS. 2017;76(2):132–40.
Fallon SA, Park JN, Ogbue CP, Flynn C, German D. Awareness and acceptability of pre-exposure HIV prophylaxis among men who have sex with men in Baltimore. AIDS Behav. 2017;21(5):1268–77.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. PLoS Med. 2009;6(7):e1000097.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Zhang C, McMahon J, Simmons J, Brown LL, Nash R, Liu Y. Suboptimal HIV pre-exposure prophylaxis awareness and willingness to use among women who use drugs in the United States: a systematic review and meta-analysis. AIDS Behav. 2019;23(10):2641–53.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Millett GA, Flores SA, Marks G, Reed JB, Herbst JH. Circumcision status and risk of HIV and sexually transmitted infections among men who have sex with men: a meta-analysis. JAMA. 2008;300(14):1674–84.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Viechtbauer W, Cheung MW. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1(2):112–25.
Shi L, Lin L. The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Medicine. 2019;98(23):e15987.
Kamitani E, Wichser ME, Adegbite AH, Mullins MM, Johnson WD, Crouch P-C, et al. Increasing prevalence of self-reported HIV preexposure prophylaxis use in published surveys: a systematic review and meta-analysis. AIDS. 2018;32(17):2633–5.
Pérez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of prep uptake among racially/ethnically diverse young men who have sex with men: the p18 study. AIDS Educ Prev. 2015;27(2):112–25.
Bauermeister JA, Meanley S, Pingel E, Soler JH, Harper GW. PrEP awareness and perceived barriers among single young men who have sex with men in the United States. Curr HIV Res. 2013;11(7):520–7.
Mustanski B, Johnson AK, Garofalo R, Ryan D, Birkett M. Perceived likelihood of using HIV pre-exposure prophylaxis medications among young men who have sex with men. AIDS Behav. 2013;17(6):2173–9.
Wejnert C, Hess KL, Rose CE, Balaji A, Smith JC, Paz-Bailey G, et al. Age-specific race and ethnicity disparities in HIV infection and awareness among men who have sex with men—20 US cities, 2008–2014. J Infect Dis. 2016;213(5):776–83.
Zhang C, McMahon J, Fiscella K, Przybyla S, Braksmajer A, LeBlanc N, Liu Y. HIV pre-exposure prophylaxis implementation cascade among health care professionals in the united states: implications from a systematic review and meta-analysis. AIDS patient care and STDs. 2019;33(12):507–27.
Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, Krakower D, Novak DS, Mimiaga MJ, Mayer KH. State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS. 2015;29(7):837–45. https://doi.org/10.1097/QAD.0000000000000622.
HIV Healthy People 2020. Available from https://www.healthypeople.gov/2020/topics-objectives/topic/hiv/objectives. Accessed 17 July 2020.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Russ, S., Zhang, C. & Liu, Y. Pre-Exposure Prophylaxis Care Continuum, Barriers, and Facilitators among Black Men Who Have Sex with Men in the United States: A Systematic Review and Meta-Analysis. AIDS Behav 25, 2278–2288 (2021). https://doi.org/10.1007/s10461-020-03156-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-03156-x