Abstract
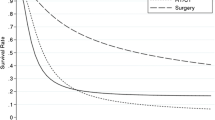
Published data on survival of T2 gallbladder carcinoma (GBC) from different countries show a wide range of 5-year survival rates from 30–> 70%. Recently, studies have demonstrated substantial variation between countries in terms of their approach to sampling gallbladders, and furthermore, that pathologists from different continents apply highly variable criteria in determining stage of invasion in this organ. These findings raised the question of whether these variations in pathologic evaluation could account for the vastly different survival rates of T2 GBC reported in the literature. In this study, survival of 316 GBCs from three countries (Chile n = 137, South Korea n = 105, USA n = 74), all adequately sampled (with a minimum of five tumor sections examined) and histopathologically verified as pT2 (after consensus examination by expert pathologists from three continents), was analyzed. Chilean patients had a significantly worse prognosis based on 5-year all-cause mortality (HR: 1.89, 95% CI: 1.27–2.83, p = 0.002) and disease-specific mortality (HR: 2.41, 95% CI: 1.51–3.84, p < 0.001), compared to their South Korean counterparts, even when controlled for age and sex. Comparing the USA to South Korea, the survival differences in all-cause mortality (HR: 1.75, 95% CI: 1.12–2.75, p = 0.015) and disease-specific mortality (HR: 1.94, 95% CI: 1.14–3.31, p = 0.015) were also pronounced. The 3-year disease-specific survival rates in South Korea, the USA, and Chile were 75%, 65%, and 55%, respectively, the 5-year disease-specific survival rates were 60%, 50%, and 50%, respectively, and the overall 5-year survival rates were 55%, 45%, and 35%, respectively. In conclusion, the survival of true T2 GBC in properly classified cases is neither as good nor as bad as previously documented in the literature and shows notable geographic differences even in well-sampled cases with consensus histopathologic criteria. Future studies should focus on other potential reasons including biologic, etiopathogenetic, management-related, populational, or healthcare practice-related factors that may influence the survival differences of T2 GBC in different regions.



Similar content being viewed by others
References
Misra S, Chaturvedi A, Misra NC, Sharma ID (2003) Carcinoma of the gallbladder. Lancet Oncol 4:167–176
Randi G, Franceschi S, La Vecchia C (2006) Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer 118:1591–1602. https://doi.org/10.1002/ijc.21683
Lazcano-Ponce EC, Miquel JF, Munoz N, Herrero R, Ferrecio C, Wistuba II, Alonso de Ruiz P, Aristi Urista G, Nervi F (2001) Epidemiology and molecular pathology of gallbladder cancer. CA Cancer J Clin 51:349–364
Pandey M (2003) Risk factors for gallbladder cancer: a reappraisal. Eur J Cancer Prev 12:15–24. https://doi.org/10.1097/01.cej.0000043740.13672.7c
Randi G, Malvezzi M, Levi F, Ferlay J, Negri E, Franceschi S, La Vecchia C (2009) Epidemiology of biliary tract cancers: an update. Ann Oncol 20:146–159. https://doi.org/10.1093/annonc/mdn533
Kanthan R, Senger JL, Ahmed S, Kanthan SC (2015) Gallbladder cancer in the 21st century. J Oncol 2015:967472. https://doi.org/10.1155/2015/967472
Wistuba II, Gazdar AF (2004) Gallbladder cancer: lessons from a rare tumour. Nat Rev Cancer 4:695–706. https://doi.org/10.1038/nrc1429
Miller G, Jarnagin WR (2008) Gallbladder carcinoma. Eur J Surg Oncol 34:306–312. https://doi.org/10.1016/j.ejso.2007.07.206
Miranda-Filho A, Pineros M, Ferreccio C, Adsay V, Soerjomataram I, Bray F, Koshiol J (2020) Gallbladder and extrahepatic bile duct cancers in the Americas: incidence and mortality patterns and trends. Int J Cancer 147:978–989. https://doi.org/10.1002/ijc.32863
Olivares LV (2016) Cancer of the gallbladder-Chilean statistics. Ecancermedicalscience 10:704. https://doi.org/10.3332/ecancer.2016.704
Bertran E, Heise K, Andia ME, Ferreccio C (2010) Gallbladder cancer: incidence and survival in a high-risk area of Chile. Int J Cancer 127:2446–2454. https://doi.org/10.1002/ijc.25421
Butte JM, Matsuo K, Gonen M, D’Angelica MI, Waugh E, Allen PJ, Fong Y, DeMatteo RP, Blumgart L, Endo I, De La Fuente H, Jarnagin WR (2011) Gallbladder cancer: differences in presentation, surgical treatment, and survival in patients treated at centers in three countries. J Am Coll Surg 212:50–61. https://doi.org/10.1016/j.jamcollsurg.2010.09.009
Kayahara M, Nagakawa T (2007) Recent trends of gallbladder cancer in Japan: an analysis of 4,770 patients. Cancer 110:572–580. https://doi.org/10.1002/cncr.22815
Bartlett DL, Fong Y, Fortner JG, Brennan MF, Blumgart LH (1996) Long-term results after resection for gallbladder cancer. Implications for staging and management. Ann Surg 224:639–646
Benoist S, Panis Y, Fagniez PL (1998) Long-term results after curative resection for carcinoma of the gallbladder. French University Association for Surgical Research. Am J Surg 175:118–122
Chijiiwa K, Nakano K, Ueda J, Noshiro H, Nagai E, Yamaguchi K, Tanaka M (2001) Surgical treatment of patients with T2 gallbladder carcinoma invading the subserosal layer. J Am Coll Surg 192:600–607
de Aretxabala XA, Roa IS, Burgos LA, Araya JC, Villaseca MA, Silva JA (1997) Curative resection in potentially resectable tumours of the gallbladder. Eur J Surg 163:419–426
Fong Y, Jarnagin W, Blumgart LH (2000) Gallbladder cancer: comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Ann Surg 232:557–569
Kim DH, Kim SH, Choi GH, Kang CM, Kim KS, Choi JS, Lee WJ (2013) Role of cholecystectomy and lymph node dissection in patients with T2 gallbladder cancer. World J Surg 37:2635–2640. https://doi.org/10.1007/s00268-013-2187-2
Mayo SC, Shore AD, Nathan H, Edil B, Wolfgang CL, Hirose K, Herman J, Schulick RD, Choti MA, Pawlik TM (2010) National trends in the management and survival of surgically managed gallbladder adenocarcinoma over 15 years: a population-based analysis. J Gastrointest Surg 14:1578–1591. https://doi.org/10.1007/s11605-010-1335-3
Miyazaki M, Itoh H, Ambiru S, Shimizu H, Togawa A, Gohchi E, Nakajima N, Suwa T (1996) Radical surgery for advanced gallbladder carcinoma. Br J Surg 83:478–481
Nevin JE, Moran TJ, Kay S, King R (1976) Carcinoma of the gallbladder: staging, treatment, and prognosis. Cancer 37:141–148
Ogura Y, Mizumoto R, Isaji S, Kusuda T, Matsuda S, Tabata M (1991) Radical operations for carcinoma of the gallbladder: present status in Japan. World J Surg 15:337–343
Shirai Y, Yoshida K, Tsukada K, Muto T (1992) Inapparent carcinoma of the gallbladder. An appraisal of a radical second operation after simple cholecystectomy. Ann Surg 215:326–331
Zhu AX, Hong TS, Hezel AF, Kooby DA (2010) Current management of gallbladder carcinoma. Oncologist 15:168–181. https://doi.org/10.1634/theoncologist.2009-0302
Adsay NV, Bagci P, Tajiri T, Oliva I, Ohike N, Balci S, Gonzalez RS, Basturk O, Jang KT, Roa JC (2012) Pathologic staging of pancreatic, ampullary, biliary, and gallbladder cancers: pitfalls and practical limitations of the current AJCC/UICC TNM staging system and opportunities for improvement. Semin Diagn Pathol 29:127–141. https://doi.org/10.1053/j.semdp.2012.08.010
de Aretxabala X, Roa I, Burgos L, Losada H, Roa JC, Mora J, Hepp J, Leon J, Maluenda F (2006) Gallbladder cancer: an analysis of a series of 139 patients with invasion restricted to the subserosal layer. J Gastrointest Surg 10:186–192. https://doi.org/10.1016/j.gassur.2005.11.003
Mazer LM, Losada HF, Chaudhry RM, Velazquez-Ramirez GA, Donohue JH, Kooby DA, Nagorney DM, Adsay NV, Sarmiento JM (2012) Tumor characteristics and survival analysis of incidental versus suspected gallbladder carcinoma. J Gastrointest Surg 16:1311–1317. https://doi.org/10.1007/s11605-012-1901-y
Tsukada K, Kurosaki I, Uchida K, Shirai Y, Oohashi Y, Yokoyama N, Watanabe H, Hatakeyama K (1997) Lymph node spread from carcinoma of the gallbladder. Cancer 80:661–667
Wanebo HJ, Castle WN, Fechner RE (1982) Is carcinoma of the gallbladder a curable lesion? Ann Surg 195:624–631
Wright BE, Lee CC, Iddings DM, Kavanagh M, Bilchik AJ (2007) Management of T2 gallbladder cancer: are practice patterns consistent with national recommendations? Am J Surg 194:820–825; discussion 825-826. https://doi.org/10.1016/j.amjsurg.2007.08.032
Yokomizo H, Yamane T, Hirata T, Hifumi M, Kawaguchi T, Fukuda S (2007) Surgical treatment of pT2 gallbladder carcinoma: a reevaluation of the therapeutic effect of hepatectomy and extrahepatic bile duct resection based on the long-term outcome. Ann Surg Oncol 14:1366–1373. https://doi.org/10.1245/s10434-006-9219-1
Yoon YS, Han HS, Cho JY, Choi Y, Lee W, Jang JY, Choi H (2015) Is laparoscopy contraindicated for gallbladder cancer? A 10-year prospective cohort study. J Am Coll Surg 221:847–853. https://doi.org/10.1016/j.jamcollsurg.2015.07.010
Koshiol J, Bellolio E, Vivallo C, Cook P, Roa JC, McGee EE, Losada H, Van Dyke AL, Van De Wyngard V, Prado R, Villaseca M, Riquelme P, Acevedo J, Olivo V, Pettit K, Hildesheim A, Medina K, Memis B, Adsay V, Ferreccio C, Araya JC (2018) Distribution of dysplasia and cancer in the gallbladder: an analysis from a high cancer-risk population. Hum Pathol 82:87–94. https://doi.org/10.1016/j.humpath.2018.07.015
Tayeb M, Rauf F, Ahmad K, Khan FM (2015) Is it necessary to submit grossly normal looking gall bladder specimens for histopathological examination? Asian Pac J Cancer Prev 16:1535–1538. https://doi.org/10.7314/apjcp.2015.16.4.1535
Emmett CD, Barrett P, Gilliam AD, Mitchell AI (2015) Routine versus selective histological examination after cholecystectomy to exclude incidental gallbladder carcinoma. Ann R Coll Surg Engl 97:526–529. https://doi.org/10.1308/rcsann.2015.0013
Renshaw AA, Gould EW (2012) Submitting the entire gallbladder in cases of dysplasia is not justified. Am J Clin Pathol 138:374–376. https://doi.org/10.1309/ajcpb0ztxxif6mof
Darmas B, Mahmud S, Abbas A, Baker AL (2007) Is there any justification for the routine histological examination of straightforward cholecystectomy specimens? Ann R Coll Surg Engl 89:238–241. https://doi.org/10.1308/003588407x168361
Elshaer M, Gravante G, Yang Y, Hudson S, Thomas K, Sorge R, Al-Hamali S, Kelkar A, Ebdewi H (2014) Routine versus selective histologic analysis of gallbladder specimens for the detection of incidental gallbladder cancers. A retrospective review over 9 years of activity with a special focus on patients’ age. Am J Surg 208:444–449. https://doi.org/10.1016/j.amjsurg.2013.12.038
Olthof PB, Metman MJH, de Krijger RR, Scheepers JJ, Roos D, Dekker JWT (2018) Routine pathology and postoperative follow-up are not cost-effective in cholecystectomy for benign gallbladder disease. World J Surg 42:3165–3170. https://doi.org/10.1007/s00268-018-4619-5
Limaiem F, Sassi A, Talbi G, Bouraoui S, Mzabi S (2017) Routine histopathological study of cholecystectomy specimens. Useful? A retrospective study of 1960 cases. Acta Gastroenterol Belg 80:365–370
Adsay V, Saka B, Basturk O, Roa JC (2013) Criteria for pathologic sampling of gallbladder specimens. Am J Clin Pathol 140:278–280. https://doi.org/10.1309/ajcpujpgqiz6dc6a
Hayes BD, Muldoon C (2014) Seek and ye shall find: the importance of careful macroscopic examination and thorough sampling in 2522 cholecystectomy specimens. Ann Diagn Pathol 18:181–186. https://doi.org/10.1016/j.anndiagpath.2014.03.004
Vega EA, Vinuela E, Okuno M, Joechle K, Sanhueza M, Diaz C, Jarufe N, Martinez J, Troncoso A, Diaz A, Chun YS, Tzeng CD, Lee JE, Vauthey JN, Conrad C (2019) Incidental versus non-incidental gallbladder cancer: index cholecystectomy before oncologic re-resection negatively impacts survival in T2b tumors. HPB (Oxford) 21:1046–1056. https://doi.org/10.1016/j.hpb.2018.12.006
Pawlik TM, Gleisner AL, Vigano L, Kooby DA, Bauer TW, Frilling A, Adams RB, Staley CA, Trindade EN, Schulick RD, Choti MA, Capussotti L (2007) Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. J Gastrointest Surg 11:1478–1486; discussion 1486-1477. https://doi.org/10.1007/s11605-007-0309-6
Fuks D, Regimbeau JM, Le Treut YP, Bachellier P, Raventos A, Pruvot FR, Chiche L, Farges O (2011) Incidental gallbladder cancer by the AFC-GBC-2009 Study Group. World J Surg 35:1887–1897. https://doi.org/10.1007/s00268-011-1134-3
Roa JC, Tapia O, Manterola C, Villaseca M, Guzman P, Araya JC, Bagci P, Saka B, Adsay V (2013) Early gallbladder carcinoma has a favorable outcome but Rokitansky-Aschoff sinus involvement is an adverse prognostic factor. Virchows Arch 463:651–661. https://doi.org/10.1007/s00428-013-1478-1
Adsay NV (2015) Gallbladder, extrahepatic biliary tree, and ampulla. In: Mills SE, Greenson JK et al (eds) Sternberg’s diagnostic surgical pathology, 6th edn. Wolters Kluwer Health, pp 1770–1846
Adsay V, Klimstra D (2015) Tumors of the gallbladder and extrahepatic bile ducts. In: Odze RD, Goldblum JR (eds) Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas, 3rd edn. Elsevier Saunders, Philadelphia
Adsay V, Roa JC, Basturk O, Torres J, Mucientes F, Del Pozo M, Villaseca M, Aguayo G, Bellolio ER, Araya JC, Endo I, Lee KB, Jang KT, Jang JY, Ohike N, Schimizu M, Hirabayashi K, Terris B, Zamboni G, Reid MD, Xue Y, Bedolla G, Quigley BC, Krasinskas A, Akkas G, Memis B, Klimstra D, Hruban R, Zhu B, Van Dyke AL, Koshiol J (2016) Epithelial atypia in the gallbladder: diagnosis and classification in an international consensus study (Abstract). Mod Pathol 29:438
Roa JC, Basturk O, Torres J, Mucientes F, Del Pozo M, Villaseca M, Aguayo G, Bellolio E, Araya JC, Endo I, Jang KT, Lee KB, Jang JY, Ohike N, Schimizu M, Hirabayashi K, Terris B, Zamboni G, Reid MD, Xue Y, Bedolla G, Quigley B, Krasinskas A, Akkas G, Memis B, Klimstra D, Hruban R, Zhu B, Van Dyke AL, Koshiol J, Adsay NV (2016) Marked geographic differences in the pathologic diagnosis of non-invasive (Tis) vs minimally invasive (T1) gallbladder cancer: santiago conference highlights the need for the unifying category “early gallbladder cancer” (EGBC) (Abstract). Mod Pathol 29:447
Vieth M, Riddell RH, Montgomery EA (2014) High-grade dysplasia versus carcinoma: east is east and west is west, but does it need to be that way? Am J Surg Pathol 38:1453–1456. https://doi.org/10.1097/pas.0000000000000288
Lauwers GY, Shimizu M, Correa P, Riddell RH, Kato Y, Lewin KJ, Yamabe H, Sheahan DG, Lewin D, Sipponen P, Kubilis PS, Watanabe H (1999) Evaluation of gastric biopsies for neoplasia: differences between Japanese and Western pathologists. Am J Surg Pathol 23:511–518. https://doi.org/10.1097/00000478-199905000-00003
https://seer.cancer.gov/statistics/ Accessed on March 20th 2020
Lau CSM, Zywot A, Mahendraraj K, Chamberlain RS (2017) Gallbladder carcinoma in the United States: a population based clinical outcomes study involving 22,343 patients from the Surveillance, Epidemiology, and End Result Database (1973-2013). HPB Surg 2017:1532835. https://doi.org/10.1155/2017/1532835
Kayahara M, Nagakawa T, Nakagawara H, Kitagawa H, Ohta T (2008) Prognostic factors for gallbladder cancer in Japan. Ann Surg 248:807–814. https://doi.org/10.1097/SLA.0b013e31818a1561
Hariharan D, Saied A, Kocher HM (2008) Analysis of mortality rates for gallbladder cancer across the world. HPB (Oxford) 10:327–331. https://doi.org/10.1080/13651820802007464
Duffy A, Capanu M, Abou-Alfa GK, Huitzil D, Jarnagin W, Fong Y, D’Angelica M, Dematteo RP, Blumgart LH, O’Reilly EM (2008) Gallbladder cancer (GBC): 10-year experience at Memorial Sloan-Kettering Cancer Centre (MSKCC). J Surg Oncol 98:485–489. https://doi.org/10.1002/jso.21141
Konstantinidis IT, Deshpande V, Genevay M, Berger D, Fernandez-del Castillo C, Tanabe KK, Zheng H, Lauwers GY, Ferrone CR (2009) Trends in presentation and survival for gallbladder cancer during a period of more than 4 decades: a single-institution experience. Arch Surg 144:441–447; discussion 447. https://doi.org/10.1001/archsurg.2009.46
Lai CH, Lau WY (2008) Gallbladder cancer--a comprehensive review. Surgeon 6:101–110
Narayan RR, Creasy JM, Goldman DA, Gönen M, Kandoth C, Kundra R, Solit DB, Askan G, Klimstra DS, Basturk O, Allen PJ, Balachandran VP, D’Angelica MI, DeMatteo RP, Drebin JA, Kingham TP, Simpson AL, Abou-Alfa GK, Harding JJ, O’Reilly EM, Butte JM, Matsuyama R, Endo I, Jarnagin WR (2019) Regional differences in gallbladder cancer pathogenesis: insights from a multi-institutional comparison of tumor mutations. Cancer 125:575–585. https://doi.org/10.1002/cncr.31850
Yang P, Javle M, Pang F, Zhao W, Abdel-Wahab R, Chen X, Meric-Bernstam F, Chen H, Borad MJ, Liu Y, Zou C, Mu S, Xing Y, Wang K, Peng C, Che X (2019) Somatic genetic aberrations in gallbladder cancer: comparison between Chinese and US patients. Hepatobiliary Surg Nutr 8:604–614. https://doi.org/10.21037/hbsn.2019.04.11
Akita M, Fujikura K, Ajiki T, Fukumoto T, Otani K, Hirose T, Tominaga M, Itoh T, Zen Y (2019) Intracholecystic papillary neoplasms are distinct from papillary gallbladder cancers: a clinicopathologic and exome-sequencing study. Am J Surg Pathol 43:783–791. https://doi.org/10.1097/pas.0000000000001237
Chang J, Jang JY, Kang MJ, Jung W, Shin YC, Kim SW (2016) Clinicopathologic differences in patients with gallbladder cancer according to the presence of anomalous biliopancreatic junction. World J Surg 40:1211–1217. https://doi.org/10.1007/s00268-015-3359-z
Kamisawa T, Ando H, Hamada Y, Fujii H, Koshinaga T, Urushihara N, Itoi T, Shimada H (2014) Diagnostic criteria for pancreaticobiliary maljunction 2013. J Hepatobiliary Pancreat Sci 21:159–161. https://doi.org/10.1002/jhbp.57
Kamisawa T, Ando H, Suyama M, Shimada M, Morine Y, Shimada H (2012) Japanese clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol 47:731–759. https://doi.org/10.1007/s00535-012-0611-2
Muraki T, Memis B, Reid MD, Uehara T, Ito T, Hasebe O, Okaniwa S, Horigome N, Hisa T, Mittal P, Freedman A, Maithel S, Sarmiento JM, Krasinskas A, Koshiol J, Adsay V (2017) Reflux-associated cholecystopathy: analysis of 76 gallbladders from patients with supra-Oddi union of the pancreatic duct and common bile duct (pancreatobiliary maljunction) elucidates a specific diagnostic pattern of mucosal hyperplasia as a prelude to carcinoma. Am J Surg Pathol 41:1167–1177. https://doi.org/10.1097/pas.0000000000000882
Sugiyama Y, Kobori H, Hakamada K, Seito D, Sasaki M (2000) Altered bile composition in the gallbladder and common bile duct of patients with anomalous pancreaticobiliary ductal junction. World J Surg 24:17–20; discussion 21. https://doi.org/10.1007/s002689910004
Rogler G (2014) Chronic ulcerative colitis and colorectal cancer. Cancer Lett 345:235–241. https://doi.org/10.1016/j.canlet.2013.07.032
Author information
Authors and Affiliations
Contributions
All authors agreed with the content and gave explicit consent to submit this work. All authors made substantial contributions to the conception, design, case acquisition, analysis, and interpretation of data, and assisted with drafting and revising the work, approving the version to be published. The authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study involved 3 continents and investigators from 5 countries and entailed the collection and detailed re-review of clinical and pathology findings in hundreds of gallbladder cancer patients, with multiple consensus meetings held in Santiago, Chile; Atlanta, USA; and Seoul, Korea. Each investigator contributed significantly in multiple ways as outlined below:
NVA, JK, JCR, MDR, OB, and JYJ conceived the study and designed the approach and analytic methods along with MSDS and MG. Case procurement for study, case organization, and collection of clinical information including survival data were performed by JMS and SKM from the USA, HFL and JCA from Chile, and JYJ, KTJ, and SHM from Korea. Initial histopathologic review in different continents was conducted by SMH, KL, HK, HJC, and KTJ (Korean cases), NVA, BP, BM, MDR, and OB (for cases from the USA), and JCA, JCR, and EB (for Chilean cases). The international pathology consensus meetings were organized and coordinated by JCR (in Santiago, Chile), JCA (in Temuco, Chile), JYJ and KTJ (in Seoul, Korea), and NVA and JK (in Atlanta, USA), and the working group that conducted the re-review of the pathology material included JYJ, SKL, HK, HJC, SMH, and KTJ, from Korea, NVA, OB, MDR, JK, from the USA, and JCR, JCA, EB, and HL from Chile. TM, BP, and BM performed the organization of the combined international data. MSD, BP, BM, MDR, TM, OB, JK, and NVA conducted the literature analysis and organization of the manuscript. Statistical analysis was performed by MG, MSDS, JK, and SB. MSDS, MG, OB, MDR, JK, and NVA prepared the manuscript draft. All authors of this paper have critically reviewed the intellectual content and approved the final version submitted.
Corresponding author
Ethics declarations
The study was conducted in accordance with the Institutional Review Board requirements.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
The manuscript has not been submitted to more than one journal for simultaneous consideration. The submitted work is original and has not been published elsewhere in any form. This study has not been split up into several parts to increase the quantity of submissions. Results presented herein have been done so without fabrication, falsification, or inappropriate data manipulation. Others’ work has been properly acknowledged in the references.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
DeSimone, M.S., Goodman, M., Pehlivanoglu, B. et al. T2 gallbladder cancer shows substantial survival variation between continents and this is not due to histopathologic criteria or pathologic sampling differences. Virchows Arch 478, 875–884 (2021). https://doi.org/10.1007/s00428-020-02968-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-020-02968-5