Abstract
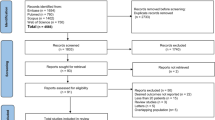
Intracranial aneurysms (IA) occur in 3–5% of the general population and may require surgical or endovascular obliteration if the patient is symptomatic or has an increased risk of rupture. These procedures carry an inherent risk of neurological complications, and the outcome can be influenced by the physiological and pharmacological effects of the administered anesthetics. Despite the critical role of anesthetic agents, however, there are no current studies to systematically assess the intraoperative anesthetic risks, benefits, and outcome effects in this population. In this systematic review of the literature, we carefully examine the existing evidence on the risks and benefits of common anesthetic agents during IA obliteration, their physiological and clinical characteristics, and effects on neurological outcome. The initial search strategy captured a total of 287 published studies. Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, 28 studies were included in the final report. Our data showed that both volatile and intravenous anesthetics are commonly employed, without evidence that either is superior. Although no specific anesthetic regimens are promoted, their unique neurological, cardiovascular, and physiological properties may be critical to the outcome in vulnerable patients. In particular, patients at risk for perioperative ischemia may benefit from timely administration of anesthetic agents with neuroprotective properties and optimization of their physiological parameters. Further studies are warranted to examine if these anesthetic regimens can reduce the risk of neurological injury and improve the overall outcome in these patients.



Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Bruder N, Boussen S, Velly L (2019) Anesthesia for aneurysmal subarachnoid hemorrhage. In: Prabhakar H, Ali Z. (eds) Textbook of neuroanesthesia and neurocritical care. Singapore: Springer Nature Singapore Pte Ltd, pp 115–130
Lecours M, Gelb AW (2015) Anesthesia for the surgical treatment of cerebral aneurysms. Rev Colom Anestesiol 43:45–51
Abd-Elsayed AA, Wehby AS, Farag E (2014) Anesthetic management of patients with intracranial aneurysms. Ochsner J 14(3):418–425
Malinova V, Schatlo B, Voit M, Suntheim P, Rohde V, Mielke D (2017) The impact of temporary clipping during aneurysm surgery on the incidence of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. J Neurosurg 129(1):84–90
Desai VR, Rosas AL, Britz GW (2017) Adenosine to facilitate the clipping of cerebral aneurysms: literature review. Stroke Vasc Neurol 2(4):204–209
Inhalational anesthetics. In: Butterworth JF, IV, Mackey DC, Wasnick JD. (eds) Morgan & Mikhail’s clinical anesthesiology, 5e. McGraw-Hill. https://accessmedicine.mhmedical.com/Book.aspx?bookid=2444. Accessed 22 Nov 2020
Drummond John C, Dao Andrew V, Roth David M, Cheng C-R, Atwater BI, Minokadeh A, Pasco LC, Patel PM (2008) Effect of dexmedetomidine on cerebral blood flow velocity, cerebral metabolic rate, and carbon dioxide response in normal humans. Anesthesiology 108(2):225–232. https://doi.org/10.1097/01.anes.0000299576.00302.4c
Chowdhury T, Petropolis A, Wilkinson M, Schaller B, Sandu N, Cappellani RB (2014) Controversies in the anesthetic management of intraoperative rupture of intracranial aneurysm. Anesthesiol Res Pract 2014:1–10
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14:579–579. https://doi.org/10.1186/s12913-014-0579-0
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, Atkins D, Barbour V, Barrowman N, Berlin JA (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Chinese edition). J Chin Integrat Med 7(9):889–896
McGregor DG, William L, Pasternak J, Rusy D, Hogan K, Samra S, Hindman B, Todd MM, Schroeder DR, Bayman EO, Clarke W, Torner J, Weeks J (2008) Effect of nitrous oxide on neurologic and neuropsychological function after intracranial aneurysm surgery. Anesthesiology 108(4):568–579. https://doi.org/10.1097/ALN.0b013e31816721fa
Pasternak JJ, McGregor DG, Lanier WL, Schroeder DR, Rusy DA, Hindman B, Clarke W, Torner J, Todd MM (2009) Effect of nitrous oxide use on long-term neurologic and neuropsychological outcome in patients who received temporary proximal artery occlusion during cerebral aneurysm clipping surgery. Anesthesiology 110(3):563–573
Madsen JB, Cold GE, Hansen ES, Bardrum B, Kruse-Larsen C (1987) Cerebral blood flow and metabolism during isoflurane-induced hypotension in patients subjected to surgery for cerebral aneurysms. Br J Anaesth 59(10):1204–1207. https://doi.org/10.1093/bja/59.10.1204
Roth S, Jones SC, Ebrahim ZY, Friel H, Little JR (1989) Local cortical blood flow and oxygen consumption during isoflurane-induced hypotension. Results in patients undergoing intracranial aneurysm clipping. Cleve Clin J Med 56(8):766–770. https://doi.org/10.3949/ccjm.56.8.766
Meyer FB, Muzzi DA (1992) Cerebral protection during aneurysm surgery with isoflurane anesthesia. J Neurosurg 76(3):541–543
Wang T, Luo F, Shan R, Zhen Y, Zhao J, Zhang S (2004) Changes of endothelin and calcitonin gene-related peptide during desflurane anesthesia in patients undergoing intracranial aneurysm clipping. J Neurosurg Anesthesiol 16(3):236–239. https://doi.org/10.1097/00008506-200407000-00009
Mayberg TS, Lam AM, Matta BF, Domino KB, Winn HR (1995) Ketamine does not increase cerebral blood flow velocity or intracranial pressure during isoflurane/nitrous oxide anesthesia in patients undergoing craniotomy. Anesth Analg 81(1):84–89. https://doi.org/10.1097/00000539-199507000-00017
Von der Brelie C, Seifert M, Rot S, Tittel A, Sanft C, Meier U, Lemcke J (2017) Sedation of patients with acute aneurysmal subarachnoid hemorrhage with ketamine is safe and might influence the occurrence of cerebral infarctions associated with delayed cerebral ischemia. World Neurosurg 97:374–382. https://doi.org/10.1016/j.wneu.2016.09.121
Souza KM, Anzoategui LC, Pedroso WC, Gemperli WA (2005) Dexmedetomidine in general anesthesia for surgical treatment of cerebral aneurysm in pregnant patient with specific hypertensive disease of pregnancy: case report. Rev Bras Anestesiol 55(2):212–216. https://doi.org/10.1590/s0034-70942005000200008
Yokota H, Yokoyama K, Noguchi H, Nishioka T, Umegaki O, Komatsu H, Sakaki T (2011) Post-operative dexmedetomidine-based sedation after uneventful intracranial surgery for unruptured cerebral aneurysm: comparison with propofol-based sedation. Neurocrit Care 14(2):182–187. https://doi.org/10.1007/s12028-010-9485-4
Lee HH, Jung YJ, Choi BY, Chang CH (2014) Usefulness of dexmedetomidine during intracerebral aneurysm coiling. J Korean Neurosurg Soc 55(4):185–189. https://doi.org/10.3340/jkns.2014.55.4.185
Tang CL, Li J, Zhang ZT, Zhao B, Wang SD, Zhang HM, Shi S, Zhang Y, Xia ZY (2018) Neuroprotective effect of bispectral index-guided fast-track anesthesia using sevoflurane combined with dexmedetomidine for intracranial aneurysm embolization. Neural Regen Res 13(2):280–288. https://doi.org/10.4103/1673-5374.226399
McDermott MW, Durity FA, Borozny M, Mountain MA (1989) Temporary vessel occlusion and barbiturate protection in cerebral aneurysm surgery. Neurosurgery 25(1):54–61; discussion 61-52. https://doi.org/10.1097/00006123-198907000-00010
McConkey PP, Kien ND (2002) Cerebral protection with thiopentone during combined carotid endarterectomy and clipping of intracranial aneurysm. Anaesth Intensive Care 30(2):219–222. https://doi.org/10.1177/0310057x0203000217
Ravussin P, de Tribolet N (1993) Total intravenous anesthesia with propofol for burst suppression in cerebral aneurysm surgery: preliminary report of 42 patients. Neurosurgery 32(2):236–240 discussion 240. https://doi.org/10.1227/00006123-199302000-00013
Schmieder K, Schregel W, Engelhardt M, Harders A, Cunitz G (2003) Cerebral vascular reactivity response to anaesthetic induction with propofol in patients with intracranial space-occupying lesions and vascular malformations. Eur J Anaesthesiol 20(6):457–460. https://doi.org/10.1017/s0265021503000711
Yamada M, Nishikawa K, Kawahara F, Yoshikawa D, Saito S, Goto F (2003) Anesthetic management for clipping a giant basilar artery aneurysm with moderate hypothermia, extracorporeal circulation assistance, and propofol infusion. J Neurosurg Anesthesiol 15(3):274–277. https://doi.org/10.1097/00008506-200307000-00018
Mahajan C, Chouhan RS, Rath GP, Dash HH, Suri A, Chandra PS, Mahajan A (2014) Effect of intraoperative brain protection with propofol on postoperative cognition in patients undergoing temporary clipping during intracranial aneurysm surgery. Neurol India 62(3):262–268. https://doi.org/10.4103/0028-3886.136908
Karwacki Z, Niewiadomski S, Witkowska M, Dzierzanowski J, Szczyrba S, Cichomska M (2018) The influence of propofol on middle cerebral artery flow velocity (VMCA) in patients with unruptured intracranial aneurysms during induction of general anaesthesia. Anaesthesiol Intensive Ther 50(5):349–358. https://doi.org/10.5603/ait.2018.0047
Ishibashi T, Toyama S, Miki K, Karakama J, Yoshino Y, Ishibashi S, Tomita M, Nemoto S (2019) Effects of propofol versus sevoflurane on cerebral circulation time in patients undergoing coiling for cerebral artery aneurysm: a prospective randomized crossover study. J Clin Monit Comput 33(6):987–998. https://doi.org/10.1007/s10877-018-00251-2
Guo D, Li Y, Wang H, Wang X, Hua W, Tang Q, Miao L, Wang G (2019) Propofol post-conditioning after temporary clipping reverses oxidative stress in aneurysm surgery. Int J Neurosci 129(2):155–164. https://doi.org/10.1080/00207454.2018.1483920
Uchida K, Yasunaga H, Sumitani M, Horiguchi H, Fushimi K, Yamada Y (2014) Effects of remifentanil on in-hospital mortality and length of stay following clipping of intracranial aneurysm: a propensity score-matched analysis. J Neurosurg Anesthesiol 26(4):291–298. https://doi.org/10.1097/ana.0000000000000039
Lavine SD, Masri LS, Levy ML, Giannotta SL (1997) Temporary occlusion of the middle cerebral artery in intracranial aneurysm surgery: time limitation and advantage of brain protection. Neurosurg Focus 2(6):e4. https://doi.org/10.3171/foc.1997.2.1.5
Foroohar M, Macdonald RL, Roth S, Stoodley M, Weir B (2000) Intraoperative variables and early outcome after aneurysm surgery. Surg Neurol 54(4):304–315. https://doi.org/10.1016/s0090-3019(00)00294-9
Allen G, Farling P, McAtamney D (2006) Anesthetic management of the pregnant patient for endovascular coiling of an unruptured intracranial aneurysm. Neurocrit Care 4(1):18–20. https://doi.org/10.1385/ncc:4:1:018
Magni G, La Rosa I, Gimignani S, Melillo G, Imperiale C, Rosa G (2007) Early postoperative complications after intracranial surgery: comparison between total intravenous and balanced anesthesia. J Neurosurg Anesthesiol 19(4):229–234. https://doi.org/10.1097/ANA.0b013e31806e5f5a
Karwacki Z, Witkowska M, Niewiadomski S, Wiatr A, Bukowski P, Wierzchowska J, Zapasnik A (2013) Anaesthetic management for endovascular treatment of unruptured intracranial aneurysms. Anaesthesiol Intensive Ther 45(3):145–148. https://doi.org/10.5603/ait.2013.0030
Hoffman WE, Charbel FT, Edelman G, Ausman JI (1998) Thiopental and desflurane treatment for brain protection. Neurosurgery 43(5):1050–1053. https://doi.org/10.1097/00006123-199811000-00026
Courville CB (1939) Untoward effects of nitrous oxide anesthesia with particular reference to residual neurologic and psychiatric manifestations. California: Pacific Press Publishing Association, p 174
Lam AM, Mayberg TS (1992) Use of nitrous oxide in neuroanesthesia: why bother? J Neurosurg Anesthesiol 4:284–284
Haelewyn B, David HN, Rouillon C, Chazalviel L, Lecocq M, Risso J-J, Lemaire M, Abraini JH (2008) Neuroprotection by nitrous oxide: facts and evidence. Crit Care Med 36(9):2651–2659
Culley DJ, Crosby G (2008) Nitrous oxide in neuroanesthesia: tried and true or toxin? Anesthesiology 108(4):553–554
Pasternak JJ, Lanier WL (2010) Is nitrous oxide use appropriate in neurosurgical and neurologically at-risk patients? Curr Opin Anaesthesiol 23(5):544–550. https://doi.org/10.1097/ACO.0b013e32833e1520
Varma MK, Price K, Jayakrishnan V, Manickam B, Kessell G (2007) Anaesthetic considerations for interventional neuroradiology. Br J Anaesth 99(1):75–85. https://doi.org/10.1093/bja/aem122
Frost EA (2017) Nitrous oxide in neuroanesthesia: does it have a place? In: Scher CS, Clebone A, Miller SM, Roccaforte JD, Capan LM (eds) You’re wrong, I’m right: dueling authors reexamine classic teachings in anesthesia. Cham: Springer International Publishing, pp 207–208
Frawley G, Davidson A (2016) Inhaled anestheteic agents. In: Davis PJ, Cladis FP (eds) Smith’s anesthesia for infants and children. Philadelphia: Elsevier Health Sciences, pp 200–213
Lee JJ, Li L, Jung H-H, Zuo Z (2008) Postconditioning with isoflurane reduced ischemia-induced brain injury in rats. Anesthesiology 108(6):1055–1062
Lam AM, Gelb AW (1983) Cardiovascular effects of isoflurane-induced hypotension for cerebral aneurysm surgery. Anesth Analg 62(8):742–748
MADSEN JB, COLD GE, HANSEN ES, BARDRUM B, KRUSE-LARSEN C (1987) Cerebral blood flow and metabolism during isoflurane-induced hypotension in patients subjected to surgery for cerebral aneurysms. BJA 59(10):1204–1207. https://doi.org/10.1093/bja/59.10.1204
Gaidhani N, Sun F, Schreihofer D, Uteshev VV (2017) Duration of isoflurane-based surgical anesthesia determines severity of brain injury and neurological deficits after a transient focal ischemia in young adult rats. Brain Res Bull 134:168–176. https://doi.org/10.1016/j.brainresbull.2017.07.018
Lehmann F, Müller M, Zimmermann J, Güresir Á, Lehmann V, Putensen C, Vatter H, Güresir E (2020) Inhalational isoflurane sedation in patients with decompressive craniectomy suffering from severe subarachnoid hemorrhage: a case series. J Neuroanaesthesiol Crit Care 7:27–33
Cottrell JE, Patel P (2017) Cottrell and Patel's neuroanesthesia, Sixth edn. Elsevier, Edinburgh
Brioni JD, Varughese S, Ahmed R, Bein B (2017) A clinical review of inhalation anesthesia with sevoflurane: from early research to emerging topics. J Anesth 31(5):764–778. https://doi.org/10.1007/s00540-017-2375-6
Schifilliti D, Grasso G, Conti A, Fodale V (2010) Anaesthetic-related neuroprotection: intravenous or inhalational agents? CNS Drugs 24(11):893–907. https://doi.org/10.2165/11584760-000000000-00000
Xu L, Shen J, Yu L, Sun J, McQuillan PM, Hu Z, Yan M (2018) Role of autophagy in sevoflurane-induced neurotoxicity in neonatal rat hippocampal cells. Brain Res Bull 140:291–298. https://doi.org/10.1016/j.brainresbull.2018.05.020
Bo LJ, Yu PX, Zhang FZ, Dong ZM (2018) Dexmedetomidine mitigates sevoflurane-induced cell cycle arrest in hippocampus. J Anesth 32(5):717–724. https://doi.org/10.1007/s00540-018-2545-1
Eger EI 2nd, Gong D, Koblin DD, Bowland T, Ionescu P, Laster MJ, Weiskopf RB (1998) The effect of anesthetic duration on kinetic and recovery characteristics of desflurane versus sevoflurane, and on the kinetic characteristics of compound A, in volunteers. Anesth Analg 86(2):414–421. https://doi.org/10.1097/00000539-199802000-00037
Holmstrom A, Akeson J (2004) Desflurane increases intracranial pressure more and sevoflurane less than isoflurane in pigs subjected to intracranial hypertension. J Neurosurg Anesthesiol 16(2):136–143. https://doi.org/10.1097/00008506-200404000-00005
Sponheim S, Skraastad O, Helseth E, Due-Tonnesen B, Aamodt G, Breivik H (2003) Effects of 0.5 and 1.0 MAC isoflurane, sevoflurane and desflurane on intracranial and cerebral perfusion pressures in children. Acta Anaesthesiol Scand 47(8):932–938. https://doi.org/10.1034/j.1399-6576.2003.00199.x
Kundra S, Mahendru V, Gupta V, Choudhary AK (2014) Principles of neuroanesthesia in aneurysmal subarachnoid hemorrhage. J Anaesthesiol Clin Pharmacol 30(3):328–337. https://doi.org/10.4103/0970-9185.137261
Lee JW, Woo JH, Baik HJ, Kim DY, Chae JS, Yang NR, Seo EK (2018) The effect of anesthetic agents on cerebral vasospasms after subarachnoid hemorrhage: a retrospective study. Medicine (Baltimore) 97(31):e11666. https://doi.org/10.1097/MD.0000000000011666
Srivastava S (2017) Use of desflurane in neurosurgery: cons. J Neuroanaesthesiol Crit Care 04. https://doi.org/10.4103/2348-0548.199955
Urwin SC, Menon DK (2004) Comparative tolerability of sedative agents in head-injured adults. Drug Saf 27(2):107–133. https://doi.org/10.2165/00002018-200427020-00003
Luthra A, Rath G (2018) Ketamine: a neuroanesthesiologist's friend or foe? J Neuroanaesthesiol Crit Care 05:77–82. https://doi.org/10.1055/s-0038-1654746
Soriano FX, Papadia S, Hofmann F, Hardingham NR, Bading H, Hardingham GE (2006) Preconditioning doses of NMDA promote neuroprotection by enhancing neuronal excitability. J Neurosci 26(17):4509–4518. https://doi.org/10.1523/jneurosci.0455-06.2006
Himmelseher S, Durieux ME (2005) Revising a dogma: ketamine for patients with neurological injury? Anesth Analg 101(2):524–534, table of contents. https://doi.org/10.1213/01.Ane.0000160585.43587.5b
Prielipp RC, Wall MH, Tobin JR, Groban L, Cannon MA, Fahey FH, Gage HD, Stump DA, James RL, Bennett J, Butterworth J (2002) Dexmedetomidine-induced sedation in volunteers decreases regional and global cerebral blood flow. Anesth Analg 95(4):1052–1059, table of contents. https://doi.org/10.1097/00000539-200210000-00048
Singh S, Chouhan RS, Bindra A, Radhakrishna N (2018) Comparison of effect of dexmedetomidine and lidocaine on intracranial and systemic hemodynamic response to chest physiotherapy and tracheal suctioning in patients with severe traumatic brain injury. J Anesth 32(4):518–523. https://doi.org/10.1007/s00540-018-2505-9
Batra A, Verma R, Bhatia VK, Chandra G, Bhushan S (2017) Dexmedetomidine as an anesthetic adjuvant in intracranial surgery. Anesth Essays Res 11(2):309–313. https://doi.org/10.4103/0259-1162.194555
Iwasaki Y, Nakamura T, Hamakawa T (2010) Retrospective evaluation of dexmedetomidine for postoperative sedation in patients for cerebral aneurysm surgery. Masui 59(11):1396–1399
Shapiro H, Galindo A, Wyte S, Harris A (1973) Rapid intraoperative reduction of intracranial pressure with thiopentone. BJA 45(10):1057–1062
Smith AL, Hoff JT, Nielsen SL, Larson CP (1974) Barbiturate protection in acute focal cerebral ischemia. Stroke 5(1):1–7. https://doi.org/10.1161/01.str.5.1.1
Hoff JT, Smith AL, Hankinson HL, Nielsen SL (1975) Barbiturate protection from cerebral infarction in primates. Stroke 6(1):28–33. https://doi.org/10.1161/01.str.6.1.28
Zaidan JR, Klochany A, Martin WM, Ziegler JS, Harless DM, Andrews RB (1991) Effect of thiopental on neurologic outcome following coronary artery bypass grafting. Anesthesiology 74(3):406–411. https://doi.org/10.1097/00000542-199103000-00003
Nussmeier NA, Arlund C, Slogoff S (1986) Neuropsychiatric complications after cardiopulmonary bypass: cerebral protection by a barbiturate. Anesthesiology 64(2):165–170. https://doi.org/10.1097/00000542-198602000-00006
Belopavlovic M, Buchthal A, Beks JW (1985) Barbiturates for cerebral aneurysm surgery. A review of preliminary results. Acta Neurochir 76(3–4):73–81. https://doi.org/10.1007/bf01418464
Vuyk J, Sitsen E, Reekers M (2020) Intravenous anesthetics. In: Gropper MA, Cohen NH, Eriksson LI, Fleisher LA, Leslie K, Wiener-Kronish JP. (eds) Miller’s anesthesia, 9th edition. Philadelphia: Elsevier Health Sciences, pp 638–679
Ravussin P, Revelly JP, Chiolero R (1991) clinical use of propofol in neuroanesthesia. Agressologie 32(8-9 spec):407–411
Acquaviva R, Campisi A, Murabito P, Raciti G, Avola R, Mangiameli S, Musumeci I, Barcellona ML, Vanella A, Li Volti G (2004) Propofol attenuates peroxynitrite-mediated DNA damage and apoptosis in cultured astrocytes: an alternative protective mechanism. Anesthesiology 101(6):1363–1371. https://doi.org/10.1097/00000542-200412000-00017
Sagara Y, Hendler S, Khoh-Reiter S, Gillenwater G, Carlo D, Schubert D, Chang J (1999) Propofol hemisuccinate protects neuronal cells from oxidative injury. J Neurochem 73(6):2524–2530. https://doi.org/10.1046/j.1471-4159.1999.0732524.x
Chui J, Mariappan R, Mehta J, Manninen P, Venkatraghavan L (2014) Comparison of propofol and volatile agents for maintenance of anesthesia during elective craniotomy procedures: systematic review and meta-analysis. Can J Anesthesia 61(4):347–356
Hayward NJ, McKnight AT, Woodruff GN (1993) Neuroprotective effect of the kappa-agonist enadoline (CI-977) in rat models of focal cerebral ischaemia. Eur J Neurosci 5(7):961–967. https://doi.org/10.1111/j.1460-9568.1993.tb00947.x
Zhang J, Haddad GG, Xia Y (2000) Delta-, but not mu- and kappa-, opioid receptor activation protects neocortical neurons from glutamate-induced excitotoxic injury. Brain Res 885(2):143–153. https://doi.org/10.1016/s0006-8993(00)02906-1
He X, Sandhu HK, Yang Y, Hua F, Belser N, Kim DH, Xia Y (2013) Neuroprotection against hypoxia/ischemia: delta-opioid receptor-mediated cellular/molecular events. Cell Mol Life Sci 70(13):2291–2303. https://doi.org/10.1007/s00018-012-1167-2
Girard F, Moumdjian R, Boudreault D, Chouinard P, Bouthilier A, Ruel M (2009) The effect of sedation on intracranial pressure in patients with an intracranial space-occupying lesion: remifentanil versus propofol. Anesth Analg 109(1):194–198. https://doi.org/10.1213/ane.0b013e3181a3ea3a
Degoute CS (2007) Controlled hypotension: a guide to drug choice. Drugs 67(7):1053–1076. https://doi.org/10.2165/00003495-200767070-00007
Ihn YK, Shin SH, Baik SK, Choi IS (2018) Complications of endovascular treatment for intracranial aneurysms: management and prevention. Interv Neuroradiol 24(3):237–245. https://doi.org/10.1177/1591019918758493
Hoffman WE, Edelman G (2000) Enhancement of brain tissue oxygenation during high dose isoflurane anesthesia in the dog. J Neurosurg Anesthesiol 12(2):95–98. https://doi.org/10.1097/00008506-200004000-00004
Tsai YC, Huang SJ, Lai YY, Chang CL, Cheng JT (1994) Propofol does not reduce infarct volume in rats undergoing permanent middle cerebral artery occlusion. Acta Anaesthesiol Sin 32(2):99–104
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, Floyd J, Fornage M, Gillespie C, Isasi C (2017) Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 135(10):e146–e603
Lavine SD, Masri LS, Levy ML, Giannotta SL (1997) Temporary occlusion of the middle cerebral artery in intracranial aneurysm surgery: time limitation and advantage of brain protection. J Neurosurg 87(6):817–824. https://doi.org/10.3171/jns.1997.87.6.0817
Hadler RA, Neuman MD, FLeisher LA (2020) Risk of anesthesia. In: Gropper MA, Cohen NH, Eriksson LI, Fleisher LA, Leslie K, Wiener-Kronish JP. (eds) Miller’s anesthesia, 9th edition. Philadelphia: Elsevier Health Sciences, pp 892–917
Fukuda M, Vazquez AL, Zong X, Kim S-G (2013) Effects of the α2-adrenergic receptor agonist dexmedetomidine on neural, vascular and BOLD fMRI responses in the somatosensory cortex. Eur J Neurosci 37(1):80–95. https://doi.org/10.1111/ejn.12024
Author information
Authors and Affiliations
Contributions
SE, JV, ABB, and SG: study design, data collection, data analysis, and writing up the first draft of the manuscript. LKB, ME, CF, RP, AT, CSO, SS, and AN: study design, data review and analysis, revision, and finalization of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This hospital registry study was approved by the Institutional Review Board at the Beth Israel Deaconess Medical Center.
Informed consent
Waived.
Consent to participate
NA, review of published literature.
Consent for publication
All authors participated in the development of the manuscript and give consent for the article to be published in Neurosurgical Review.
Code availability
NA, review of published literature.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Esmaeeli, S., Valencia, J., Buhl, L.K. et al. Anesthetic management of unruptured intracranial aneurysms: a qualitative systematic review. Neurosurg Rev 44, 2477–2492 (2021). https://doi.org/10.1007/s10143-020-01441-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01441-w