Abstract
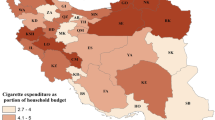
This paper aims at assessing and exploring socioeconomic inequalities in tobacco use in Kenya. Using the theory of fundamental causes, and concentration index, we investigate the determinants of tobacco use, and whether it disproportionately affects the poor. All data used in this study emanated from the 2014 Global Adult Tobacco Survey implemented in Kenya on a nationally representative sample of men and women aged 15 years and older. Our results suggest a link between tobacco use and socioeconomic inequality. Overall, poorer households are more affected by tobacco use than richer households. This socioeconomic inequality is more evident among men and households living in urban areas. The decomposition of the concentration index indicates that the overall socioeconomic inequality for current tobacco smokers is explained by 69.11% of household wealth. To reduce the prevalence rate of smoking in Kenya, policymakers could design and implement tobacco control programs through the equity lens. Community health workers could be used to promote non-smoking behaviors among the poor.




Similar content being viewed by others
References
Amos, A., Greaves, L., Nichter, M., & Bloch, M. (2011). Women and tobacco: A call for including gender in tobacco control research, policy and practice. Tobacco Control, 21(2), 1–8.
Barkan, S. E., & Rocque, M. (2018). Socioeconomic status and racism as fundamental causes of street criminality. Critical Criminology, 26(2), 211–231.
Bobak, M., Jha, P., Nguyen, S., & Jarvis, M. (2000). Poverty and smoking. Tobacco Control in Developing Countries, 1, 41–62.
Boffetta, P., & Straif, K. (2009). Use of smokeless tobacco and risk of myocardial infarction and stroke: Systematic review with meta-analysis. BMJ, 339, b3060.
Britton, J. (2017). Death, disease, and tobacco. The Lancet, 389(10082), 1861–1862.
Cambron, C., Kosterman, R., & Hawkins, J. D. (2019). Neighborhood poverty increases risk for cigarette smoking from age 30 to 39. Annals of Behavioral Medicine, 53(9), 858–864.
Chockalingam, K., Vedhachalam, C., Rangasamy, S., Sekar, G., Adinarayanan, S., Swaminathan, S., et al. (2013). Prevalence of tobacco use in urban, semi urban and rural areas in and around Chennai city, India. PLoS ONE, 8(10), 1–9.
Ciecierski, C. U., & Chaloupka, F. J. (2001). Tool 2. Tobacco data, data for economic analysis. In A. Yurekli & J. D. Beyer (Eds.), Economics of tobacco toolkit. Washington: World Bank.
Demombynes, G., & Özler, B. (2002). Crime and local inequality in South Africa. Journal of Development Economics, 76(2), 265–292.
Dong, B., Egger, P. H., & Guo, Y. (2020). Is poverty the mother of crime? Evidence from homicide rates in china. PLoS ONE, 15(5), 1–22.
Erreygers, G. (2009). Correcting the concentration index. Journal of Health Economics, 28(2), 504–515.
Fajnzylber, P., Lederman, D., & Loayza, N. (2002). Inequality and violent crime. The journal of Law and Economics, 45(1), 1–39.
Filmer, D., & Pritchett, L. H. (2001). Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of india. Demography, 38(1), 115–132.
Filmer, D., & Scott, K. (2012). Assessing asset indices. Demography, 49(1), 359–392.
Flay, B. R., Petraitis, J., & Hu, F. (1995). The theory of triadic influence: Preliminary evidence related to alcohol and tobacco use. In J. B. Fertig, & Allen J. P. (Eds.), NIAAA research monograph-alcohol and tobacco: From basic science to clinical practice Bethesda (pp. 37–57). MD: US Government Printing Office.
Flay, B. R., Petraitis, J., & Hu, F. B. (1999). Psychosocial risk and protective factors for adolescent tobacco use. Nicotine and Tobacco Research, 1, S59–S65.
Flint, A. J., & Novotny, T. E. (1997). Poverty status and cigarette smoking prevalence and cessation in the united states, 1983–1993: The independent risk of being poor. Tobacco Control, 6(1), 14–18.
Gilman, S. E., Martin, L. T., Abrams, D. B., Kawachi, I., Kubzansky, L., Loucks, E. B., et al. (2008). Educational attainment and cigarette smoking: A causal association? International Journal of Epidemiology, 37(3), 615–624.
Giovino, G. A., Henningfield, J. E., Tomar, S. L., Escobedo, L. G., & Slade, J. (1995). Epidemiology of tobacco use and dependence. Epidemiologic reviews, 17(1), 48–65.
Giovino, G. A., Mirza, S. A., Samet, J. M., Gupta, P. C., Jarvis, M. J., Bhala, N., et al. (2012). Tobacco use in 3 billion individuals from 16 countries: An analysis of nationally representative cross-sectional household surveys. The Lancet, 380(9842), 668–679.
Gouda, H. N., Charlson, F., Sorsdahl, K., Ahmadzada, S., Ferrari, A. J., Erskine, H., et al. (2019). Burden of non-communicable diseases in sub-saharan africa, 1990–2017: Results from the global burden of disease study 2017. The Lancet Global Health, 7(10), e1375–e1387.
Higgins, S. T., Kurti, A. N., Redner, R., White, T. J., Gaalema, D. E., Roberts, M. E., et al. (2015). A literature review on prevalence of gender differences and intersections with other vulnerabilities to tobacco use in the united states, 2004–2014. Preventive medicine, 80, 89–100.
Howe, L. D., Hargreaves, J. R., Gabrysch, S., & Huttly, S. R. (2009). Is the wealth index a proxy for consumption expenditure? A systematic review. Journal of Epidemiology and Community Health, 63(11), 871–877.
Idris, B. I., Giskes, K., Borrell, C., Benach, J., Costa, G., Federico, B., et al. (2007). Higher smoking prevalence in urban compared to non-urban areas: Time trends in six European countries. Health and place, 13(3), 702–712.
Kabir, M., & Goh, K.-L. (2014). Determinants of tobacco use among students aged 13–15 years in Nepal and Sri Lanka: Results from the global youth tobacco survey, 2007. Health Education Journal, 73(1), 51–61.
Kaplan, M., Carriker, L., & Waldron, I. (1990). Gender differences in tobacco use in Kenya. Social Science and Medicine, 30(3), 305–310.
Kauffman, S. E., Silver, P., & Poulin, J. (1997). Gender differences in attitudes toward alcohol, tobacco, and other drugs. Social Work, 42(3), 231–241.
KNBS (2014). Global adult tobacco survey. Kenya report 2014. Kenya: Kenya National Bureau of Statistics.
Kolenikov, S., & Angeles, G. (2009). Socioeconomic status measurement with discrete proxy variables: Is principal component analysis a reliable answer? Review of Income and Wealth, 55(1), 128–165.
Koning, P., Webbink, D., & Martin, N. G. (2015). The effect of education on smoking behavior: New evidence from smoking durations of a sample of twins. Empirical Economics, 48(4), 1479–1497.
Legleye, S., Khlat, M., Beck, F., & Peretti-Watel, P. (2011). Widening inequalities in smoking initiation and cessation patterns: A cohort and gender analysis in france. Drug and Alcohol Dependence, 117(2), 233–241.
Leventhal, A. M., Waters, A. J., Boyd, S., Moolchan, E. T., Lerman, C., & Pickworth, W. B. (2007). Gender differences in acute tobacco withdrawal: Effects on subjective, cognitive, and physiological measures. Experimental and Clinical Psychopharmacology, 15(1), 21–36.
Lindelow, M. (2006). Sometimes more equal than others: How health inequalities depend on the choice of welfare indicator. Health Economics, 15(3), 263–279.
Liu, H., Rizzo, J. A., Sun, Q., & Wu, F. (2015). How do smokers respond to cigarette taxes? Evidence from china’s cigarette industry. Health Economics, 24(10), 1314–1330.
Mackenbach, J. P., Looman, C. W., Artnik, B., Bopp, M., Deboosere, P., Dibben, C., et al. (2017). ‘Fundamental causes’ of inequalities in mortality: An empirical test of the theory in 20 European populations. Sociology of Health and Illness, 39(7), 1117–1133.
Maralani, V. (2014). Understanding the links between education and smoking. Social Science Research, 48, 20–34.
Mathers, C. D., & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. PloS Medicine, 3(11), 2011–2030.
McKenzie, D. J. (2005). Measuring inequality with asset indicators. Journal of Population Economics, 18(2), 229–260.
Morrow, M., & Barraclough, S. (2010). Gender equity and tobacco control: Bringing masculinity into focus. Global Health Promotion, 17(1_suppl), 21–28.
Ngaruiya, C., Abubakar, H., Kiptui, D., Kendagor, A., Ntakuka, M. W., Nyakundi, P., et al. (2018). Tobacco use and its determinants in the 2015 Kenya who steps survey. BMC Public Health, 18(3), 1–13.
O’Donnell, O., van Doorslaer, E., Wagstaff, A., & Lindelow, M. (2007). Analyzing health equity using household survey data: A guide to techniques and their implementation. Washington: The World Bank.
Peretti-Watel, P., L’Haridon, O., & Seror, V. (2013). Time preferences, socioeconomic status and smokers’ behaviour, attitudes and risk awareness. The European Journal of Public Health, 23(5), 783–788.
Phelan, J. C., & Link, B. G. (2005). Controlling disease and creating disparities: A fundamental cause perspective. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 60(Special_Issue_2), S27–S33.
Phelan, J. C., Link, B. G., Diez-Roux, A., Kawachi, I., & Levin, B. (2004). “Fundamental causes” of social inequalities in mortality: A test of the theory. Journal of Health and Social Behavior, 45(3), 265–285.
Phelan, J. C., Link, B. G., & Tehranifar, P. (2010). Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior, 51(1_suppl), S28–S40.
Prescott, E., Osler, M., Anderson, P. K., Hein, H. O., Borch-Johnsen, K., Lange, P., et al. (1998). Mortality in women and men in relation to smoking. International Journal of Epidemiology, 27(1), 27–32.
Purcell, K. R., O’Rourke, K., & Rivis, M. (2015). Tobacco control approaches and inequity—how far have we come and where are we going? Health Promotion International, 30(suppl_2), ii89–ii101.
Qasim, M. (2016). Using the theory of fundamental causes to show the potential effects of socioeconomic status on surgical outcomes. Journal of Health Disparities Research and Practice, 9(2), 143–153.
Rubin, M. S., Colen, C. G., & Link, B. G. (2010). Examination of inequalities in HIV/AIDS mortality in the united states from a fundamental cause perspective. American Journal of Public Health, 100(6), 1053–1059.
Sander, W. (1995). Schooling and quitting smoking. The Review of Economics and Statistics, 77(1), 191–199.
Shohaimi, S., Luben, R., Wareham, N., Day, N., Bingham, S., Welch, A., et al. (2003). Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class. A cross sectional study in the Norfolk cohort of the European investigation into cancer (Epic-Norfolk). Journal of Epidemiology and Community Health, 57(4), 270–276.
Silverstein, B., Feld, S., & Kozlowski, L. T. (1980). The availability of low-nicotine cigarettes as a cause of cigarette smoking among teenage females. Journal of Health and Social Behavior, 21(4), 383–388.
Stewart, F. (2010). Horizontal inequalities in Kenya and the political disturbances of 2008: Some implications for aid policy. Conflict, Security and Development, 10(1), 133–159.
Thakur, J., Prinja, S., Bhatnagar, N., Rana, S. K., Sinha, D. N., & Singh, P. K. (2015). Widespread inequalities in smoking and smokeless tobacco consumption across wealth quintiles in states of India: Need for targeted interventions. The Indian Journal of Medical Research, 141(6), 789–798.
US Department of Health Human Services (2004). The health consequences of smoking: A report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 62.
Valdez, A., Kaplan, C. D., & Curtis, R. L., Jr. (2007). Aggressive crime, alcohol and drug use, and concentrated poverty in 24 US urban areas. The American Journal of Drug and Alcohol Abuse, 33(4), 595–603.
Van Doorslaer, E., & Jones, A. M. (2003). Inequalities in self-reported health: Validation of a new approach to measurement. Journal of Health Economics, 22(1), 61–87.
Wagstaff, A., Van Doorslaer, E., & Watanabe, N. (2003). On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. Journal of Econometrics, 112(1), 207–223.
Waldron, I. (1991). Patterns and causes of gender differences in smoking. Social Science and Medicine, 32(9), 989–1005.
Waldron, I., Bratelli, G., & Carriker, L. (1988a). Gender differences in tobacco use in Asian, African, and Latin American so-cieties. Social Science and Medicine, 27, 1269–1275.
Waldron, I., Bratelli, G., Carriker, L., Sung, W.-C., Vogeli, C., & Waldman, E. (1988b). Gender differences in tobacco use in Africa, Asia, the Pacific, and Latin America. Social Science and Medicine, 27(11), 1269–1275.
Wang, Y., Browne, D. C., Storr, C. L., & Wagner, F. A. (2005). Gender and the tobacco–depression relationship: A sample of African American college students at a historically black college or university (HBCU). Addictive Behaviors, 30(7), 1437–1441.
Wasserman, J., Manning, W. G., Newhouse, J. P., & Winkler, J. D. (1991). The effects of excise taxes and regulations on cigarette smoking. Journal of Health Economics, 10(1), 43–64.
WHO. (2012). Who global report on mortality attributable to tobacco. Geneva: World Health Organization.
Willson, A. E. (2009). Fundamental causes’ of health disparities: A comparative analysis of Canada and the united states. International Sociology, 24(1), 93–113.
Acknowledgement
This work was presented at the Center of Research in Economics and Management (CREM, CNRS 6211)’s seminar in June 2018 at Rennes University (France). We are grateful for the comments received which help to improve the quality of the paper. We are grateful to the two anonymous reviewers for their constructive comments. The usual disclaimer applies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
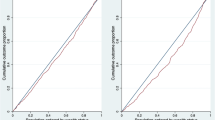
See Fig.
Construction of the wealth index using principal component analysis, number of components, and percent explained variance. Since these variables are binary outcomes, we use the polychoric principal component analysis (PCA). We choose a total number of two components which explained approximately 65% of the total variance. Sampling weights are used to account for the sampling design of the survey
See Tables
6,
7,
8,
9 and
Rights and permissions
About this article
Cite this article
Donfouet, H.P.P., Mohamed, S.F. & Malin, E. Socioeconomic inequality in tobacco use in Kenya: a concentration analysis. Int J Health Econ Manag. 21, 247–269 (2021). https://doi.org/10.1007/s10754-020-09292-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-020-09292-0