Abstract
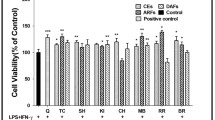
Wheat is a major diet from many years; apart from its nutritious value, the wheat protein gliadin is responsible for many inflammatory diseases like celiac disease (CD), and non-celiac gluten sensitivity (NCGS). In this study, the gliadin-induced inflammation and associated cellular damage along with the protective role of curcumin was evaluated using human intestinal cell lines (HCT-116 and HT-29) as a model. Cells were cultured and exposed to 160 μg/ml of gliadin, 100 μM H2O2, and 10 μM curcumin (3 h pretreatment) followed by the assessment of inflammation. Spectrophotometric methods, real-time-PCR, ELISA, Western blotting, and confocal microscopy techniques were used to assess inflammatory markers such as advanced oxidation protein products (AOPPs) level, activity of myeloperoxidase (MPO) and NADPH oxidase (NOX), cytokines, and cell damage markers. The results show that gliadin increases the AOPPs level and the activity of MPO and NOX expression. It enhances inflammation by increasing expression of pro-inflammatory cytokines, altered expression of anti-inflammatory, and regulatory cytokines. It exacerbates the cellular damage by increasing MMP-2 and 9 and decreasing integrin α and β expression. Gliadin promotes disease pathogenesis by inducing the inflammation and cellular damage which further alter the cellular homeostasis. The pretreatment of curcumin counteracts the adverse effect of gliadin and protect the cells via diminishing the inflammation and help the cell to regain the cellular morphology suggesting phytochemical-based remedial interventions against wheat allergies.








Similar content being viewed by others
References
Shewry, Peter R., Nigel G. Halford, Peter S. Belton, and Arthur S. Tatham. 2002. The structure and properties of gluten: an elastic protein from wheat grain. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences 357 (1418): 133–142.
Balakireva, Anastasia V., and Andrey A. Zamyatnin. 2016. Properties of gluten intolerance: gluten structure, evolution, pathogenicity and detoxification capabilities. Nutrients 8 (10): 644.
Molberg, Øyvind, Stephen N. Mcadam, Roman Körner, Hanne Quarsten, Christel Kristiansen, Lars Madsen, Lars Fugger, Helge Scott, Ove Norén, and Peter Roepstorff. 1998. Tissue transglutaminase selectively modifies gliadin peptides that are recognized by gut-derived T cells in celiac disease. Nature Medicine 4 (6): 713–717.
Mayassi, Toufic, Kristin Ladell, Herman Gudjonson, James E. McLaren, Dustin G. Shaw, Mai T. Tran, Jagoda J. Rokicka, Ian Lawrence, Jean-Christophe Grenier, and Vincent van Unen. 2019. Chronic inflammation permanently reshapes tissue-resident immunity in celiac disease. Cell 176 (5): 967–981 e919.
Gupta, Kunj Bihari, Shishir Upadhyay, Ram Gopal Saini, Anil K Mantha, and Monisha Dhiman. 2018. Inflammatory response of gliadin protein isolated from various wheat varieties on human intestinal cell line. Journal of Cereal Science 81:91-98.
Thakur, Shweta, Monisha Dhiman, and Anil K. Mantha. 2018. APE1 modulates cellular responses to organophosphate pesticide-induced oxidative damage in non-small cell lung carcinoma A549 cells. Molecular and Cellular Biochemistry 441 (1-2): 201–216.
Levrand, Sandra, Benoît Pesse, François Feihl, Bernard Waeber, Pal Pacher, Joëlle Rolli, Marie-Denise Schaller, and Lucas Liaudet. 2005. Peroxynitrite is a potent inhibitor of NF-κB activation triggered by inflammatory stimuli in cardiac and endothelial cell lines. Journal of Biological Chemistry 280 (41): 34878–34887.
Dhiman, Monisha, Jose Guillermo Estrada-Franco, Jasmine M. Pando, Francisco J. Ramirez-Aguilar, Heidi Spratt, Sara Vazquez-Corzo, Gladys Perez-Molina, Rosa Gallegos-Sandoval, Roberto Moreno, and Nisha Jain Garg. 2009. Increased myeloperoxidase activity and protein nitration are indicators of inflammation in patients with Chagas' disease. Clinical and Vaccine Immunology 16 (5): 660–666.
Baskol, Gülden, Hüseyin Demir, Mevlut Baskol, Eser Kilic, Filiz Ates, Cigdem Karakukcu, and Muzaffer Ustdal. 2006. Investigation of protein oxidation and lipid peroxidation in patients with rheumatoid arthritis. Cell Biochemistry and Function: Cellular biochemistry and its modulation by active agents or disease 24 (4): 307–311.
Vaday, Gayle G., Donna M. Peehl, Pournima A. Kadam, and Diana M. Lawrence. 2006. Expression of CCL5 (RANTES) and CCR5 in prostate cancer. The Prostate 66 (2): 124–134.
Cholia, Ravi P., Monisha Dhiman, Raj Kumar, and Anil K. Mantha. 2018. Oxidative stress stimulates invasive potential in rat C6 and human U-87 MG glioblastoma cells via activation and cross-talk between PKM2, ENPP2 and APE1 enzymes. Metabolic Brain Disease 33 (4): 1307–1326.
Upadhyay, Shishir, Anil K Mantha, and Monisha Dhiman. 2020. Glycyrrhiza glabra (Licorice) root extract attenuates doxorubicin-induced cardiotoxicity via alleviating oxidative stress and stabilising the cardiac health in H9c2 cardiomyocytes. Journal of Ethnopharmacology:112690.
Monguzzi, Erika, Laura Marabini, Luca Elli, Valentina Vaira, Stefano Ferrero, Francesca Ferretti, Federica Branchi, Gabriella Gaudioso, Alice Scricciolo, and Vincenza Lombardo. 2019. Gliadin effect on the oxidative balance and DNA damage: An in-vitro, ex-vivo study. Digestive and Liver Disease 51 (1): 47–54.
Qiao, Shuo-Wang, Melinda Ráki, Kristin S. Gunnarsen, Geir-Åge Løset, Knut E.A. Lundin, Inger Sandlie, and Ludvig M. Sollid. 2011. Posttranslational modification of gluten shapes TCR usage in celiac disease. The Journal of Immunology 187 (6): 3064–3071.
Kagnoff, Martin F. 2007. Celiac disease: pathogenesis of a model immunogenetic disease. The Journal of Clinical Investigation 117 (1): 41–49.
McAllister, Christopher S., and Martin F. Kagnoff. 2012. The immunopathogenesis of celiac disease reveals possible therapies beyond the gluten-free diet. Seminars in Immunopathology 4 (4): 581–600.
Kristjánsson, Gudjon, Per Venge, Alkwin Wanders, Lars Lööf, and Roger Hällgren. 2004. Clinical and subclinical intestinal inflammation assessed by the mucosal patch technique: studies of mucosal neutrophil and eosinophil activation in inflammatory bowel diseases and irritable bowel syndrome. Gut 53 (12): 1806–1812.
Peterson, Christer G.B., Elisabeth Eklund, Yesuf Taha, Yngve Raab, and Marie Carlson. 2002. A new method for the quantification of neutrophil and eosinophil cationic proteins in feces: establishment of normal levels and clinical application in patients with inflammatory bowel disease. The American Journal of Gastroenterology 97 (7): 1755–1762.
Gryszczyńska, Bogna, Dorota Formanowicz, Magdalena Budzyń, Maria Wanic-Kossowska, Elżbieta Pawliczak, Piotr Formanowicz, Wacław Majewski, Krzysztof Wojciech Strzyżewski, Magdalena P. Kasprzak, and Maria Iskra. 2017. Advanced oxidation protein products and carbonylated proteins as biomarkers of oxidative stress in selected atherosclerosis-mediated diseases. BioMed Research International 2017. https://doi.org/10.1155/2017/4975264.
Sayar, Ersin, Sebahat Özdem, Gülbahar Uzun, Ali İşlek, Aygen Yılmaz, and Reha Artan. 2015. Total oxidant status, total antioxidant capacity and ischemia modified albumin levels in children with celiac disease. Turkish Journal of Pediatrics 57 (5): 498–503.
Panday, Arvind, Malaya K. Sahoo, Diana Osorio, and Sanjay Batra. 2015. NADPH oxidases: an overview from structure to innate immunity-associated pathologies. Cellular & Molecular Immunology 12 (1): 5–23.
Xu, Qing, Swati Choksi, Qu Jianhui, Jonathan Jang, Moran Choe, Botond Banfi, John F. Engelhardt, and Zheng-Gang Liu. 2016. NADPH Oxidases are essential for macrophage differentiation. The Journal of Biological Chemistry 291 (38): 20030–20041.
Krause, Karl-Heinz, and Karen Bedard. 2008. NOX enzymes in immuno-inflammatory pathologies. In Seminars in Immunopathology30(3):193-194..
Daulatzai, Mak A. 2015. Non-celiac gluten sensitivity triggers gut dysbiosis, neuroinflammation, gut-brain axis dysfunction, and vulnerability for dementia. CNS & Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders) 14 (1): 110–131.
Patlevič, Peter, Janka Vašková, Pavol Švorc Jr, Ladislav Vaško, and Pavol Švorc. 2016. Reactive oxygen species and antioxidant defense in human gastrointestinal diseases. Integrative Medicine Research 5 (4): 250–258.
Antvorskov, Julie C., Petra Fundova, Karsten Buschard, and David P. Funda. 2013. Dietary gluten alters the balance of pro-inflammatory and anti-inflammatory cytokines in T cells of BALB/c mice. Immunology 138 (1): 23–33.
Forsberg, Göte, Olle Hernell, Sten Hammarström, and Marie-Louise Hammarström. 2007. Concomitant increase of IL-10 and pro-inflammatory cytokines in intraepithelial lymphocyte subsets in celiac disease. International Immunology 19 (8): 993–1001.
Kumar, B.V. Mohan, M. Vijaykrishnaraj, Nawneet K. Kurrey, Vijay S. Shinde, and P. Prabhasankar. 2019. Prolyl endopeptidase-degraded low immunoreactive wheat flour attenuates immune responses in Caco-2 intestinal cells and gluten-sensitized BALB/c mice. Food and Chemical Toxicology 129: 466–475.
Abadie, Valérie, and Bana Jabri. 2014. IL-15: a central regulator of celiac disease immunopathology. Immunological Reviews 260 (1): 221–234.
Mention, Jean-Jacques, Mélika Ben Ahmed, Bernadette Bègue, Ullah Barbe, Virginie Verkarre, Vahid Asnafi, Jean-frédéric Colombel, Paul-henri Cugnenc, Frank M. Ruemmele, and Elisabeth Mcintyre. 2003. Interleukin 15: a key to disrupted intraepithelial lymphocyte homeostasis and lymphomagenesis in celiac disease. Gastroenterology 125 (3): 730–745.
Maiuri, Luigi, Carolina Ciacci, Salvatore Auricchio, Virginia Brown, Sonia Quaratino, and Marco Londei. 2000. Interleukin 15 mediates epithelial changes in celiac disease. Gastroenterology 119 (4): 996–1006.
Jabri, Bana, Natacha Patey–Mariaud De Serre, Christophe Cellier, Kelly Evans, Cécile Gache, Carla Carvalho, Jean–François Mougenot, Matthieu Allez, Raymond Jian, and Pierre Desreumaux. 2000. Selective expansion of intraepithelial lymphocytes expressing the HLA-E–specific natural killer receptor CD94 in celiac disease. Gastroenterology 118 (5):867-879.
Fernandez-Jimenez, Nora, Ainara Castellanos-Rubio, Leticia Plaza-Izurieta, Iñaki Irastorza, Xabier Elcoroaristizabal, Amaia Jauregi-Miguel, Tamara Lopez-Euba, Carlos Tutau, Marian M. de Pancorbo, and Juan Carlos Vitoria. 2014. Coregulation and modulation of NFκB-related genes in celiac disease: uncovered aspects of gut mucosal inflammation. Human Molecular Genetics 23 (5): 1298–1310.
Przemioslo, R.T., M. Kontakou, V. Nobili, and P.J. Ciclitira. 1994. Raised pro-inflammatory cytokines interleukin 6 and tumour necrosis factor alpha in coeliac disease mucosa detected by immunohistochemistry. Gut 35 (10): 1398–1403.
Sturgess, R.P., L.B. Hooper, J. Spencer, C.H. Hung, J.M. Nelufer, and P.J. Ciclitira. 1992. Effects of interferon-y and tumour necrosis factor-cu on epithelial HLA class-II expression on jejunal mucosal biopsy specimens cultured in vitro. Scandinavian Journal of Gastroenterology 27 (11): 907–911.
Maiuri, Maria Chiara, Daniela De Stefano, Guido Mele, Simona Fecarotta, Luigi Greco, Riccardo Troncone, and Rosa Carnuccio. 2003. Nuclear factor κB is activated in small intestinal mucosa of celiac patients. Journal of Molecular Medicine 81 (6): 373–379.
de Almeida, Natália Ellen Castilho, Franciele Grego Esteves, José Roberto Aparecido dos Santos-Pinto, Carla Peres de Paula, Anderson Ferreira da Cunha, Iran Malavazi, Mario Sergio Palma, and Edson Rodrigues-Filho. 2020. Digestion of intact gluten proteins by bifidobacterium species: reduction of cytotoxicity and proinflammatory responses. Journal of Agricultural and Food Chemistry 68 (15): 4485–4492.
Wan, Fengyi, and Michael J. Lenardo. 2009. Specification of DNA binding activity of NF-κB proteins. Cold Spring Harbor Perspectives in Biology 1 (4): a000067.
Liu, Ting, Lingyun Zhang, Donghyun Joo, and Shao-Cong Sun. 2017. NF-κB signaling in inflammation. Signal Transduction and Targeted Therapy 2 (1): 1–9.
Kárpáti, Sarolta, Miklós Sárdy, Krisztián Németh, Balázs Mayer, Neil Smyth, Mats Paulsson, and Heiko Traupe. 2018. Transglutaminases in autoimmune and inherited skin diseases: The phenomena of epitope spreading and functional compensation. Experimental Dermatology 27 (8): 807–814.
Ciccocioppo, R., A. Di Sabatino, C. Ara, F. Biagi, M. Perilli, G. Amicosante, M.G. Cifone, and G.R. Corazza. 2003. Gliadin and tissue transglutaminase complexes in normal and coeliac duodenal mucosa. Clinical and Experimental Immunology 134 (3): 516–524.
Bagatur, Yesim, Ayca Zeynep Ilter Akulke, Ajna Bihorac, Merve Erdem, and Dilek Telci. 2018. Tissue transglutaminase expression is necessary for adhesion, metastatic potential and cancer stemness of renal cell carcinoma. Cell Adhesion & Migration 12 (2): 138–151.
Lai, Thung-S, Robert A. Lindberg, Hua-Lin Zhou, Zishan A. Haroon, Mark W. Dewhirst, Alfred Hausladen, Y.-L. Juang, Jonathan S. Stamler, and Charles S. Greenberg. 2017. Endothelial cell-surface tissue transglutaminase inhibits neutrophil adhesion by binding and releasing nitric oxide. Scientific Reports 7 (1): 1–9.
Ciccocioppo, Rachele, Antonio Di Sabatino, Michael Bauer, Daniela N. Della Riccia, Francesca Bizzini, Federico Biagi, Maria G. Cifone, Gino R. Corazza, and Detlef Schuppan. 2005. Matrix metalloproteinase pattern in celiac duodenal mucosa. Laboratory Investigation 85 (3): 397–407.
Acknowledgments
KBG acknowledges the ICMR, New Delhi, for providing financial assistance in term of JRF/SRF. Central Instrumentation Laboratory (CIL) of CUPB thankfully acknowledged for confocal microscope facility. Authors are also thankful to the Honorable Vice-Chancellor for providing the necessary facilities at the Central University of Punjab, Bathinda, India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gupta, K.B., Mantha, A.K. & Dhiman, M. Mitigation of Gliadin-Induced Inflammation and Cellular Damage by Curcumin in Human Intestinal Cell Lines. Inflammation 44, 873–889 (2021). https://doi.org/10.1007/s10753-020-01383-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-020-01383-x