Abstract
Introduction
The objective of this study was to evaluate the utility of three-dimensional (3D) versus conventional two-dimensional (2D) endoscopy for fetal myelomeningocele repair using a low-fidelity fetoscopic surgical simulator.
Methods
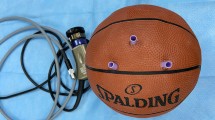
A low-fidelity fetoscopic box trainer was developed for surgical simulation of myelomeningocele repair. Participants with varying surgical experience were recruited and completed three essential tasks (cutting skin, dural patch placement, and suturing skin) using both 2D and 3D endoscopic visualization. Participants were randomized to begin all tasks in either 2D or 3D. Time to completion was measured for each task, and each participant subsequently completed the NASA Load Index test and a questionnaire evaluating their experience.
Results
Sixteen participants completed the study tasks using both 2D and 3D endoscopes in the simulator. While the mean performance time across all tasks was shorter with 3D versus 2D endoscopy (cutting skin, 47 vs. 54 seconds; dural patch placement, 38 vs. 52 seconds; and suturing skin, 424 vs. 499 seconds), the results did not reach statistical significance. When comparing times to completion of each of the three tasks between levels of expertise, participants in the expert category were faster when suturing skin on the 2D modality (P = 0.047). Under 3D visualization, experts were faster at cutting the skin (P = 0.008). When comparing experiences using the NASA-TLX test, participants felt that their performance was better using 3D over the 2D system (P = 0.045). Overall, 13 of 16 (81.3%) participants preferred 3D over 2D visualization.
Conclusions
Three-dimensional endoscopes could potentially be used in the near future for relative improvement in visualization and possibly performance during complex fetoscopic procedures such as prenatal repair of myelomeningocele defects. Further studies utilizing 3D scopes for other related procedures may potentially support clinical implementation of this technology in fetal surgery and also prove to be a useful tool in surgical training.





Similar content being viewed by others
Data availability
Data and materials are available from the corresponding author upon request.
References
Adzick NS, Thom EA, Spong CY, Brock JW, Burrows PK, Johnson MP, Howell LJ, Farrell JA, Dabrowiak ME, Sutton LN, Gupta N, Tulipan NB, D’Alton ME, Farmer DL, Investigators M (2011) A randomized trial of prenatal versus postnatal repair of myelomeningocele. N Engl J Med 364:993–1004
Bauer DF, Beier AD, Nikas DC, Assassi N, Blount J, Durham SR, Flannery AM, Klimo P, McClung-Smith C, Rehring P, Tamber MS, Tyagi R, Mazzola CA (2019) Congress of neurological surgeons systematic review and evidence-based guideline on the management of patients with myelomeningocele: whether prenatal or postnatal closure affects future ambulatory status. Neurosurgery 85:E409–E411
Patel SK, Habli MA, McKinney DN, Tabbah SM, Lim FY, Peiro JL, Stevenson CB (2020) Fetoscopic multilayer, dural patch closure technique for intrauterine myelomeningocele repair: 2-dimensional operative video. Oper Neurosurg (Hagerstown)
Kozlov Y, Kovalkov K, Nowogilov V (2016) 3D Laparoscopy in neonates and infants. J Laparoendosc Adv Surg Tech A 26:1021–1027
Bickerton R, Nassimizadeh AK, Ahmed S (2019) Three-dimensional endoscopy: the future of nasoendoscopic training. Laryngoscope 129:1280–1285
Rampinelli V, Doglietto F, Mattavelli D, Qiu J, Raffetti E, Schreiber A, Villaret AB, Kucharczyk W, Donato F, Fontanella MM, Nicolai P (2017) Two-dimensional high definition versus three-dimensional endoscopy in endonasal skull base surgery: a comparative preclinical study. World Neurosurg 105:223–231
Szold A (2005) Seeing is believing: visualization systems in endoscopic surgery (video, HDTV, stereoscopy, and beyond). Surg Endosc 19:730–733
Chan AC, Chung SC, Yim AP, Lau JY, Ng EK, Li AK (1997) Comparison of two-dimensional vs three-dimensional camera systems in laparoscopic surgery. Surg Endosc 11:438–440
Herron DM, Lantis JC, Maykel J, Basu C, Schwaitzberg SD (1999) The 3-D monitor and head-mounted display. A quantitative evaluation of advanced laparoscopic viewing technologies. Surg Endosc 13:751–755
McDougall EM, Soble JJ, Wolf JS, Nakada SY, Elashry OM, Clayman RV (1996) Comparison of three-dimensional and two-dimensional laparoscopic video systems. J Endourol 10:371–374
Birkett DH, Josephs LG, Este-McDonald J (1994) A new 3-D laparoscope in gastrointestinal surgery. Surg Endosc 8:1448–1451
Taffinder N, Smith SG, Huber J, Russell RC, Darzi A (1999) The effect of a second-generation 3D endoscope on the laparoscopic precision of novices and experienced surgeons. Surg Endosc 13:1087–1092
Hart S (2006) NASA-Task Load Index (NASA-TLX); 20 years later. Human Factors and Ergonomics Society Annual Meeting, pp 904-908
SG H, LE S (1988) Development of NASA-TLX (Task Load Index): results of empirical and theoretical research. In: PA H, N M (eds) Human mental workload. North Holland Press, Amsterdam
Van Gompel JJ, Tabor MH, Youssef AS, Lau T, Carlson AP, van Loveren HR, Agazzi S (2014) Field of view comparison between two-dimensional and three-dimensional endoscopy. Laryngoscope 124:387–390
Kari E, Oyesiku NM, Dadashev V, Wise SK (2012) Comparison of traditional 2-dimensional endoscopic pituitary surgery with new 3-dimensional endoscopic technology: intraoperative and early postoperative factors. Int Forum Allergy Rhinol 2:2–8
Fraser JF, Allen B, Anand VK, Schwartz TH (2009) Three-dimensional neurostereoendoscopy: subjective and objective comparison to 2D. Minim Invasive Neurosurg 52:25–31
Zaidi HA, Zehri A, Smith TR, Nakaji P, Laws ER (2016) Efficacy of three-dimensional endoscopy for ventral skull base pathology: a systematic review of the literature. World Neurosurg 86:419–431
Wataganara T, Gosavi A, Nawapun K, Vijayakumar PD, Phithakwatchara N, Choolani M, Su LL, Biswas A, Mattar CNZ (2018) Model surgical training: skills acquisition in fetoscopic laser photocoagulation of monochorionic diamniotic twin placenta using realistic simulators. J Vis Exp
Belfort MA, Whitehead WE, Bednov A, Shamshirsaz AA (2018) Low-fidelity simulator for the standardized training of fetoscopic meningomyelocele repair. Obstet Gynecol 131:125–129
Ghasemloonia A, Maddahi Y, Zareinia K, Lama S, Dort JC, Sutherland GR (2017) Surgical skill assessment using motion quality and smoothness. J Surg Educ 74:295–305
Werner H, Lopes J, Tonni G, Araujo Júnior E (2015) Physical model from 3D ultrasound and magnetic resonance imaging scan data reconstruction of lumbosacral myelomeningocele in a fetus with Chiari II malformation. Childs Nerv Syst 31:511–513
Werner H, Ribeiro G, Lopes J, Sá RAM, Maia F, Castro P, Araujo Júnior E (2020) Virtual navigation for the improvement of parents counseling and the planning of fetal endoscopic myelomeningocele repair. Childs Nerv Syst
Acknowledgments
The authors would like to acknowledge Ahmed Hussein, MD, for his assistance with statistical analysis and Kora Tristan Montemagno, Rebecca Allessia Fumagelli, and Ikrame Labiad for their technical assistance with simulator setup and data collection. Thank you to Daniel Russo MD, Adolfo Etchegaray MD, Emrah Aydin MD, and all the surgeons that participated in this testing. We would also like to thank the Goodyear Lab and University of Cincinnati Department of Neurosurgery for providing laboratory space to carry out this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Patel, Kashyrina, Duru, Miyabe, Lim, Peiro, and Stevenson have no conflicts of interest or financial ties to disclose. None of the authors have any financial or commercial relationships with Applied Medical, TrueTM, Karl Storz, or Medtronic/Covidien.
Ethics approval
Not applicable.
Consent to participate
All volunteers consented to participate in this study.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, S.K., Kashyrina, O., Duru, S. et al. Comparison of two- and three-dimensional endoscopic visualization for fetal myelomeningocele repair: a pilot study using a fetoscopic surgical simulator. Childs Nerv Syst 37, 1613–1621 (2021). https://doi.org/10.1007/s00381-020-04999-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04999-4