Abstract
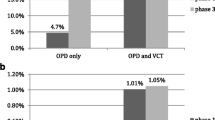
We investigated a novel community-based HIV testing and counseling (HTC) strategy by recruiting men from bars in northern Tanzania in order to identify new HIV infections. All bars in the town of Boma Ng’ombe were identified and male patrons were systematically invited to participate in a health study. HIV testing was offered to all enrolled participants. Outputs included HIV test yield, cost per diagnosis, and comparison of our observed test yield to that among male patients contemporaneously tested at five local facility-based HTC. We enrolled 366 participants and identified 17 new infections – providing a test yield of 5.3% (95% Confidence interval [CI] 3.3–8.4). The test yield among men contemporaneously tested at five local HTC centers was 2.1% (95% CI 1.6–2.8). The cost-per-diagnosis was $634. Our results suggest that recruiting male bar patrons for HIV testing is efficient for identifying new HIV infections. The scalability of this intervention warrants further evaluation.
Resumen
Investigamos una novedosa estrategia comunitaria de asesoramiento y pruebas de VIH (HTC) reclutando hombres de los bares del norte de Tanzania para identificar nuevas infecciones de VIH. Se identificaron todos los bares de la ciudad de Boma Ng'ombe y se invitó sistemáticamente a los clientes varones a participar en un estudio de salud. Se ofrecieron pruebas de VIH a todos los participantes inscritos. Los resultados incluyeron los resultados de las pruebas de VIH, el costo por diagnóstico y la comparación de nuestros resultados observados con los de los pacientes varones que simultáneamente se sometieron a pruebas en cinco centros locales de HTC. Se inscribieron 366 participantes y se identificaron 17 nuevas infecciones, proporcionando un resultado en las pruebas del 5.3% (intervalo de confianza [IC] del 95%: 3.3-8.4). Los resultados de las pruebas realizadas simultáneamente en cinco centros locales de HTC fue del 2.1% (IC del 95%: 1.6-2.8). El costo por diagnóstico fue de $634. Nuestros resultados sugieren que el reclutamiento de clientes masculinos para las pruebas de VIH fue eficiente para identificar nuevas infecciones de VIH. La escalabilidad de esta intervención merece una evaluación adicional.



Similar content being viewed by others
References
Joint United Nations Programme on HIV/AIDS. Knowledge is Power Knowledge is power: know your status, know your viral load. Geneva: Joint United Nations Programme on HIV/AIDS; 2018.
Tsai AC, Siedner MJ. The missing men: HIV treatment scale-up and life expectancy in Sub-Saharan Africa. PLoS Med. 2015;12(11):e1001906.
Sileo KM, Fielding-Miller R, Dworkin SL, Fleming PJ. What role do masculine norms play in men’s HIV testing in Sub-Saharan Africa?: A scoping review. AIDS Behav. 2018;22(8):2468–79.
Dovel K, Yeatman S, Watkins S, Poulin M. Men’s heightened risk of AIDS-related death: the legacy of gendered HIV testing and treatment strategies. AIDS. 2015;29(10):1123–5.
Leichliter JS, Paz-Bailey G, Friedman AL, Habel MA, Vezi A, Sello M, et al. “Clinics aren’t meant for men”: sexual health care access and seeking behaviours among men in Gauteng province, South Africa. Sahara J. 2011;8(2):82–8.
Pascoe L, Peacock D, Stemple L. Reaching men: addressing the blind spot in the HIV response. Int J Mens Soc Community Health. 2018;1(SP1):e57-70.
Fleming PJ, Colvin C, Peacock D, Dworkin SL. What role can gender-transformative programming for men play in increasing South African men’s HIV testing and engagement in HIV care and treatment? Cult Health Sex. 2016;18(11):1251–64.
Colvin CJ. Strategies for engaging men in HIV services. The Lancet HIV. 2019;6(3):e191-200.
Sharma M, Barnabas RV, Celum C. Community-based strategies to strengthen men’s engagement in the HIV care cascade in sub-Saharan Africa. PLoS Med. 2017;14(4):e1002262.
Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature. 2015;528(7580):S77-85.
Hlongwa M, Mashamba-Thompson T, Makhunga S, Muraraneza C, Hlongwana K. Men’s perspectives on HIV self-testing in sub-Saharan Africa: a systematic review and meta-synthesis. BMC Public Health. 2020;20(1):66.
Hatzold K, Gudukeya S, Mutseta MN, Chilongosi R, Nalubamba M, Nkhoma C, et al. HIV self‐testing: breaking the barriers to uptake of testing among men and adolescents in sub‐Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. J Int AIDS Soc. 2019;22(Suppl Suppl 1):e25244
WHO. Consolidated guidelines on HIV testing services 2015. Genera: WHO; 2015. p. 2015.
Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in Sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141.
Fritz KE, Woelk GB, Bassett MT, McFarland WC, Routh JA, Tobaiwa O, et al. The association between alcohol use, sexual risk behavior, and HIV infection among men attending Beerhalls in Harare, Zimbabwe. AIDS Behav. 2002;6(3):221–8.
Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC). Tanzania HIV Impact Survey (THIS) 2016–2017: Final Report. Dar es Salaam, Tanzania. December 2018. [Internet]. Available from: http://phia.icap.columbia.edu
Muhib FB, Lin LS, Stueve A, Miller RL, Ford WL, Johnson WD, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(Suppl 1):216–22.
Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56(4):423–32.
Francis JM, Weiss HA, Helander A, Kapiga SH, Changalucha J, Grosskurth H. Comparison of self-reported alcohol use with the alcohol biomarker phosphatidylethanol among young people in northern Tanzania. Drug Alcohol Depend. 2015;156:289–96.
Kwesigabo G, Mwangu MA, Kakoko DC, Warriner I, Mkony CA, Killewo J, et al. Tanzania’s health system and workforce crisis. J Public Health Policy. 2012;33(Suppl 1):S35-44.
Carrasco MA, Esser MB, Sparks A, Kaufman MR. HIV-alcohol risk reduction interventions in Sub-Saharan Africa: a systematic review of the literature and recommendations for a way forward. AIDS Behav. 2016;20(3):484–503.
Mak J, Mayhew SH, von Maercker A, Integra Research Team IRT, Colombini M. Men’s use of sexual health and HIV services in Swaziland: a mixed methods study. Sex Health. 2016;13(3):265–74.
Chamie G, Hickey MD, Kwarisiima D, Ayieko J, Kamya MR, Havlir DV. Universal HIV testing and treatment (UTT) integrated with chronic disease screening and treatment: the SEARCH study. Curr HIV/AIDS Rep. 2020;17(4):315–23.
Corbett EL, Dauya E, Matambo R, Cheung YB, Makamure B, Bassett MT, et al. Uptake of workplace HIV counselling and testing: a cluster-randomised trial in Zimbabwe. PLoS Med. 2006;3(7):e238.
Shapiro AE, van Heerden A, Krows M, Sausi K, Sithole N, Schaafsma TT, et al. An implementation study of oral and blood-based HIV self-testing and linkage to care among men in rural and peri-urban KwaZulu-Natal, South Africa. J Int AIDS Soc. 2020;23(S2):e25514.
De Cock KM, Barker JL, Baggaley R, El Sadr WM. Where are the positives? HIV testing in sub-Saharan Africa in the era of test and treat. AIDS. 2019;33(2):349–52.
Phillips AN, Cambiano V, Nakagawa F, Bansi-Matharu L, Wilson D, Jani I, et al. Cost-per-diagnosis as a metric for monitoring cost-effectiveness of HIV testing programmes in low-income settings in southern Africa: health economic and modelling analysis. J Int AIDS Soc. 2019;22(7):e25325.
Chang W, Chamie G, Mwai D, Clark TD, Thirumurthy H, Charlebois ED, et al. Cost and efficiency of a hybrid mobile multi-disease testing approach with high HIV testing coverage in East Africa. J Acquir Immune Defic Syndr. 2016;73(3):e39-45.
Lasry A, Bachanas P, Suraratdecha C, Alwano MG, Behel S, Pals S, et al. Cost of community-based HIV testing activities to reach saturation in Botswana. AIDS Behav. 2019;23(4):875–82.
de Beer I, Chani K, Feeley FG, Rinke de Wit TF, Sweeney-Bindels E, Mulongeni P. Assessing the costs of mobile voluntary counseling and testing at the work place versus facility based voluntary counseling and testing in Namibia. Rural Remote Health. 2015;15(4):3357.
Meehan S-A, Beyers N, Burger R. Cost analysis of two community-based HIV testing service modalities led by a Non-Governmental Organization in Cape Town, South Africa. BMC Health Serv Res [Internet]. 2017 Dec 2 [cited 2020 Jan 16];17. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5712171/
Hauck K. The costs of home-based HIV testing and counselling in sub-Saharan Africa and its association with testing yield: a literature review. Afr J AIDS Res. 2019;18(4):324–31.
Johnson C, Dalal S, Baggaley R, Hogan D, Parrott G, Mathews R, et al. Systematic review of HIV testing costs in high and low income settings [Internet]. Consolidated Guidelines on HIV Testing Services: 5Cs: Consent, Confidentiality, Counselling, Correct Results and Connection 2015. World Health Organization; 2015 [cited 2020 Oct 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK316032/
Tabana H, Nkonki L, Hongoro C, Doherty T, Ekström AM, Naik R, et al. A cost-effectiveness analysis of a home-based HIV counselling and testing intervention versus the standard (Facility Based) HIV testing strategy in rural South Africa. PLoS ONE. 2015;10(8):e0135048.
Mangenah C, Mwenge L, Sande L, Ahmed N, d’Elbée M, Chiwawa P, et al. Economic cost analysis of door-to-door community-based distribution of HIV self-test kits in Malawi, Zambia and Zimbabwe. J Int AIDS Soc. 2019;22(Suppl 1):e25255.
Ruzagira E, Baisley K, Kamali A, Biraro S, Grosskurth H. Linkage to HIV care after home-based HIV counselling and testing in sub-Saharan Africa: a systematic review. Tropical Med Int Health. 2017;22(7):807–21.
Acknowledgements
The authors would like to thank the study participants as well as the clinical staff and administration at the facility-based testing centers in Boma Ng’ombe. In addition, we would like to thank the village leaders and ward leaders in Hai district who supported the study.
Funding
This research was supported by the US NIH Fogarty International Center grant D43TW009337. DBM and PM received support from the NIH Ruth L. Kirschstein National Research Service Award (NRSA) 5T32AI007392.
Author information
Authors and Affiliations
Contributions
DBM and NMT conceived the study; DBM and NMT designed the study protocol; DBM, BN, and NMT implemented and supervised the study; DBM performed the data analysis; DBM drafted the manuscript; DBM, PM, AM, TP, JO, BN, and NMT critically revised the manuscript for content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest related to this work.
Ethical Approval
Ethics approval was obtained from the Institutional Review Board of Duke University, the Research Ethics Committee of Kilimanjaro Christian Medical Centre, and the Ethics Coordinating Committee of the Tanzanian National Institute for Medical Research.
Informed Consent
Written consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Madut, D.B., Manavalan, P., Mtalo, A. et al. Increasing the Uptake of HIV Testing among Men in Tanzania: A Novel Intervention for Bar Patrons. AIDS Behav 25, 2014–2022 (2021). https://doi.org/10.1007/s10461-020-03131-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-03131-6