Abstract
Background and Objective
Dissecting cellulitis of the scalp is a primary scarring alopecia. Isotretinoin is commonly referenced in the literature as a treatment for dissecting cellulitis. The objective of this article was to conduct a review and meta-analysis to assess the efficacy of isotretinoin for treating dissecting cellulitis of the scalp.
Methods
The following databases were searched for articles prior to 23 June, 2019: PubMed, Embase, Cochrane Central, CINAHL, and Web of Science. Multi-patient studies (more than three) that reported on the administration of isotretinoin for dissecting cellulitis were included. A pooled meta-analysis for improvement of disease burden after isotretinoin administration in patients with dissecting cellulitis of the scalp was performed. A fixed-effects model was used.
Results
Five articles were ultimately used for the quantitative meta-analysis. The overall efficacy rate of isotretinoin in treating dissecting cellulitis of the scalp was estimated to be 0.9 with a 95% confidence interval (0.81–0.97). The sensitivity analysis suggested that the overall efficacy is still very high, with a range of 0.83–0.94. Recurrence was seen in 24% (6/25) of patients. Common associated diseases amongst patients with dissecting cellulitis of the scalp were acne conglobata 20% (30/151) and hidradenitis suppurativa 19% (11/72).
Conclusions
Isotretinoin is an effective treatment for improving symptoms of dissecting cellulitis of the scalp. Disease recurrence is a common finding for those who undergo successful treatment.
Similar content being viewed by others
This review and meta-analysis found isotretinoin to be an effective treatment for improving symptoms of dissecting cellulitis. |
Recurrence after treatment was cited in a minority of patients treated with isotretinoin. |
Tumor necrosis factor-α inhibitors, adalimumab and infliximab, as well as ALA-PDT treatment have been detailed in case studies as potentially effective off-label treatments for refractory dissecting cellulitis. |
1 Introduction
Dissecting cellulitis of the scalp (DCS), or perifolliculitis capitis abscedens et suffodiens, is a rare, primary neutrophilic scarring alopecia [1]. Dissecting cellulitis of the scalp belongs to the “follicular occlusion tetrad,” composed of hidradenitis suppurativa, acne conglobate, and pilonidal cysts [2]. Dissecting cellulitis of the scalp is characterized by multiple confluent, suppurative nodules on the scalp that can cause patchy hair loss [3]. The nodules are often associated with pain and pruritus [4, 5]. Inflammatory nodules and abscesses may combine and with prolonged disease may lead to scarring alopecia [6]. The disease can be physically disfiguring and emotionally traumatic owing to the cosmetic appearance of the scalp and difficulty sleeping because of pressure placed on the nodules [3]. The disease has historically been cited as occurring predominantly in young men (aged 18–40 years) of African descent [7], but has recently been shown to occur in other skin phototypes as well [2, 5, 8, 9].
Common treatments for dissecting cellulitis are oral antibiotics (doxycycline, azithromycin, rifampicin), isotretinoin, intralesional triamcinolone acetate, and surgical excision or drainage [4, 10]. Oral antibiotics are often first-line treatment for mild DCS [9]. Isotretinoin is a commonly used treatment for severe DCS, or DCS that is recalcitrant to other therapies such as oral and topical antibiotics [11,12,13,14]. Historically, documented use of isotretinoin for treating DCS has been largely limited to case reports consisting of one or two patients [11,12,13,14]. In the past 5 years, there have been many more multi-patient studies conducted that have used isotretinoin to treat dissecting cellulitis [4, 5, 8, 9, 15]. This literature review analyzes these studies to attempt to determine whether isotretinoin is effective in decreasing the severity of dissecting cellulitis.
2 Methods
2.1 Search Strategies
The following databases were searched for articles prior to 23 June, 2019: PubMed, Embase, Cochrane Central, CINAHL, and Web of Science. Search terms included “Accutane AND dissecting cellulitis”, “Isotretinoin AND dissecting cellulitis,” “Isotretinoin AND perifolliculitis capitis abscedens et suffodiens”, and “Isotretinoin AND primary cicatricial alopecia”. All applicable studies were exported from their respective databases into Endnote for subsequent de-duplication, abstract review, and full-text review. Studies that were ultimately included met criteria for primary articles that detailed the use of isotretinoin to treat dissecting cellulitis. Articles of any age were included.
2.2 Inclusion and Exclusion Criteria
The initial number of articles (six databases) was 369. The number of articles after de-duplication was 164. Inclusion criteria were articles written in English, involve the use of isotretinoin, use in human subjects, and details a dermatologic condition. Exclusion criteria were not a multi-patient study (more than three patients), not a primary research article (e.g., review article, abstract only), does not administer isotretinoin (discussion only), and does not discuss isotretinoin AND dissecting cellulitis.
2.3 Outcome Measure
The primary outcome measure for this meta-analysis was successful improvement of disease after isotretinoin treatment. The definition for treatment success varied among studies, with some studies citing complete resolution of disease while others citing only improvement in disease burden. Therefore, “improvement of disease” was used to standardize the outcome measure across studies. Eligible outcomes included decrease in number of nodules, decrease in inflammation, regrowth of hair, and partial or complete remission of disease. Recurrence was defined as any return of inflammation or nodules after discontinuing isotretinoin.
2.4 Data Extraction
The following study characteristics were collected in Excel: first author; year of publication; study design; years of study; number of patients treated overall; number of patients treated with isotretinoin; location of treatment center; age of patients (mean and range); skin type of patient population; male/female ratio; interventions used (past and present); treatment instructions; dose administered; treatment length; cumulative dosing; follow-up interval; success (%); recurrence (%); family history; associated comorbidities; associated pruritis; associated pain; number of nodules (between one and five); number of nodules (greater than five); bacterial culture results. All study data were compiled and displayed in Table 1. Study authors were contacted about any potential discrepancies in data.
2.5 Data Analysis and Statistical Methods
Overall efficacy of isotretinoin in treating DCS was estimated through a meta-analysis using R package “metafor” from R 3.5.2 [16]. For the purposes of the statistical analysis, efficacy was defined as “any improvement in dissecting cellulitis after use of isotretinoin”.
Cochran’s Q test was used to test heterogeneity among studies. As there was no evidence of heterogeneity, a fixed-effect model was used. Freeman–Tukey (double arcsine) transformation for proportions was used [17]. Sensitivity analysis was performed by estimating the pooled efficacy after excluding one study at a time. Fixed-effect models were also used. Ninety-five percent confidence intervals (CIs) based on the z test were reported for all estimated efficacy. A p value of 0.05 was considered significant.
3 Results
3.1 Selection of Studies
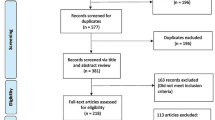
A literature search returned 369 total articles, and 164 articles remained after de-duplication. Abstract and title review showed that of these 164 articles, 48 were case reports with fewer than three patients involved, three were not primary articles (one review article, one poster presentation, one abstract only), 12 merely discussed isotretinoin without administering it, and 92 discussed either isotretinoin or dissecting cellulitis but not both. These articles were excluded. Of the remaining articles, a full-text review revealed one article administered isotretinoin without mentioning treatment results, one article administered isotretinoin but not for dissecting cellulitis, one article administered isotretinoin and rifampicin together, and one article presented with an English abstract but the subsequent article was written in French. The remaining five articles were used for the purposes of this review. Because of unclear wording, two of the included articles had a possibility of administering isotretinoin concomitantly with another treatment [8, 9]. These studies were ultimately included because the possibility of concomitant treatment would have only affected a significant minority of their patient population that received isotretinoin. Reasons for exclusions were detailed in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram (Fig. 1).
3.2 Study Characteristics
The characteristics of the five studies are displayed in Table 1. All five studies were retrospective. The dates of publication were from 2004 to 2018, involving cases from 1995 to 2015. Studies were carried out in China (1), Taiwan (1), France (1), Spain (1), and Canada (1). The number of patients treated with isotretinoin had a range of 4–35. Patient age range was 12–62 years. Three studies listed the mean age of patients with DCS (mean: 26.7 years). The study participants were overwhelmingly male (144/153, 94.1%). Vertex of the scalp was the most commonly recorded location of nodules (range 49–89.4% of patients, mean: 99/138, 71.7%). Two studies cited the percentage of patients that had one to five scalp nodules (62.1% and 71.4%, mean: 56/87, 64.4%) and more than five scalp nodules (37.9% and 28.6%, mean: 31/87, 35.6%). Positive bacterial culture results were reported in three studies (25/42, 59.5%). No other laboratory results were reported in the data.
All studies used isotretinoin after prior use of oral antibiotics. One study mentioned combined use of isotretinoin and prednisolone in a few patients [9]. Isotretinoin dosing varied between studies. Some studies calculated isotretinoin dosing by body weight, between 0.5 and 1 mg/kg/day. One study administered isotretinoin in doses between 40 and 80 mg/day. One study administered 30 mg/day for all patients. Dosing was not defined in one study.
Treatment length range was 1–18 months. After contacting study authors, two studies defined mean treatment duration as 4.2 months and 10 months. One study defined mean treatment duration as 9 months but included other patients without DCS as well. Two studies did not provide values for mean treatment duration. Cumulative dosing was defined in only one study (mean 5731 mg; range 280–19,920 mg). Mean follow-up time was cited in two studies as 6–7 months and 29 months.
3.3 Summary Table of Findings
A summary of the findings is shown in Table 1.
3.4 Efficacy
All five studies documented the percentage of patients that saw improvement of their dissecting cellulitis through use of isotretinoin. In all five studies, an overwhelming majority of patients saw improvement or complete remission of their dissecting cellulitis (75–100%). One study cited complete remission in a majority of patients (33/35, 94.3%) [4]. One study cited both complete remission (6/16, 37.5%) and partial improvement (6/16, 37.5%) in its patients [9]. One study cited reduction in inflammation in a majority of patients (7/8, 88%) [5]. Two studies did not elaborate on improvement [8, 15]. The combined percentage of patients who saw complete remission of disease was 76.5% (39/51). A pooled analysis of the five studies found high efficacy of isotretinoin in improving disease burden in patients with DCS. The overall efficacy of isotretinoin in treating DCS was estimated to be 0.9 with a 95% CI [0.81–0.97]. The study-specific and overall estimated efficacy are shown within the forest plot in Fig. 2. A sensitivity analysis was performed, and suggested that the overall efficacy of isotretinoin was still very high when excluding studies, with a range of 0.83–0.94. If the study with the largest sample size was removed, the estimated efficacy would be as low as 0.83 with a 95% CI (0.67–0.95). The sensitivity analysis is displayed in Table 2.
3.5 Recurrence
Recurrence of dissecting cellulitis after treatment with isotretinoin was noted in four out of five studies. Each of the four studies defined recurrence as occurring after treatment discontinuation. Two of these studies did not give exact values on how many patients experienced recurrence. In the other two studies, the percentage of patients that had recurrences of DCS was 25% and 22.2%, with an overall recurrence of 24% (6/25). One study did not mention if recurrence had occurred or not. One study noted that re-treating dissecting cellulitis after recurrence led to “satisfactory” results [8].
3.6 Associated Manifestations
Four out of five studies cited an associated manifestation of acne conglobata from 14.2 to 44.4% of patients treated. One study cited no associated manifestation of acne conglobata. The total prevalence of acne conglobata was 18.5% (28/151). Two out of five studies cited an associated manifestation of hidradenitis suppurativa (12% and 23.8%). One study cited no associated manifestation of hidradenitis suppurativa, while two studies did not mention an associated manifestation of hidradenitis suppurativa. The total prevalence of hidradenitis suppurativa was 15.3% (11/72). Three studies cited no associated manifestation of pilonidal sinus, while two studies did not mention pilonidal sinus.
Two studies noted associated pruritus in patients (8% and 90%). One study noted associated pruritus in patients but did not give an exact number, while two studies did not mention associated pruritus. The total prevalence of associated pruritus was 31.9% (23/72). Three studies noted associated pain with a range of 25–67% of patients. One study noted associated pain but did not give an exact number. One study did not mention associated pain. The total prevalence of associated pain was 45.9% (61/133).
4 Discussion
4.1 Summary of Evidence
This review found that isotretinoin is a highly effective treatment for providing improvement in dissecting cellulitis. The overall efficacy of isotretinoin for treating dissecting cellulitis was estimated to be 0.9 with a 95% CI (0.81–0.97). A consistently high proportion of patients saw improvement in their disease burden across all five studies, as demonstrated by the sensitivity analysis. Because of the variation in definitions of “efficacy” across studies, further statistical separation of efficacy based on degrees of improvement is not currently possible. However, the true proportion of patients who see a complete remission of disease after treatment should be significant, as two studies clearly defined a pool of patients as having “complete remission of disease”, which would represent 54.16% (39/72) of patients included in these studies [4, 9]. While all studies reported prior use of antibiotics, one study included patients who did not respond to multiple prior treatments including antibiotics and oral corticosteroids [4]. The patients within this study may have had more severe disease. This did not seem to affect treatment response, as the patients in this study had a high percentage of “complete remission” (33/35, 92%). While there exists the possibility of concomitant therapy in a minority of patients in two studies, this did not correlate with treatment response as high rates of improvement were found in studies both with and without potential concomitant therapy [8, 9]. Future studies can improve the body of evidence by defining degrees of improvement, as well as comparing treatment with isotretinoin vs placebo or other treatments. Dosing varied throughout the five studies. However, the study with the most treatment success (33/35 patients had complete remission) used a dosage of 0.5–0.8 mg/kg/day with an average treatment length of 3 months [4]. Treatment length and cumulative dose should be recorded to see if there is a positive correlation with treatment response. While four out of five papers included average dosing, mean duration of treatment was reported in only two studies [4, 9]. Cumulative dosing average was cited in one study [9]. Without one of these two variables, it is difficult to accurately calculate whether the cumulative amount of isotretinoin administered correlates to better treatment outcomes. This information could greatly aid in standardizing current isotretinoin treatment guidelines for patients with DCS.
Study results suggest that recurrence is a commonly expected outcome after successful treatment of isotretinoin for dissecting cellulitis. Recurrence was noted in four out of five studies, although exact numbers were provided in only two studies (6/25, 24%). Retreatment with isotretinoin after recurrence seems to be a satisfactory option [8]. Recurrence of disease is also a commonly reported outcome across other treatment options such as oral antibiotics [4, 18]. Isotretinoin has been hypothesized to offer a longer duration of remission before disease recurrence [9]. Because of the lack of reporting of cumulative doses, it is not possible at this time to draw conclusions on whether higher cumulative doses can result in decreased recurrence. Maintenance therapy with 0.75–1 mg/kg/day has been described as a satisfactory option to combat the high recurrence rates associated with DCS [19]. Future studies should also explore whether lower dosages of less than 0.5 mg/kg/day can be an effective option in reducing recurrence rates while minimizing potential side effects.
4.2 Associated Manifestations
Associated pain (61/133, 45.9%) and pruritus (23/72, 31.9%) were frequently documented symptoms, and are likely due to the inflammatory pathogenesis of DCS. Additionally, the mean age of onset (26.7 years), the predominance of nodules on the vertex of the scalp (99/138, 71.7%), and the overwhelmingly male patient population are consistent with what is described in the literature [4, 10]. Multiple scalp nodules are common, with over one-third of cited patients having more than five nodules (31/87, 35.6%). There was frequent mention of the associated manifestations of acne conglobata (30/151, 19.9%) and hidradenitis suppurativa (11/72, 18.5%), which are frequently described in the literature as part of the follicular tetrad along with dissecting cellulitis. These data show that these two diseases can occur concurrently with DCS. There was no mention of pilonidal cysts, with three studies explicitly mentioning that no patients had associated pilonidal cysts. This suggests that although DCS and pilonidal cysts are both parts of the follicular tetrad, they are not often found concurrently with each other. Bacterial cultures were commonly positive when reported (25/42, 59.5%). When positive, cultures grew coagulase-negative staphylococci, Staphylococcus aureus, Staphylococcus epidermidis, Enterobacter aerogenes, or mixed bacteria.
4.3 Limitations
The strengths of this study include the use of a comprehensive search strategy across five databases and the statistical analysis. The findings from this study are generalizable because the studies reported results from five different countries across three continents. This study has limitations owing to the low quality of study designs in the available literature. These include the lack of a control group to compare with isotretinoin, small study sizes, varied outcome measures, inconsistent dosages across studies, and reliance on observational studies instead of randomized controlled trials to analyze treatment efficacy. Future studies are required to answer whether isotretinoin is more effective than other common treatments for DCS. Inclusion of specific definitions for clinical improvement, dosage regimens, and recurrence rates would lead to more impactful conclusions to inform clinical practice. Use of prospective studies and larger sample sizes would help increase the quality of knowledge on treatments for dissecting cellulitis.
4.4 Implications for Practice
The findings from this review reveal that isotretinoin can be very effective as monotherapy for significant improvement or complete recovery of dissecting cellulitis. Oral antibiotics may still be considered as first-line therapy for less severe cases of dissecting cellulitis owing to their milder side-effect profile [9]. Recurrence after successful treatment of dissecting cellulitis is common, and subsequent retreatment with isotretinoin has been documented in the literature as successful [9]. Continued maintenance therapy with isotretinoin may help decrease the rate of recurrence [19]. The average dosing requirement amongst these five studies was 0.5–0.75 mg/kg/day for a minimum of 3 months.
4.5 Treatment Alternatives
There is no well-established treatment for dissecting cellulitis that is refractory to antibiotics and isotretinoin [10]. Surgical excision of sinus tracts can be done but is very destructive [20].
Tumor necrosis factor-α inhibitors, adalimumab and infliximab, have been detailed in case studies to be effective in improving DCS [21,22,23,24,25,26]. One case report notes that of the 14 patients who have been described in case reports (as of 4 July, 2019), 85.7% (12/14) saw an improvement in inflammatory skin symptoms of DCS. After not responding to treatment with isotretinoin, 71.4% (10/14) were administered tumor necrosis factor-α inhibitors [21]. The most common dosage used for adalimumab was an 80-mg loading dose with a 40-mg dose every other week thereafter, while the most common dosage used for infliximab was 5 mg/kg at 8-week intervals [21]. Complete remission was seen in three patients [23, 26, 27]. One study noted that in two out of three patients, inflammatory infiltrate was reduced but the underlying subcutaneous sinus tract structure stayed unchanged, and one patient relapsed 4 weeks after cessation of treatment [24]. It seems that while tumor necrosis factor-α inhibitors may be effective in improving DCS in patients who have not responded to or who cannot take isotretinoin, it may not be a curative option. Biologic agents are known to only suppress the underlying inflammatory process, and upon cessation would likely lead to disease relapse.
There have been three recent case studies detailing the use of multiple sessions of 10% aminolevulinic acid during photodynamic therapy (ALA-PDT) laser treatment as an alternative to isotretinoin [28,29,30]. These studies have cited significant improvement or complete remission in patients with DCS at an efficacy comparable to isotretinoin [28,29,30]. No recurrence was cited in two studies (follow-up at 7 weeks [30] and 3 months [28]). Treatment with 10% ALA-PDT may also be a safe alternative for dissecting cellulitis that is refractory to isotretinoin, patients who have adverse effects from using isotretinoin (acne fulminans [31], pseudotumor cerebri [32], hepatotoxicity [33]), alcoholics [33], or pregnant women [34]. It is also an attractive option in that it may offer a lower rate of recurrence than isotretinoin [28, 30]. However, more data are needed.
5 Conclusions
Isotretinoin is a highly effective treatment for improving symptoms of dissecting cellulitis of the scalp. Disease recurrence is a common finding for those who undergo successful treatment, and subsequent retreatment with isotretinoin is an option. It will be important for future studies to document follow-ups, duration of treatment, average dosing, and average cumulative dose to draw conclusions on clinical dosing guidelines.
References
Brănişteanu DE, Molodoi A, Ciobanu D, et al. The importance of histopathologic aspects in the diagnosis of dissecting cellulitis of the scalp. Rom J Morphol Embryol. 2009;50:719–24.
Vasanth V, Chandrashekar B. Follicular occlusion tetrad. Indian Dermatol Online J. 2014;5:491. https://doi.org/10.4103/2229-5178.142517.
Jerome MA, Laub DR. Dissecting cellulitis of the scalp: case discussion, unique considerations, and treatment options. Eplasty. 2014;14:ic17.
Badaoui A, Reygagne P, Cavelier-Balloy B, et al. Dissecting cellulitis of the scalp: a retrospective study of 51 patients and review of literature. Br J Dermatol. 2016;174:421–3. https://doi.org/10.1111/bjd.13999.
Segurado-Miravalles G, Camacho-Martínez FM, Arias-Santiago S, et al. Epidemiology, clinical presentation and therapeutic approach in a multicentre series of dissecting cellulitis of the scalp. J Eur Acad Dermatol Venereol. 2017;31:e199-200. https://doi.org/10.1111/jdv.13948.
Sperling LC. Scarring alopecia and the dermatopathologist. J Cutan Pathol. 2001;28:333–42.
Scott DA. Disorders of the hair and scalp in blacks. Dermatol Clin. 1988;6:387–95.
Zhang X, Qi S, Zhao Y, et al. Clinical features of primary cicatricial alopecia in Chinese patients. Indian J Dermatol Venereol Leprol. 2014;80:306. https://doi.org/10.4103/0378-6323.136833.
Lee C-N, Chen W, Hsu C-K, et al. Dissecting folliculitis (dissecting cellulitis) of the scalp: a 66-patient case series and proposal of classification. J Dtsch Dermatol Ges. 2018;16:1219–26. https://doi.org/10.1111/ddg.13649.
Scheinfeld N. Dissecting cellulitis (perifolliculitis capitis abscedens et suffodiens): a comprehensive review focusing on new treatments and findings of the last decade with commentary comparing the therapies and causes of dissecting cellulitis to hidradenitis suppurativa. Dermatol Online J. 2014;20:22692.
Berne B, Venge P, Ohman S. Perifolliculitis capitis abscedens et suffodiens (Hoffman): complete healing associated with oral zinc therapy. Arch Dermatol. 1985;121:1028–30.
Benvenuto ME, Rebora A. Fluctuant nodules and alopecia of the scalp: perifolliculitis capitis abscedens et suffodiens. Arch Dermatol. 1992;128(1115–7):1118–9. https://doi.org/10.1001/archderm.128.8.1115b.
Stites PC, Boyd AS. Dissecting cellulitis in a white male: a case report and review of the literature. Cutis. 2001;67:37–40.
Schewach-Millet M, Ziv R, Shapira D. Perifolliculitis capitis abscedens et suffodiens treated with isotretinoin (13-cis-retinoic acid). J Am Acad Dermatol. 1986;15:1291–2. https://doi.org/10.1016/s0190-9622(86)80042-1.
Tan E, Martinka M, Ball N, Shapiro J. Primary cicatricial alopecias: clinicopathology of 112 cases. J Am Acad Dermatol. 2004;50:25–32. https://doi.org/10.1016/j.jaad.2003.04.001.
R. The R Project for statistical computing. https://www.r-project.org/. Accessed 8 Oct 2019.
Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21:607–11. https://doi.org/10.1214/aoms/1177729756.
Greenblatt DT, Sheth N, Teixeira F. Dissecting cellulitis of the scalp responding to oral quinolones. Clin Exp Dermatol. 2008;33:99–100. https://doi.org/10.1111/j.1365-2230.2007.02598.x.
Khaled A, Zeglaoui F, Zoghlami A, et al. Dissecting cellulitis of the scalp: response to isotretinoin. J Eur Acad Dermatol Venereol. 2007;21:1430–1.
Bellew SG, Nemerofsky R, Schwartz RA, Granick MS. Successful treatment of recalcitrant dissecting cellulitis of the scalp with complete scalp excision and split-thickness skin graft. Dermatol Surg. 2003;29:1068–70.
Takahashi T, Yamasaki K, Terui H, et al. Perifolliculitis capitis abscedens et suffodiens treatment with tumor necrosis factor inhibitors: a case report and review of published cases. J Dermatol. 2019;46:802–7. https://doi.org/10.1111/1346-8138.14998.
Mansouri Y, Martin-Clavijo A, Newsome P, Kaur MR. Dissecting cellulitis of the scalp treated with tumour necrosis factor-α inhibitors: experience with two agents. Br J Dermatol. 2016;174:916–8. https://doi.org/10.1111/bjd.14269.
Brandt HRC, Malheiros APR, Teixeira MG, Machado MCR. Perifolliculitis capitis abscedens et suffodiens successfully controlled with infliximab. Br J Dermatol. 2008;159:506–7. https://doi.org/10.1111/j.1365-2133.2008.08674.x.
Navarini AA, Trüeb RM. 3 cases of dissecting cellulitis of the scalp treated with adalimumab. Arch Dermatol. 2010;146:517–20. https://doi.org/10.1001/archdermatol.2010.16.
Wollina U, Gemmeke A, Koch A. Dissecting cellulitis of the scalp responding to intravenous tumor necrosis factor-alpha antagonist. J Clin Aesthet Dermatol. 2012;5:36–9.
Sand FL, Thomsen SF. Off-label use of TNF-alpha inhibitors in a dermatological university department: retrospective evaluation of 118 patients. Dermatol Ther. 2015;28:158–65. https://doi.org/10.1111/dth.12222.
Martin-García RF, Rullán JM. Refractory dissecting cellulitis of the scalp successfully controlled with adalimumab. P R Health Sci J. 2015;34:102–4.
Feng Y, Zhang Y, Guo H, et al. Treatment of dissecting cellulitis of the scalp with 10% ALA-PDT. Lasers Surg Med. 2019;51:332–8. https://doi.org/10.1002/lsm.23016.
Zhan Y, Chen X, Zhou Y, et al. Dissecting cellulitis of the scalp successfully treated with ALA-PDT: case report. Photodiagn Photodyn Ther. 2018;24:182–4. https://doi.org/10.1016/j.pdpdt.2018.10.001.
Liu Y, Ma Y, Xiang L-H. Successful treatment of recalcitrant dissecting cellulitis of the scalp with ALA-PDT: case report and literature review. Photodiagn Photodyn Ther. 2013;10:410–3. https://doi.org/10.1016/j.pdpdt.2013.03.008.
Li AW, Antaya RJ. Isotretinoin-induced acne fulminans without systemic symptoms with concurrent exuberant granulation tissue. Pediatr Dermatol. 2018;35:257–8. https://doi.org/10.1111/pde.13389.
Varoglu AO, Aksoy A. Herpes simplex encephalitis and pseudotumour cerebri due to isotretinoin. J Pak Med Assoc. 2018;68:1833–5.
Brelsford M, Beute TC. Preventing and managing the side effects of isotretinoin. Semin Cutan Med Surg. 2008;27:197–206. https://doi.org/10.1016/j.sder.2008.07.002.
Centers for Disease Control and Prevention (CDC). Accutane-exposed pregnancies: California, 1999. MMWR Morb Mortal Wkly Rep. 2000;49:28–31.
Acknowledgements
We acknowledge the biostatistical consultation and support provided by Dr. Jie Yang and the Biostatistical Consulting Core at the School of Medicine, Stony Brook University.
Author information
Authors and Affiliations
Contributions
Study conception was performed by WG and DS. Study methodology and design were performed by WG and GS. Study data curation and literature search was performed by WG. Formal analysis was performed by CZ. Study supervision and mentorship was provided by DS. The first draft of the manuscript was written by WG and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflicts of Interest/Competing Interests
William Guo, Chencan Zhu, Gregg Stevens, and David Silverstein have no conflicts of interest that are directly relevant to the content of this article.
Ethical approval
The study conducted was in accordance with the ethical standards of the 1964 Helsinki declaration and subsequent amendments.
Availability of Data and Material
Not applicable.
Code availability
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Guo, W., Zhu, C., Stevens, G. et al. Analyzing the Efficacy of Isotretinoin in Treating Dissecting Cellulitis: A Literature Review and Meta-Analysis. Drugs R D 21, 29–37 (2021). https://doi.org/10.1007/s40268-020-00335-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-020-00335-y