Abstract
This study examined the role of autonomy support from adults’ informal health supporters (family or friends) in diabetes-specific health behaviors and health outcomes. Using baseline data from 239 Veterans with type 2 diabetes at risk of complications enrolled in behavioral trial, we examined associations between autonomy support from a support person and that support person’s co-residence with the participant’s diabetes self-care activities, patient activation, cardiometabolic measures, and predicted risk of a cardiac event. Autonomy support from supporters was associated with significantly increased adherence to healthy lifestyle behaviors (diet, p < .001 and exercise, p = .003); higher patient activation (p < .001); greater patient efficacy in interacting with healthcare providers, and lower 5-year (p = .044) and 10-year (p = .027) predicted cardiac risk. Autonomy support was not significantly associated with diabetes-specific behaviors (checking blood glucose, foot care, or medication taking); or hemoglobin A1c, systolic blood pressure, or non-HDL cholesterol. There was a significant interaction of autonomy support and supporter residence in one model such that lack of autonomy support was associated with lower patient activation only among individuals with in-home supporters. No other interactions were significant. Findings suggest that autonomy support from family and friends may play a role in patient self-management, patient activation, and lower cardiac risk.

Similar content being viewed by others
References
Aikens, J. E., Rosland, A. M., & Piette, J. D. (2015a). Improvements in illness self-management and psychological distress associated with telemonitoring support for adults with diabetes. Primary Care Diabetes, 9, 127–134.
Aikens, J. E., Trivedi, R., Aron, D. C., & Piette, J. D. (2015b). Integrating support persons into diabetes telemonitoring to improve self-management and medication adherence. Journal of General Internal Medicine, 30, 319–326.
Aikens, J. E., Zivin, K., Trivedi, R., & Piette, J. D. (2014). Diabetes self-management support using mHealth and enhanced informal caregiving. Journal of Diabetes and Its Complications, 28, 171–176.
Baker, A. C., Wiebe, D. J., Kelly, C. S., Munion, A., Butner, J. E., Swinyard, M. T., et al. (2019). Structural model of patient-centered communication and diabetes management in early emerging adults at the transfer to adult care. Journal of Behavioral Medicine, 42, 831–841.
Beck, J., Greenwood, D. A., Blanton, L., Bollinger, S. T., Butcher, M. K., Condon, J. E., et al. (2017). National standards for diabetes self-management education and support. The Diabetes Educator, 43, 449–464.
Berg, C. A., Helgeson, V. S., Tracy, E. L., Butner, J. E., Kelly, C. S., Van Vleet, M., & Litchman, M. L. (2020). Daily illness appraisal and collaboration in couples with type 1 diabetes. Health Psychology.
Blaum, C. S., Cigolle, C. T., Boyd, C., Wolff, J. L., Tian, Z., Langa, K. M., et al. (2010). Clinical complexity in middle-aged and older adults with diabetes: The Health and Retirement Study. Medical Care, 48, 327.
Center for Disease Control and Prevention. (2018). Data and Statistics. Retrieved from https://www.cdc.gov/diabetes/data/
Chang, H. Y., Weiner, J. P., Richards, T. M., Bleich, S. N., & Segal, J. B. (2012). Predicting costs with diabetes complications severity index in claims data. The American Journal of Managed Care, 18, 213–219.
Chao, S. Y., Zarzabal, L. A., Walker, S. M., Herzog, C. M., Eilerman, P. A., Luce, B. K., et al. (2013). Estimating diabetes prevalence in the military health system population from 2006 to 2010. Military Medicine, 178, 986–993.
Corp, Stata. (2017). Stata Statistical Software: Release 15. College Station, TX: StataCorp LP.
Einarson, T. R., Acs, A., Ludwig, C., & Panton, U. H. (2018). Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovascular Diabetology, 17, 83.
Fields, B., Makaroun, L., Rodriguez, K. L., Robinson, C., Forman, J., & Rosland, A.-M. (2020). Caregiver role development in chronic disease: A qualitative study of informal caregiving for veterans with diabetes. Chronic Illness.
Graffigna, G., Barello, S., Bonanomi, A., & Menichetti, J. (2016). The motivating function of healthcare professional in eHealth and mHealth interventions for type 2 diabetes patients and the mediating role of patient engagement. Journal of Diabetes Research, 2016, 1–10.
Gregg, E. W., Beckles, G., Williamson, D. F., Leveille, S. G., Langlois, J. A., Engelgau, M. M., et al. (2000). Diabetes and physical disability among older US adults. Diabetes Care, 23, 1272–1277.
Harding, J. L., Pavkov, M. E., Magliano, D. J., Shaw, J. E., & Gregg, E. W. (2019). Global trends in diabetes complications: A review of current evidence. Diabetologia, 62, 3–16.
Helgeson, V. S., Berg, C. A., Kelly, C. S., Van Vleet, M., Zajdel, M., Tracy, E. L., et al. (2019). Patient and partner illness appraisals and health among adults with type 1 diabetes. Journal of Behavioral Medicine, 42, 480–492.
Hibbard, J. H., Mahoney, E. R., Stockard, J., & Tusler, M. (2005). Development and testing of a short form of the Patient Activation Measure. Health Services Research, 40, 1918–1930.
Janevic, M., Piette, J., Ratz, D., Kim, H., & Rosland, A. M. (2016). Correlates of family involvement before and during medical visits among older adults with high-risk diabetes. Diabetic Medicine, 33, 1140–1148.
Julien, E., Senécal, C., & Guay, F. (2009). Longitudinal relations among perceived autonomy support from health care practitioners, motivation, coping strategies and dietary compliance in a sample of adults with type 2 diabetes. Journal of Health Psychology, 14, 457–470.
Koponen, A. M., Simonsen, N., & Suominen, S. (2017). Determinants of physical activity among patients with type 2 diabetes: The role of perceived autonomy support, autonomous motivation and self-care competence. Psychology, Health & Medicine, 22, 332–344.
Ladhani, N., Majumdar, S., Johnson, J., Tsuyuki, R., Lewanczuk, R., Spooner, R., et al. (2012). Adding pharmacists to primary care teams reduces predicted long-term risk of cardiovascular events in Type 2 diabetic patients without established cardiovascular disease: Results from a randomized trial. Diabetic Medicine, 29, 1433–1439.
Lee, A. A., Piette, J., Heisler, M., Janevic, M. R., Langa, K. M., & Rosland, A. M. (2017). Family members experinces supporting adults with chronic illness: A national survey. Families, Systems, & Health, 35, 463–473.
Lee, A. A., Piette, J., Heisler, M., Janevic, M. R., & Rosland, A. (2019). Diabetes self-management and glycemic control: The role of autonomy support from informal health supporters. Health Psychology, 38, 122–132.
Lee, A. A., Piette, J. D., Heisler, M., & Rosland, A. M. (2018). Diabetes distress and glycemic control: The buffering effect of autonomy support from important family members and friends. Diabetes Care, 41, 1157–1163.
Little, R. R. (2003). Glycated hemoglobin standardization–National Glycohemoglobin Standardization Program (NGSP) perspective. Clinical Chemistry and Laboratory Medicine, 41, 1191–1198.
Liu, Y., Sayam, S., Shao, X., Wang, K., Zheng, S., Li, Y., et al. (2017). Peer reviewed: Prevalence of and trends in diabetes among Veterans, United States, 2005–2014. Preventing Chronic Disease. https://doi.org/10.5888/pcd14.170230
Maly, R. C., Frank, J. C., Marshall, G. N., DiMatteo, M. R., & Reuben, D. B. (1998). Perceived efficacy in patient-physician interactions (PEPPI): Validation of an instrument in older persons. Journal of the American Geriatrics Society, 46, 889–894.
Morrish, N., Wang, S. L., Stevens, L., Fuller, J., Keen, H., & Group, W. M. S. (2001). Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia, 44, S14.
Nouwen, A., Ford, T., Balan, A. T., Twisk, J., Ruggiero, L., & White, D. (2011). Longitudinal motivational predictors of dietary self-care and diabetes control in adults with newly diagnosed type 2 diabetes mellitus. Health Psychology, 30, 771–779.
Peter, M., Oostveen, J. C., Zandbelt, L. C., Taal, E., Drossaert, C. H., Harmsen, E. J., et al. (2012). Further validation of the 5-item Perceived Efficacy in Patient-Physician Interactions (PEPPI-5) scale in patients with osteoarthritis. Patient Education and Counseling, 87, 125–130.
Piette, J. D., Rosland, A. M., Silveira, M., Kabeto, M., & Langa, K. M. (2010). The case for involving adult children outside of the household in the self-management support of older adults with chronic illnesses. Chronic Illness, 6, 34–45.
Raaijmakers, L. G., Martens, M. K., Bagchus, C., de Weerdt, I., de Vries, N. K., & Kremers, S. P. (2015). Correlates of perceived self-care activities and diabetes control among Dutch type 1 and type 2 diabetics. Journal of Behavioral Medicine, 38, 450–459.
Remmers, C., Hibbard, J., Mosen, D. M., Wagenfield, M., Hoye, R. E., & Jones, C. (2009). Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? The Journal of Ambulatory Care Management, 32, 320–327.
Rosland, A. M., Heisler, M., Choi, H. J., Silveira, M. J., & Piette, J. D. (2010). Family influences on self-management among functionally independent adults with diabetes or heart failure: Do family members hinder as much as they help? Chronic Illness, 6, 22–33.
Rosland, A.-M., Heisler, M., Janevic, M. R., Connell, C. M., Langa, K. M., Kerr, E. A., et al. (2013). Current and potential support for chronic disease management in the United States: The perspective of family and friends of chronically ill adults. Families, Systems, & Health, 31, 119.
Rosland, A. M., Piette, J. D., Lyles, C. R., Parker, M. M., Moffet, H. H., Adler, N. E., et al. (2014). Social support and lifestyle vs. medical diabetes self-management in the Diabetes Study of Northern California (DISTANCE). Annals of Behavioral Medicine, 48, 438–447.
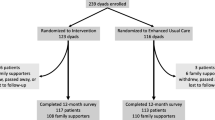
Rosland, A. M., Piette, J. D., Trivedi, R., Kerr, E. A., Stoll, S., Tremblay, A., et al. (2018). Engaging family supporters of adult patients with diabetes to improve clinical and patient-centered outcomes: Study protocol for a randomized controlled trial. Trials, 19, 394.
Shrivastava, S. R., Shrivastava, P. S., & Ramasamy, J. (2013). Role of self-care in management of diabetes mellitus. Journal of Diabetes & Metabolic Disorders, 12, 1–5.
Silliman, R. A., Bhatti, S., Khan, A., Dukes, K. A., & Sullivan, L. M. (1996). The care of older persons with diabetes mellitus: Families and primary care physicians. Journal of the American Geriatrics Society, 44, 1314–1321.
Singh, G. M., Danaei, G., Pelizzari, P. M., Lin, J. K., Cowan, M. J., Stevens, G. A., et al. (2012). The age associations of blood pressure, cholesterol, and glucose: analysis of health examination surveys from international populations. Circulation, 125, 2204–2211.
Song, Y., Nam, S., Park, S., Shin, I.-S., & Ku, B. J. (2017). The impact of social support on self-care of patients with diabetes: What is the effect of diabetes type? Systematic review and meta-analysis. The Diabetes Educator, 43, 396–412.
Stevens, R. J., Kothari, V., Adler, A. I., Stratton, I. M., & Holman, R. R. (2001). The UKPDS risk engine: A model for the risk of coronary heart disease in Type II diabetes (UKPDS 56). Clinical Science, 101, 671–679.
Su, Y.-L., & Reeve, J. (2011). A meta-analysis of the effectiveness of intervention programs designed to support autonomy. Educational Psychology Review, 23, 159–188.
Tinetti, M. E., & Studenski, S. A. (2011). Comparative effectiveness research and patients with multiple chronic conditions. The New England Journal of Medicine, 364, 2478–2481.
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23, 943–950.
Van Dieren, S., Beulens, J., Kengne, A., Peelen, L., Rutten, G., Woodward, M., et al. (2012). Prediction models for the risk of cardiovascular disease in patients with type 2 diabetes: A systematic review. Heart, 98, 360–369.
Von Korff, M., Katon, W., Lin, E. H., Simon, G., Ciechanowski, P., Ludman, E., et al. (2005). Work disability among individuals with diabetes. Diabetes Care, 28, 1326–1332.
Wallston, K. A., Rothman, R. L., & Cherrington, A. (2007). Psychometric properties of the perceived diabetes self-management scale (PDSMS). Journal of Behavioral Medicine, 30, 395–401.
Webb, D., Khunti, K., Gray, L., Srinivasan, B., Farooqi, A., Wareham, N., et al. (2012). Intensive multifactorial intervention improves modelled coronary heart disease risk in screen-detected Type 2 diabetes mellitus: A cluster randomized controlled trial. Diabetic Medicine, 29, 531–540.
Williams, G. C., Freedman, Z. R., & Deci, E. L. (1998). Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care, 21, 1644–1651.
Williams, G. C., Lynch, M., & Glasgow, R. E. (2007). Computer-assisted intervention improves patient-centered diabetes care by increasing autonomy support. Health Psychology, 26, 728–734.
Williams, G. C., Lynch, M. F., McGregor, H. A., Ryan, R. M., Sharp, D., & Deci, E. L. (2006). Validation of the” Important Other” Climate Questionnaire: Assessing autonomy support for health-related change. Families, Systems, & Health, 24, 179–194.
Williams, G. C., McGregor, H. A., Zeldman, A., Freedman, Z. R., & Deci, E. L. (2004). Testing a self-determination theory process model for promoting glycemic control through diabetes self-management. Health Psychology, 23, 58–66.
Williams, G. C., Patrick, H., Niemiec, C. P., Williams, L. K., Divine, G., Lafata, J. E., et al. (2009). Reducing the health risks of diabetes: How self-determination theory may help improve medication adherence and quality of life. The Diabetes Educator, 35, 484–492.
Young, B. A., Lin, E., Von Korff, M., Simon, G., Ciechanowski, P., Ludman, E. J., et al. (2008). Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. The American Journal of Managed Care, 14, 15–24.
Zimbudzi, E., Lo, C., Ranasinha, S., Kerr, P. G., Polkinghorne, K. R., Teede, H., et al. (2017). The association between patient activation and self-care practices: A cross-sectional study of an Australian population with comorbid diabetes and chronic kidney disease. Health Expectations, 20, 1375–1384.
Zoffmann, V., & Lauritzen, T. (2006). Guided self-determination improves life skills with type 1 diabetes and A1C in randomized controlled trial. Patient Education and Counseling, 64(1), 78–86.
Funding
This work was supported by the Veterans Administration Health Services Research and Development IIR 14–074-1, the Michigan Center for Diabetes Translational Research (National Institutes of Health (NIH) Grant 5P60- DK09292), and the Michigan Claude D. Pepper Older Americans Independence Center (NIH Grant AG-024824). The funder did not and will not have any role in the study design; collection, management, analysis, and interpretation of data; writing of this report; or decision to submit this report for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Aaron A. Lee declare that he has no conflict of interest, Michele Heisler declare that she has no conflict of interest, Ranak Trivedi declare that she has no conflict of interest, Patric Leukel declare that he has no conflict of interest, Maria K. Mor declare that she has no conflict of interest, and Ann-Marie Rosland declare that she has no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, A.A., Heisler, M., Trivedi, R. et al. Autonomy support from informal health supporters: links with self-care activities, healthcare engagement, metabolic outcomes, and cardiac risk among Veterans with type 2 diabetes. J Behav Med 44, 241–252 (2021). https://doi.org/10.1007/s10865-020-00196-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-020-00196-5