Abstract
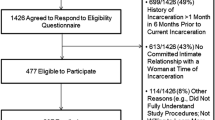
Black men who have sex with men (MSM) engaged in sex work (BMSM-SW) experience elevated HIV and sexually transmitted infection (STI) prevalence. Further, BMSM-SW have been shown to have higher rates of syndemic psychosocial health conditions which contribute to HIV risk behavior and incidence, and poorer care outcomes than other groups of men who have sex with men. However, syndemic perspectives have not been applied to understanding past-year STI burden among BMSM-SW in the U.S. Sexually active Black MSM ≥ 18 years old were recruited from Black Pride events in six U.S. cities (n = 4421) between 2014 and 2017. Multivariable logistic regressions assessed correlates of past-year sex work engagement; whether BMSM-SW had higher odds of syndemic conditions; and whether BMSM-SW had higher odds of self-reported, past-year STI diagnoses. Structural equation models assessed relationships between sex work engagement, syndemic conditions, and STI controlled for sociodemographics and number of sexual partners. A total of 254 (5.7%) Black MSM reported past-year sex work, of whom 45.3% were HIV positive. BMSM-SW were significantly more likely to be Hispanic, to report past-year bisexual behavior, and to report annual income < $10,000. In multivariable models, BMSM-SW were significantly more likely to report intimate partner violence, assault victimization, polydrug use, and depression symptoms; they were also more likely to report past-year gonorrhea, chlamydia, and syphilis. Syndemic conditions mediated the relationship between past-year sex work and past-year STI burden, constituting a significant indirect effect. BMSM-SW in the U.S. face severe biopsychosocial health disparities. Interventions developed for BMSM engaged in sex work are lacking. Our results suggest that interventions containing safer sex work education and sex-positive biobehavioral HIV/STI prevention alongside substance use, mental health, employment, and education components will be most effective.

Similar content being viewed by others
References
Andresen, E. M., Malmgren, J. A., Carter, W. B., & Patrick, D. L. (1994). Screening for depression in well older adults: Evaluation of a short form of the CES-D. American Journal of Preventive Medicine, 10(2), 77–84.
Balaji, A. B., Bowles, K. E., Hess, K. L., Smith, J. C., Paz-Bailey, G., & Group, N. S. (2017). Association between enacted stigma and HIV-related risk behavior among MSM, National HIV Behavioral Surveillance System, 2011. AIDS and Behavior, 21(1), 227–237.
Baral, S. D., Friedman, M. R., Geibel, S., Rebe, K., Bozhinov, B., Diouf, D., … Cáceres, C. F. (2015). Male sex workers: Practices, contexts, and vulnerabilities for HIV acquisition and transmission. The Lancet, 385(9964), 260–273.
Bauermeister, J. A., Eaton, L., Meanley, S., Pingel, E. S., & Partnership, U. (2017). Transactional sex with regular and casual partners among young men who have sex with men in the Detroit metro area. American Journal of Men’s Health, 11(3), 498–507.
Bauermeister, J. A., Eaton, L., & Stephenson, R. (2016). A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among young men who have sex with men living in metro Detroit. Behavioral Medicine, 42(3), 197–204.
Biello, K. B., Colby, D., Closson, E., & Mimiaga, M. J. (2014). The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City, Vietnam. AIDS and Behavior, 18(7), 1264–1271.
Biello, K. B., Oldenburg, C. E., Mitty, J. A., Closson, E. F., Mayer, K. H., Safren, S. A., & Mimiaga, M. J. (2017). The “Safe Sex” conundrum: Anticipated stigma from sexual partners as a barrier to PrEP use among substance using MSM engaging in transactional sex. AIDS and Behavior, 21(1), 300–306.
Bobashev, G. V., Zule, W. A., Osilla, K. C., Kline, T. L., & Wechsberg, W. M. (2009). Transactional sex among men and women in the south at high risk for HIV and other STIs. Journal of Urban Health, 86(1), 32–47.
Bukowski, L. A., Chandler, C. J., Creasy, S. L., Matthews, D. D., Friedman, M. R., & Stall, R. D. (2018). Characterizing the HIV care continuum and identifying barriers and facilitators to HIV diagnosis and viral suppression among black transgender women in the United States. Journal of Acquired Immune Deficiency Syndromes, 79(4), 413–420.
Crosby, R. A., & Mena, L. (2017). Correlates of enhanced sexual pleasure from condom use: A study of young black men who have sex with men in the United States. AIDS and Behavior, 21(5), 1491–1496.
Dilley, J., McFarland, W., & Kellogg, T. (2000). Use of a unique testing code among anonymous testers to track repeat tests, estimate HIV incidence, and identify risk factors for HIV seroconversion [Abstract MoPpD1132]. Paper presented at the International AIDS Conference, Durban, South Africa.
dos Ramos Farías, M. S., Garcia, M. N., Reynaga, E., Romero, M., Vaulet, M. L. G., Fermepín, M. R., … González, J. V. (2011). First report on sexually transmitted infections among trans (male to female transvestites, transsexuals, or transgender) and male sex workers in Argentina: High HIV, HPV, HBV, and syphilis prevalence. International Journal of Infectious Diseases, 15(9), e635–e640.
Dyer, T. P., Shoptaw, S., Guadamuz, T. E., Plankey, M., Kao, U., Ostrow, D., … Stall, R. (2012). Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. Journal of Urban Health, 89(4), 697–708.
Dyer, T. V., Turpin, R. E., Stall, R., Khan, M. R., Nelson, L. E., Brewer, R., … Mayer, K. H. (2020). Latent profile analysis of a syndemic of vulnerability factors on incident sexually transmitted infection in a cohort of black men who have sex with men only and black men who have sex with men and women in the HIV prevention trials network 061 study. Sexually Transmitted Diseases, 47(9), 571–579.
Eaton, L. A., Matthews, D. D., Driffin, D. D., Bukowski, L., Wilson, P. A., Stall, R. D., & POWER Study Team. (2017). A multi-US city assessment of awareness and uptake of pre-exposure prophylaxis (PrEP) for HIV prevention among Black men and transgender women who have sex with men. Prevention Science, 18(5), 505–516.
Edeza, A., Galárraga, O., Santamaria, E. K., Sosa-Rubí, S., Operario, D., & Biello, K. B. (2020). “I do try to use condoms, but…”: knowledge and interest in PrEP among male sex workers in Mexico City. Archives of Sexual Behavior, 49(1), 355–363.
Farmer, P. (2001). Infections and inequalities: The modern plagues. Berkeley: University of California Press.
Friedman, M. R., Bukowski, L., Eaton, L. A., Matthews, D. D., Dyer, T. V., Siconolfi, D., & Stall, R. (2019). Psychosocial health disparities among black bisexual men in the U.S.: Effects of sexuality nondisclosure and gay community support. Archives of Sexual Behavior, 48(1), 213–224.
Friedman, M. R., Sang, J. M., Bukowski, L. A., Matthews, D. D., Eaton, L. A., Raymond, H. F., & Stall, R. (2018). HIV care continuum disparities Among black bisexual Men and the mediating effect of psychosocial comorbidities. Journal of Acquired Immune Deficiency Syndromes, 77(5), 451–458.
Guadamuz, T. E., Friedman, M. S., Marshal, M. P., Herrick, A. L., Lim, S. H., Wei, C., & Stall, R. (2013). Health, sexual health, and syndemics: Toward a better approach to STI and HIV preventive interventions for men who have sex with men (MSM) in the United States. In S. O. Aral, K. A. Fenton, & J. A. Lipshutz (Eds.), The new public health and STD/HIV prevention (pp. 251–272). New York: Springer.
Halkitis, P. N., Kapadia, F., Bub, K. L., Barton, S., Moreira, A. D., & Stults, C. B. (2015). A longitudinal investigation of syndemic conditions among young gay, bisexual, and other MSM: The P18 Cohort Study. AIDS and Behavior, 19(6), 970–980.
Hammer, G. P., Kellogg, T. A., McFarland, W. C., Wong, E., Louie, B., Williams, I., … Klausner, J. D. (2003). Low incidence and prevalence of hepatitis C virus infection among sexually active non-intravenous drug-using adults, San Francisco, 1997–2000. Sexually Transmitted Diseases, 30(12), 919–924.
Hernández-Romieu, A. C., Siegler, A. J., Sullivan, P. S., Crosby, R., & Rosenberg, E. S. (2014). How often do condoms fail? A cross-sectional study exploring incomplete use of condoms, condom failures and other condom problems among black and white MSM in southern USA. Sexually Transmitted Infections, 90(8), 602–607.
Jenness, S. M., Maloney, K. M., Smith, D. K., Hoover, K. W., Goodreau, S. M., Rosenberg, E. S., … Sullivan, P. S. (2018). The PrEP care continuum and racial disparities in HIV incidence among men who have sex with men. BioRxiv, 249540.
Kelley, C. F., Rosenberg, E. S., O’Hara, B. M., Frew, P. M., Sanchez, T., Peterson, J. L., … Sullivan, P. S. (2012). Measuring population transmission risk for HIV: An alternative metric of exposure risk in men who have sex with men (MSM) in the US. PLoS ONE, 7(12), e53284. https://doi.org/10.1371/journal.pone.0053284.
Kelley, C. F., Vaughan, A. S., Luisi, N., Sanchez, T. H., Salazar, L. F., Frew, P. M., … Rosenberg, E. S. (2015). The effect of high rates of bacterial sexually transmitted infections on HIV incidence in a cohort of black and white men who have sex with men in Atlanta, Georgia. AIDS Research and Human Retroviruses, 31(6), 587–592.
Koken, J., Bimbi, D. S., & Parsons, J. (2010). Male and female escorts: A comparative analysis. In R. Weitzer (Ed.), Sex for sale: Prostitution, pornography, and the sex industry (pp. 205–223). New York: Routledge. https://doi.org/10.4324/9780203872802.
Lanier, Y., & Sutton, M. Y. (2013). Reframing the context of preventive health care services and prevention of HIV and other sexually transmitted infections for young men: New opportunities to reduce racial/ethnic sexual health disparities. American Journal of Public Health, 103(2), 262–269.
Malebranche, D. J., Gvetadze, R., Millett, G. A., & Sutton, M. Y. (2012). The relationship between gender role conflict and condom use among Black MSM. AIDS and Behavior, 16(7), 2051–2061.
Matthews, D. D., Herrick, A., Coulter, R. W., Friedman, M. R., Mills, T. C., Eaton, L. A., … POWER Study Team. (2016). Running backwards: Consequences of current HIV incidence rates for the next generation of black MSM in the United States. AIDS and Behavior, 20(1), 7–16.
Maulsby, C., Millett, G., Lindsey, K., Kelley, R., Johnson, K., Montoya, D., & Holtgrave, D. (2014). HIV among black men who have sex with men (MSM) in the United States: A review of the literature. AIDS and Behavior, 18(1), 10–25.
Mgbako, O., Park, S. H., Callander, D., Brinker, D. A., Kuhner, C., Carrico, A. W., … Duncan, D. T. (2019). Transactional sex, condomless anal sex, and HIV risk among men who have sex with men. International Journal of STD and AIDS, 30(8), 795–801.
Mimiaga, M. J., Reisner, S. L., Tinsley, J. P., Mayer, K. H., & Safren, S. A. (2009). Street workers and internet escorts: Contextual and psychosocial factors surrounding HIV risk behavior among men who engage in sex work with other men. Journal of Urban Health, 86(1), 54–66.
Minichiello, V., Scott, J., & Callander, D. (2013). New pleasures and old dangers: Reinventing male sex work. Journal of Sex Research, 50(3–4), 263–275.
Minichiello, V., Scott, J., & Callander, D. (2015). A new public health context to understand male sex work. BMC Public Health, 15(1), 282. https://doi.org/10.1186/s12889-015-1498-7.
Muraguri, N., Tun, W., Okal, J., Broz, D., Raymond, H. F., Kellogg, T., … Kaiser, R. (2015). HIV and STI prevalence and risk factors among male sex workers and other men who have sex with men in Nairobi, Kenya. Journal of Acquired Immune Deficiency Syndromes, 68(1), 91–96.
Mustanski, B., Phillips, G., Ryan, D. T., Swann, G., Kuhns, L., & Garofalo, R. (2017). Prospective effects of a syndemic on HIV and STI incidence and risk behaviors in a cohort of young men who have sex with men. AIDS and Behavior, 21(3), 845–857.
Nerlander, L. M., Hess, K. L., Sionean, C., Rose, C. E., Thorson, A., Broz, D., & Paz-Bailey, G. (2017). Exchange sex and HIV infection among men who have sex with men: 20 US cities, 2011. AIDS and Behavior, 21(8), 2283–2294.
Parsons, J. T., Grov, C., & Golub, S. A. (2012). Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: Further evidence of a syndemic. American Journal of Public Health, 102(1), 156–162.
Patel, V. V., Masyukova, M., Sutton, D., & Horvath, K. J. (2016). Social media use and HIV-related risk behaviors in young black and Latino gay and bi men and transgender individuals in New York City: Implications for online interventions. Journal of Urban Health, 93(2), 388–399.
Philbin, M. M., Kinnard, E. N., Tanner, A. E., Ware, S., Chambers, B. D., Ma, A., & Fortenberry, J. D. (2018). The association between incarceration and transactional sex among HIV-infected young men who have sex with men in the United States. Journal of Urban Health, 95(4), 576–583.
Raymond, H. F., & McFarland, W. (2009). Racial mixing and HIV risk among men who have sex with men. AIDS and Behavior, 13(4), 630–637.
Schrimshaw, E. W., Siegel, K., & Meunier, É. (2017). Venues where male sex workers meet partners: The emergence of gay hookup apps and web sites. American Journal of Public Health, 107(12), 1866.
Singer, M. C., Bulled, N., Ostrach, B., & Mendenhall, E. (2017). Syndemics and the biosocial conception of health. The Lancet, 389(10072), 941–950.
Singer, M. C., Erickson, P. I., Badiane, L., Diaz, R., Ortiz, D., Abraham, T., & Nicolaysen, A. M. (2006). Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science and Medicine, 63(8), 2010–2021.
Smith, W. P. (2012). Exploring dimensions of racism, homophobia, and social network as concomitant predictors of condom use in a sample of Black MSM. Journal of Gay & Lesbian Social Services, 24(4), 417–445.
Stall, R., Friedman, M., & Catania, J. A. (2008). Interacting epidemics and gay men’s health: A theory of syndemic production among urban gay men. In R. J. Wolitski, R. Stall, & R. O. Valdiserri (Eds.), Unequal opportunity: Health disparities affecting gay and bisexual men in the United States (pp. 251–274). New York: Oxford University Press.
Stall, R., Mills, T. C., Williamson, J., Hart, T., Greenwood, G., Paul, J., … Catania, J. A. (2003). Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health, 93(6), 1866–1867.
Sullivan, P. S., Peterson, J., Rosenberg, E. S., Kelley, C. F., Cooper, H., Vaughan, A., … Del Rio, C. (2014). Understanding racial HIV/STI disparities in black and white men who have sex with men: A multilevel approach. PLoS ONE, 9(3), e90514. https://doi.org/10.1371/journal.pone.0090514.
Tobin, K. E., Yang, C., King, K., Latkin, C. A., & Curriero, F. C. (2016). Associations between drug and alcohol use patterns and sexual risk in a sample of African American men who have sex with men. AIDS and Behavior, 20(3), 590–599.
Tsai, A. C., & Burns, B. F. (2015). Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Social Science and Medicine, 139, 26–35.
Underhill, K., Morrow, K. M., Colleran, C. M., Holcomb, R., Operario, D., Calabrese, S. K., … Mayer, K. H. (2014). Access to healthcare, HIV/STI testing, and preferred pre-exposure prophylaxis providers among men who have sex with men and men who engage in street-based sex work in the US. PLoS ONE, 9(11), e112425. https://doi.org/10.1371/journal.pone.0112425.
Valente, P. K., Mantell, J. E., Masvawure, T. B., Tocco, J. U., Restar, A. J., Gichangi, P., … Sandfort, T. G. (2020). “I couldn’t afford to resist”: Condom negotiations between male sex workers and male clients in Mombasa, Kenya. AIDS and Behavior, 24(3), 925–937.
Walters, S. M., Braksmajer, A., Coston, B., Yoon, I., Grov, C., Downing, M. J., … Hirshfield, S. (2020). A syndemic model of exchange sex among hiv-positive men who have sex with men. Archives of Sexual Behavior, 49(6), 1965–1978.
Wilson, P. A., Nanin, J., Amesty, S., Wallace, S., Cherenack, E. M., & Fullilove, R. (2014). Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. Journal of Urban Health, 91(5), 983–998.
Wong, F., Huang, Z., He, N., Smith, B., Ding, Y., Fu, C., & Young, D. (2008). HIV risks among gay-and non-gay-identified migrant money boys in Shanghai, China. AIDS Care, 20(2), 170–180.
Acknowledgements
We thank the Center for Black Equity and local Black Pride organizations for partnering with us to implement POWER, the community-based organizations who performed onsite HIV testing on the study’s behalf, the thousands of study participants who volunteered their time to contribute to this research, and members of the POWER Study Team who made data collection possible. The local Black Pride organizations are as follows: D.C. Black Pride, Detroit’s Hotter than July, Houston Splash, In the Life Atlanta, Memphis Black Pride, and Philadelphia Black Pride. The community-based organizations who performed onsite HIV testing are as follows: Atlanta: AID Atlanta, AIDS Health Care Foundation, NAESM; Detroit: Community Health Awareness Group, Horizons Project, Unified; Houston: Avenue 360, Houston AIDS Foundation, Positive Efforts; Memphis: Friends for Life; Philadelphia: Access Matters, Philadelphia FIGHT; Washington, D.C.: Us Helping Us. An earlier version of this manuscript was presented at the 2018 International Academy of Sex Research meeting (Madrid, Spain).
Funding
This study was partially supported by National Institutes of Health Grant R01NR013865 and analysis was partially supported by NIMH training Grant 5-T32MH094174-09.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to report for any of this paper’s contributing authors.
Ethical Approval
All study procedures were approved by the University of Pittsburgh Institutional Review Board.
Informed Consent
Informed consent was obtained for all enrolled participants. All study procedures were approved by the University of Pittsburgh Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
See Table 5.
Appendix 2
See Figure 2.
Structural equation model showing total and indirect effects pathways between past-year sex work, syndemic psychosocial conditions, and STI burden among sexually active Black men in the POWER study, 2014—2017. ***p < .001. Path coefficients and standard errors (parenthesized) are shown for total effects pathways. Italicized path coefficients and standard errors (parenthesized) are shown for indirect effects pathways. Model adjusted for year, city, income, bisexual behavior, Hispanic ethnicity, HIV positive status, bisexual behavior, and age ≥ 40. Covariate paths are suppressed for interpretability. Fit statistics are as follows: SRMR = 0.034; RMSEA = 0.049 (95% CI 0.046, 0.052); CFI = 0.928; TLI = 0.902
Appendix 3
See Table 6.
Rights and permissions
About this article
Cite this article
Chandler, C.J., Meunier, É., Eaton, L.A. et al. Syndemic Health Disparities and Sexually Transmitted Infection Burden Among Black Men Who Have Sex with Men Engaged in Sex Work in the U.S.. Arch Sex Behav 50, 1627–1640 (2021). https://doi.org/10.1007/s10508-020-01828-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-020-01828-2