Abstract
Whether in the West or the East, the connection between the ear and the rest of the body has been explored for a long time. Especially in the past century or more, the relevant theoretical and applied research on the ear has greatly promoted the development of ear therapy, and finally the concept of transcutaneous auricular vagus nerve stimulation (taVNS) has been proposed. The purpose of taVNS is to treat a disease non-invasively by applying electrical current to the cutaneous receptive field formed by the auricular branch of the vagus nerve in the outer ear. In the past two decades, taVNS has been a topic of basic, clinical, and transformation research. It has been applied as an alternative to drug treatment for a variety of diseases. Based on the rapid understanding of the application of taVNS to human health and disease, some limitations in the development of this field have also been gradually exposed. Here, we comprehensively review the origin and research status of the field.


Similar content being viewed by others
References
Rossi S, Santarnecchi E, Valenza G, Ulivelli M. The heart side of brain neuromodulation. Philos Trans A Math Phys Eng Sci 2016, 374: 20150187.
Nicholson WC, Kempf MC, Moneyham L, Vance DE. The potential role of vagus-nerve stimulation in the treatment of HIV-associated depression: a review of literature. Neuropsychiatr Dis Treat 2017, 13:1677–1689.
Ben-Menachem E, Revesz D, Simon BJ, Silberstein S. Surgically implanted and non-invasive vagus nerve stimulation: a review of efficacy, safety and tolerability. Eur J Neurol 2015, 22:1260–1268.
He W, Wang X, Shi H, Shang H, Li L, Jing X, et al. Auricular acupuncture and vagal regulation. Evid Based Complement Alternat Med 2012, 2012: 786839.
Sator-Katzenschlager SM, Michalek-Sauberer A. P-Stim Auricular electroacupuncture stimulation device for pain relief. Expert Rev Med Devices 2007, 4: 23–32.
P Nogier. From Acuriculotherapy to Auriculomedicine, Maisonneuve, Sainte-Ruffine, France, 1981.
Gori L, Firenzuoli F. Ear acupuncture in european traditional medicine. Evid Based Complement Alternat Med 2007, 4:13–16.
Peuker ET, Filler TJ. The nerve supply of the human auricle. Clin Anat 2002, 15:35–37.
Chen M, Yu L, Ouyang F, Liu Q, Wang Z, Wang S, et al. The right side or left side of noninvasive transcutaneous vagus nerve stimulation: Based on conventional wisdom or scientific evidence? Int J Cardiol 2015, 187: 44–45.
Howland RH. Vagus nerve stimulation. Curr Behav Neurosci Rep 2014, 1: 64–73.
Clancy JA, Mary DA, Witte KK, Greenwood JP, Deuchars SA, Deuchars J. Non-invasive vagus nerve stimulation in healthy humans reduces sympathetic nerve activity. Brain Stimul 2014, 7(6): 871–877.
Kaniusas E, Kampusch S, Tittgemeyer M, Panetsos F, Gines RF, Papa M, et al. Current directions in the auricular vagus nerve stimulation I - A physiological perspective. Front Neurosci 2019, 13: 854.
Lewis PM, Thomson RH, Rosenfeld JV, Fitzgerald PB. Brain neuromodulation techniques: A review. Neuroscientist 2016, 22(4): 406–421.
Kaniusas E, Kampusch S, Tittgemeyer M, Panetsos F, Gines RF, Papa M, et al. Current directions in the auricular vagus nerve stimulation II - An engineering perspective. Front Neurosci 2019, 13: 772.
Ventureyra EC. Transcutaneous vagus nerve stimulation for partial onset seizure therapy. A new concept. Childs Nerv Syst 2000, 16:101–102.
Ay I, Nasser R, Simon B, Ay H. Transcutaneous cervical vagus nerve stimulation ameliorates acute ischemic injury in rats. Brain Stimul 2016, 9: 166–173.
Ma J, Qiao P, Li Q, Wang Y, Zhang L, Yan LJ, et al. Vagus nerve stimulation as a promising adjunctive treatment for ischemic stroke. Neurochem Int 2019; 131:104539.
Lendvai IS, Maier A, Scheele D, Hurlemann R, Kinfe TM. Spotlight on cervical vagus nerve stimulation for the treatment of primary headache disorders: a review. J Pain Res 2018, 11:1613–1625.
Broncel A, Bocian R, Kłos-Wojtczak P, Kulbat-Warycha K, Konopacki J. Vagal nerve stimulation as a promising tool in the improvement of cognitive disorders. Brain Res Bull 2020, 155: 37–47.
Bucksot JE, Morales Castelan K, Skipton SK, Hays SA. Parametric characterization of the rat Hering-Breuer reflex evoked with implanted and non-invasive vagus nerve stimulation. Exp Neurol 2020, 327: 113220.
Gurel NZ, Huang M, Wittbrodt MT, Jung H, Ladd SL, Shandhi MMH, et al. Quantifying acute physiological biomarkers of transcutaneous cervical vagal nerve stimulation in the context of psychological stress. Brain Stimul 2020, 13: 47–59.
Rimmele F, Jürgens TP. Neuromodulation in primary headaches: current evidence and integration into clinical practice. Curr Opin Neurol 2020, 33: 329–337.
Magis D, Gérard P, Schoenen J. Transcutaneous Vagus Nerve Stimulation (tVNS) for headache prophylaxis: initial experience. J Headache Pain 2013, 14:198.
Muthulingam JA, Olesen SS, Hansen TM, Brock C, Drewes AM, Frøkjær JB. Study protocol for a randomised double-blinded, sham-controlled, prospective, cross-over clinical trial of vagal neuromodulation for pain treatment in patients with chronic pancreatitis. BMJ Open 2019, 9: e029546.
Safi S, Ellrich J, Neuhuber W. Myelinated axons in the auricular branch of the human vagus nerve. Anat Rec (Hoboken) 2016, 299:1184–1191.
Nemeroff CB, Mayberg HS, Krahl SE, McNamara J, Frazer A, Henry TR, et al. VNS therapy in treatment-resistant depression: clinical evidence and putative neurobiological mechanisms. Neuropsychopharmacology 2006, 31: 1345–1355.
Badran BW, Yu AB, Adair D, Mappin G, DeVries WH, Jenkins DD, et al. Laboratory administration of transcutaneous auricular vagus nerve stimulation (taVNS): Technique, targeting, and considerations. J Vis Exp 2019, 143:https://doi.org/10.3791/58984.
Redgrave J, Day D, Leung H, Laud PJ, Ali A, Lindert R, et al. Safety and tolerability of Transcutaneous Vagus Nerve stimulation in humans: a systematic review. Brain Stimul 2018, 11:1225–1238.
Nomura S, Mizuno N. Central distribution of primary afferent fibers in the Arnold's nerve (the auricular branch of the vagus nerve): A transganglionic HRP study in the cat. Brain Res 1984, 292:199–205.
Bermejo P, López M, Larraya I, Chamorro J, Cobo JL, Ordóñez S, et al. Innervation of the human cavum conchae and auditory canal: anatomical basis for transcutaneous auricular nerve stimulation. Biomed Res Int 2017, 2017: 7830919.
Yakunina N, Kim SS, Nam EC. Optimization of transcutaneous vagus nerve stimulation using functional MRI. Neuromodulation 2017, 20: 290–300.
Badran BW, Brown JC, Dowdle LT, Mithoefer OJ, LaBate NT, Coatsworth J, et al. Tragus or cymba conchae? Investigating the anatomical foundation of transcutaneous auricular vagus nerve stimulation (taVNS). Brain Stimul 2018, 11: 947–948
Butt MF, Albusoda A, Farmer AD, Aziz Q. The anatomical basis for transcutaneous auricular vagus nerve stimulation. J Anat 2020, 236: 588–611.
Li S, Wang Y, Gao G, Guo X, Zhang Y, Zhang Z, et al. Transcutaneous auricular vagus nerve stimulation at 20 Hz improves depression-like behaviors and down-regulates the hyperactivity of HPA axis in chronic unpredictable mild stress model rats. Front Neurosci 2020, 14: 680.
Badran BW, Dowdle LT, Mithoefer OJ, LaBate NT, Coatsworth J, Brown JC, et al. Neurophysiologic effects of transcutaneous auricular vagus nerve stimulation (taVNS) via electrical stimulation of the tragus: A concurrent taVNS/fMRI study and review. Brain Stimul 2018, 11: 492–500.
Stefan H, Kreiselmeyer G, Kerling F, Kurzbuch K, Rauch C, Heers M, et al. Transcutaneous vagus nerve stimulation (t-VNS) in pharmacoresistant epilepsies: A proof of concept trial. Epilepsia 2012, 53: e115–118.
He W, Jing X, Wang X, Rong P, Li L, Shi H, et al. Transcutaneous auricular vagus nerve stimulation as a complementary therapy for pediatric epilepsy: a pilot trial. Epilepsy Behav 2013, 28: 343–346.
Rong P, Liu A, Zhang J, Wang Y, He W, Yang A, et al. Transcutaneous vagus nerve stimulation for refractory epilepsy: A randomized controlled trial. Clin Sci (Lond) 2014.
Aihua L, Lu S, Liping L, Xiuru W, Hua L, Yuping W. A controlled trial of transcutaneous vagus nerve stimulation for the treatment of pharmacoresistant epilepsy. Epilepsy Behav 2014, 39: 105–110.
Bauer S, Baier H, Baumgartner C, Bohlmann K, Fauser S, Graf W, et al. Transcutaneous vagus nerve stimulation (tVNS) for treatment of drug-resistant epilepsy: A randomized, double-blind clinical trial (cMPsE02). Brain Stimul 2016, 9: 356–363.
Hamer HM, Bauer S. Lessons learned from transcutaneous vagus nerve stimulation (tVNS). Epilepsy Res 2019, 153: 83–84.
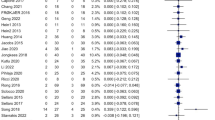
Wu K, Wang Z, Zhang Y, Yao J, Zhang Z. Transcutaneous vagus nerve stimulation for the treatment of drug-resistant epilepsy: a meta-analysis and systematic review. ANZ J Surg 2020, 90: 467–471.
Assenza G, Campana C, Colicchio G, Tombini M, Assenza F, Di Pino G, et al. Transcutaneous and invasive vagal nerve stimulations engage the same neural pathways: in-vivo human evidence. Brain Stimul 2017, 10: 853–854.
Hein E, Nowak M, Kiess O, Biermann T, Bayerlein K, Kornhuber J, et al. Auricular transcutaneous electrical nerve stimulation in depressed patients: a randomized controlled pilot study. J Neural Transm (Vienna) 2013, 120: 821–827.
Trevizol AP, Taiar I, Barros MD, Liquidatto B, Cordeiro Q, Shiozawa P. Transcutaneous vagus nerve stimulation (tVNS) protocol for the treatment of major depressive disorder: a case study assessing the auricular branch of the vagus nerve. Epilepsy Behav 2015, 53: 166–167.
Trevizol AP, Shiozawa P, Taiar I, Soares A, Gomes JS, Barros MD, et al. Transcutaneous vagus nerve stimulation (taVNS) for major depressive disorder: an open label proof of concept trial. Brain Stimul 2016, 9: 453–454.
Rong P, Liu J, Wang L, Liu R, Fang J, Zhao J, et al. Effect of transcutaneous auricular vagus nerve stimulation on major depressive disorder: A nonrandomized controlled pilot study. J Affect Disord 2016, 195: 172–179.
Fang J, Rong P, Hong Y, Fan Y, Liu J, Wang H, et al. Transcutaneous vagus nerve stimulation modulates default mode network in major depressive disorder. Biol Psychiatry 2016, 79: 266–273.
Wu C, Liu P, Fu H, Chen W, Cui S, Lu L, et al. Transcutaneous auricular vagus nerve stimulation in treating major depressive disorder: a systematic review and meta-analysis. Medicine (Baltimore) 2018, 97: e13845.
Kong J, Fang J, Park J, Li S, Rong P. Treating depression with transcutaneous auricular vagus nerve stimulation: state of the art and future perspectives. Front Psychiatry 2018, 9: 20.
Jiang T. Recent progress in basic and clinical research on disorders of consciousness. Neurosci Bull 2018, 34: 589–591.
Noé E, Ferri J, Colomer C, Moliner B, O'Valle M, Ugart P, et al. Feasibility, safety and efficacy of transauricular vagus nerve stimulation in a cohort of patients with disorders of consciousness. Brain Stimul 2020, 13: 427–429.
Yu YT, Yang Y, Wang LB, Fang JL, Chen YY, He JH, et al. Transcutaneous auricular vagus nerve stimulation in disorders of consciousness monitored by fMRI: The first case report. Brain Stimul 2017, 10: 328–330.
Zhao B, Li L, Jiao Y, Luo M, Xu K, Hong Y, et al. Transcutaneous auricular vagus nerve stimulation in treating post-stroke insomnia monitored by resting-state fMRI: The first case report. Brain Stimul 2019, 12: 824–826.
Liu L, Zhao M, Yu X, Zang W. Pharmacological modulation of vagal nerve activity in cardiovascular diseases. Neurosci Bull 2019, 35:156–166.
Olshansky B, Sabbah HN, Hauptman PJ, Colucci WS. Parasympathetic nervous system and heart failure pathophysiology and potential implications for therapy. Circulation 2008, 118: 863–871.
De Ferrari GM, Crijns HJ, Borggrefe M, Milasinovic G, Smid J, Zabel M, et al. Chronic vagus nerve stimulation: a new and promising therapeutic approach for chronic heart failure. European Heart Journal 2011, 32: 847–855.
Scherlag BJ, Helfant RH, Haft JI, Damato AN. Electrophysiology underlying ventricular arrhythmias due to coronary ligation. Am J Physiol 1970, 219: 1665–1671.
Kent KM, Smith ER, Redwood DR, Epstein SE. Electrical stability of acutely ischemic myocardium. Influences of heart rate and vagal stimulation. Circulation 1973, 47: 291–298.
Vanoli E, De Ferrari GM, Stramba-Badiale M, Hull SS, Foreman RD, Schwartz PJ. Vagal stimulation and prevention of sudden death in conscious dogs with a healed myocardial infarction. Circ Res 1991, 68: 1471–1481.
Myers RW, Pearlman AS, Hyman RM, Goldstein RA, Kent KM, Goldstein RE, et al. Beneficial effects of vagal stimulation and bradycardia during experimental acute myocardial ischemia. Circulation 1974, 49: 943–947.
James RG, Arnold JM, Allen JD, Pantridge JF, Shanks RG. The effects of heart rate, myocardial ischemia and vagal stimulation on the threshold for ventricular fibrillation. Circulation 1977, 55: 311–317.
Yu L, Wang S, Zhou X, Wang Z, Huang B, Liao K, et al. Chronic intermittent low-level stimulation of tragus reduces cardiac autonomic remodeling and ventricular arrhythmia inducibility in a post-infarction canine model. JACC Clin Electrophysiol 2016, 2: 330–339.
Bonaz B, Sinniger V, Pellissier S. Anti-inflammatory properties of the vagus nerve: potential therapeutic implications of vagus nerve stimulation. The Journal of Physiology 2016, 594: 5781–5790.
Lu KH, Cao J, Oleson S, Ward MP, Phillips RJ, Powley TL, et al. Vagus nerve stimulation promotes gastric emptying by increasing pyloric opening measured with magnetic resonance imaging. Neurogastroenterol Motil 2018, 30: e13380.
Frøkjaer JB, Bergmann S, Brock C, Madzak A, Farmer AD, Ellrich J, et al. Modulation of vagal tone enhances gastroduodenal motility and reduces somatic pain sensitivity. Neurogastroenterol Motil 2016, 28: 592–598.
A Zillekens, GS Hong, B Schneiker, A Schmidt, JC Kalff, S Wehner. Untersuchung des Effektes einer transkutanen Vagus nerve stimulation auf den postoperativen Ileus im Maus model. Z Gastroenterol 2014, 52 - FV39.
Rawat JK, Roy S, Singh M, Guatam S, Yadav RK, Ansari MN, et al. Transcutaneous vagus nerve stimulation regulates the cholinergic anti-inflammatory pathway to counteract 1, 2-dimethylhydrazine induced colon carcinogenesis in albino wistar rats. Front Pharmacol 2019, 10: 353.
Williams EK, Chang RB, Strochlic DE, Umans BD, Lowell BB, Liberles SD. Sensory neurons that detect stretch and nutrients in the digestive system. Cell 2016, 166: 209–221.
Beekwilder J P, Beems T. Overview of the clinical applications of vagus nerve stimulation. J Clin Neurophysiol 2010, 27: 130–138.
S.C. Schachter, C.B. Saper, Vagus nerve stimulation, Epilepsia 1998, 39: 677–686.
Brandt C, Volk H A, Loscher W. Striking differences in individual anticonvulsant response to phenobarbital in rats with spontaneous seizures after status epilepticus. Epilepsia 2004, 45: 1488–1497.
Brezun J M, Daszuta A. Depletion in serotonin decreases neurogenesis in the dentate gyrus and the subventricular zone of adult rats. Neuroscience 1999, 89: 999–1002.
Castle M, Comoli E, Loewy A D. Autonomic brainstem nuclei are linked to the hippocampus. Neuroscience 2005, 134: 657–669.
He W, Jing XH, Zhu B, Zhu XL, Li L, Bai WZ, et al. The auriculo-vagal afferent pathway and its role in seizure suppression in rats. BMC Neurosci 2013, 14: 85.
Deuchars SA, Lall VK, Clancy J, Mahadi M, Murray A, Peers L, et al. Mechanisms underpinning sympathetic nervous activity and its modulation using transcutaneous vagus nerve stimulation. Exp Physiol 2018, 103: 326–331.
Mahadi KM, Lall VK, Deuchars SA, Deuchars J. Cardiovascular autonomic effects of transcutaneous auricular nerve stimulation via the tragus in the rat involve spinal cervical sensory afferent pathways. Brain Stimul 2019, 12: 1151–1158.
Fallgatter AJ, Ehlis AC, Ringel TM, Herrmann MJ. Age effect on far field potentials from the brain stem after transcutaneous vagus nerve stimulation. Int J Psychophysiol 2005, 56: 37–43.
Fallgatter AJ, Neuhauser B, Herrmann MJ, Ehlis AC, Wagener A, Scheuerpflug P. Far field potentials from the brain stem after transcutaneous vagus nerve stimulation. J Neural Transm (Vienna) 2003, 110: 1437–1443.
Polak T, Markulin F, Ehlis AC, Langer JB, Ringel TM, Fallgatter AJ. Far field potentials from brain stem after transcutaneous vagus nerve stimulation: optimization of stimulation and recording parameters. J Neural Transm (Vienna) 2009, 116: 1237–1242.
Chae JH, Nahas Z, Lomarev M, Denslow S, Lorberbaum JP, Bohning DE, et al. A review of functional neuroimaging studies of vagus nerve stimulation (VNS). J Psychiatr Res 2003, 37: 443–455.
Kraus T, Hösl K, Kiess O, Schanze A, Kornhuber J, Forster C. BOLD fMRI deactivation of limbic and temporal brain structures and mood enhancing effect by transcutaneous vagus nerve stimulation. J Neural Transm (Vienna) 2007, 114: 1485–1493.
Kraus T, Kiess O, Hösl K, Terekhin P, Kornhuber J, Forster C. CNS BOLD fMRI effects of sham-controlled transcutaneous electrical nerve stimulation in the left outer auditory canal-a pilot study. Brain Stimul 2013, 6: 798–804.
Dietrich S, Smith J, Scherzinger C, Hofmann-Preiss K, Freitag T, Eisenkolb A, et al. A novel transcutaneous vagus nerve stimulation leads to brainstem and cerebral activations measured by functional MRI. Biomed Tech (Berl) 2008, 53: 104–111.
Mercante B, Ginatempo F, Manca A, Melis F, Enrico P, Deriu F. Anatomo-physiologic basis for auricular stimulation. Med Acupunct 2018, 30: 141–150.
Jiang Y, Cao Z, Ma H, Wang G, Wang X, Wang Z, et al. Auricular vagus nerve stimulation exerts antiinflammatory effects and immune regulatory function in a 6-OHDA model of Parkinson's disease. Neurochem Res 2018, 43: 2155.
Tracey KJ. The inflammatory reflex. Nature 2002, 420: 853–859.
Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Vest 2007, 117: 289–296.
Acknowledgements
This review was supported by the National Key R&D Program of China (2018YFC1705800), the National Natural Science Foundation of China (81803872, 81674072), the Joint Sino-German Research Project (GZ1236), and the Fundamental Research Funds for the Central Public Welfare Research Institutes (ZZ201813006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Wang, Y., Li, SY., Wang, D. et al. Transcutaneous Auricular Vagus Nerve Stimulation: From Concept to Application. Neurosci. Bull. 37, 853–862 (2021). https://doi.org/10.1007/s12264-020-00619-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12264-020-00619-y