Abstract
Introduction
In December 2019, an outbreak of a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) began, resulting in a number of antivirals and immune modulators being repurposed to treat the associated coronavirus disease 2019 (COVID-19). Many patients requiring treatment for COVID-19 may have either pre-existing renal or hepatic disease or experience acute renal/hepatic injury as a result of the acute infection. Altered renal or hepatic function can significantly affect drug concentrations of medications due to impaired drug metabolism and excretion, resulting in toxicity or reduced efficacy. The aim of this paper is to review the pharmacokinetics and available study data for the experimental COVID-19 therapies in patients with any degree of renal or hepatic impairment to make recommendations for dosing.
Methods
COVID-19 agents included in these recommendations were listed as primaries on the University of Liverpool COVID-19 drug interaction website (www.covid19-druginteractions.org), initially identified from Clinicialtrials.gov and ChicCTR.org.cn. A literature search was performed using PubMed and EMBASE as well as product licences and pharmacokinetic databases.
Findings
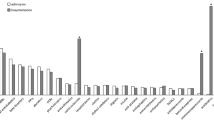
Remdesivir, dexamethasone, azithromycin, favipiravir, lopinavir/ritonavir, atazanavir, hydroxychloroquine, interferon beta, ribavirin, tocilizumab, anakinra and sarilumab were identified as experimental drugs being used in COVID-19 trials as of November 2020. Limited study data was found for these drugs in patients with renal or hepatic impairment for COVID-19 or other indications. Recommendations were made based on available data, consideration of pharmacokinetic properties (including variability), the dosing and anticipated treatment duration of each regimen in COVID-19 and known toxicities.
Conclusion
Dosing of drugs used to treat COVID-19 in patients with renal or hepatic impairment is complex. These recommendations were produced to provide guidance to clinicians worldwide who are treating patients with COVID-19, many of whom will have some degree of acute or chronic renal or hepatic impairment.
Similar content being viewed by others
Remdesivir and favipiravir should not be used in patients with impaired renal function and when ribavirin and anakinra are used in patients with impaired renal function, we would recommend dose adjustments based on the pharmacokinetics of these drugs. |
When atazanavir and favipiravir are used for COVID-19 treatment in patients with hepatic impairment, dose adjustments are recommended based on the pharmacokinetics. For tociluzumab, interferon beta and sarilumab, caution is required when used in COVID-19 patients with Child Pugh A/B. |
Licensed recommendations of these medicines in previous non-COVID-19 settings can inform dosing choices; however, often the dosage used of these medicines for the treatment of COVID-19 varies significantly amongst different studies or empirical usage. Short-term use could be considered in some circumstances where license restrictions are in place. |
1 Introduction
In December 2019, an outbreak of a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) began, which has since become a global pandemic, significantly affecting human health and global economies. A number of antivirals and immune modulators have been repurposed for the treatment of COVID-19 and these experimental agents have been used both within and outside clinical studies. Whilst most data indicate the lungs as the main organ involved in the disease, data now exist showing significant involvement of the liver and kidneys [1, 2], which can potentially impair the metabolism and excretion of the medications taken to treat the disease.
Altered renal or hepatic function can significantly affect drug concentrations of COVID-19 medications due to the impaired capacity of these organs to metabolise and excrete drugs. As well as altering elimination, the first pass metabolism can also be affected and thus the absorption and bioavailability of drugs. These changed pharmacokinetics can lead to increased or decreased exposure, resulting in either toxicity or reduced efficacy, which could be of clinical relevance based on the therapeutic window and pharmacodynamics of the specific drug. However, additional toxicity might be acceptable when the drug is effective in severe cases of COVID-19. In addition, the disease itself could also influence drug exposure.
Chronic liver disease represents a major disease burden with worldwide estimates showing an incidence of 844 million people [3]. Repurposed treatments are being used to treat COVID-19 globally in patients with both pre-existing chronic liver disease and new onset acute liver injury, so there is a need for appropriate dosing strategies. Mortality and disease-related complications of patients with COVID-19 and cirrhosis, such as hepatic encephalopathy, upper gastrointestinal bleeding, liver failure and secondary infection, are being followed up in multi-centred cohort clinical studies [4] but as of now few data exist in this group. Understanding how pre-existing liver disease influences liver injury in patients with COVID-19 and consequently drug metabolism needs further evaluation. Overall, the incidence of elevated serum liver function tests (LFTs) in hospitalised patients with COVID-19, primarily elevated AST and ALT, and elevated bilirubin, ranges from 14 to 75% [5,6,7,8,9,10] in patients with or without pre-existing liver disease. In a multi-centre study in the US, 75% of 2273 patients who tested positive had a peak ALT greater than the upper limit of normal (ULN), 45% with a rise of 2× ULN indicating that acute liver injury is common. This is most often mild but those with severe liver injury had a more severe clinical course, including higher rates of intensive care unit (ICU) admission, intubation, renal replacement therapy and mortality [9]. Low albumin has also been found to be a marker of severe infection and poor prognosis [11]. Liver damage in COVID-19 patients might be caused by the viral infection of liver cells, by immune-associated inflammation (cytokine storm release of interleukin [IL]6) or pneumonia-associated hypoxia. Additionally, in a large population study of hospitalised patients with COVID-19 in the UK, pre-existing liver disease was associated with an increased age-adjusted mortality [12].
Similar considerations are required with respect to renal function. Patients with COVID-19 may have pre-existing renal impairment due to chronic kidney disease (CKD), which is known to have an estimated global prevalence of 8.5–9.8% [13]. Preliminary data from New York showed that of the intubated patients admitted to the ICU, 20–40% had acute kidney injury (AKI) requiring renal replacement therapy (RRT) [14]. In Wuhan, lower numbers were reported: 5/138 (3.6%) patients developed AKI [15]. An early report from the United States described that 69% of COVID-19-positive patients (n = 43) developed an AKI. Aggarwal et al. [16] showed with a retrospective analysis that haematuria and proteinuria were present in 44% and 59% of COVID-19-infected patients at admission (n = 193) [17]. One hypothesis is that SARS-CoV-2 directly affects the kidney as it uses angiotensin converting enzyme (ACE) 2 to target cells. This could potentially result in loss of function. Another hypothesis is that a cytokine storm could contribute to impaired renal function or AKI [1, 18].
Based on these data and the high burden of pre-existing liver and renal disease, there is a need for evidence-based dosing recommendations for repurposed COVID-19 treatments in these special populations who are excluded from many of the clinical trials. Therefore, the aim of this paper is to review the pharmacokinetics and available study data for the experimental COVID-19 therapies in patients with any degree of renal or hepatic impairment to make recommendations for dosing in these special populations.
Despite many studies having reported both positive and negative outcomes for some of the drugs discussed in this paper, empirical use remains high in many countries with limited access to clinical studies. We do not comment on the efficacy of these agents or examine pharmacokinetic (PK) variability or bioavailability in liver disease due to lack of any pharmacokinetic/pharmacodynamic (PK/PD) data for any of the COVID therapies. As most of the world enters a second wave, higher than the first in many continents, there has been a further increase in the use of these repurposed medications, particularly in settings where there is limited choice of therapies available, and the need for appropriate dosing remains paramount.
2 Methods
2.1 Identifying COVID-19 Therapies
Repurposed therapies for COVID-19 reviewed for these recommendations were listed as primaries on the University of Liverpool COVID-19 drug interaction website [19] on 15 October 2020. The COVID-19 drug interaction website has been accessed in 196 countries and uses therapies selected for inclusion as an experimental drug therapy based on global use for treatment or prevention of COVID-19 within randomised controlled trials that are multi-country or multi-centre within one country [20]. These were identified by searching ClinicialTrials.gov and ChicCTR.org.cn for the following search terms: COVID-19, 2019-nCoV, 2019 novel coronavirus, and SARS-CoV-2. PubMed was searched with the MeSH term ‘COVID-19’. We identified dexamethasone, atazanavir, lopinavir/ritonavir, remdesivir, favipiravir, hydroxychloroquine, azithromycin, interferon beta, ribavirin, tocilizumab, anakinra and sarilumab.
Given that COVID-19 drugs are unlikely to be used in isolation, we should also consider concomitant drugs and potential drug interactions [19, 21], the effect of which may be potentiated in renal or hepatic impairment. For the purpose of this review, mild, moderate and hepatic impairment are referred to in line with drug licence and can be assumed to be Child Pugh Turcotte (CPT) score A, B and C, respectively. Monoclonal and polyclonal antibodies used in early clinical studies of SARS Cov-2 have also been excluded as, to date, there is nothing published on special populations to make recommendations on.
2.2 Identifying Hepatic and Renal Recommendations
A literature search was performed using PubMed and EMBASE to identify relevant English-language articles published up to and including October 15, 2020. Search terms included COVID-19, 2019-nCoV, SARS-CoV-2, 2019 novel coronavirus, and SARS-CoV-2 in combination with liver disease/impairment, cirrhosis and decompensation to identify peer-reviewed studies containing information on dosing in hepatic impairment. Similarly, this was carried out for end-stage renal disease and RRT/dialysis. To date, there is little published on the use of these agents in COVID-19 in renal and hepatic impairment. Active clinical trials in liver and kidney disease were identified using the above search terms on ClinicalTrials.gov and in the Chinese Clinical Trial Registry. As many of the primary medications have been repurposed, the majority of data for this article came from separate searches that were carried out for each therapeutic agent with search terms of liver impairment, cirrhosis, end-stage renal disease and dialysis. The summary of product characteristics (SmPC) from the European Medicines Agency (EMA), the Prescribing Information from the US Food and Drug Administration (FDA), renal drug handbook [22], LiverTox [23] and MicroMedex [24] were significant sources of information for this review.
3 Repurposed Treatments
The pharmacokinetic parameters of the repurposed treatments are summarised in Table 1.
3.1 Dexamethasone
Dexamethasone is a glucocorticoid used in the treatment of a variety of inflammatory and autoimmune conditions. It is used at a wide range of doses, licensed from 0.5 to 80 mg daily, and is normally administered either orally or intravenously [25]. It is used in COVID-19 dosed at 6 mg daily for 10 days, either orally or intravenously [26].
3.1.1 Renal Recommendations
Dexamethasone is metabolised in the liver and 65% of the unchanged drug is eliminated renally within 24 h. Workman et al. [27] found similar dexamethasone pharmacokinetics for patients with normal renal function and chronic renal failure. Another study [28] observed increased clearance and shortened elimination half-life, thought to be secondary to decreased protein binding of dexamethasone in uraemia [29]. High doses of dexamethasone such as 40 mg daily for 4-day cycles are used safely in the treatment of multiple myeloma, a condition often associated with significant renal dysfunction [30]. No dose adjustment is recommended for patients with renal impairment, although frequent patient monitoring is advised in the product licence [25]. Dexamethasone pharmacokinetics do not appear to be significantly impacted by RRT and it may be used at the same dose as in normal renal function in this setting [22] (Table 2).
3.1.2 Hepatic Recommendations
Other glucocorticoids, including prednisolone, are used regularly for patients with significant liver disease in the treatment of autoimmune and alcoholic hepatitis, including for patients with cirrhosis, acute liver failure, ALT/AST > 10× ULN and post-liver transplant [31, 32]. Dexamethasone is metabolised in the liver via CYP3A4 [33]. The licence for dexamethasone contains no specific recommendation for dosing in hepatic impairment, although it states that the elimination half-life is prolonged in severe liver disease [25]. Glucocorticoids can be associated with hepatic adverse effects; when used for long periods of time they can cause hepatic enlargement and steatosis. Given the low dose (6 mg daily) and short duration, this is unlikely to be significant when treating patients with COVID-19. No dose adjustment is required (Table 3).
3.2 Atazanavir and Atazanavir/Ritonavir
Atazanavir is a protease inhibitor licensed either alone at a dose of 400 mg or in combination with the pharmacokinetic booster ritonavir at a dose of 300/100 mg for the treatment of HIV infection, which is also the recommended dose in COVID-19 treatment [34, 35].
3.2.1 Renal Recommendations
Since atazanavir undergoes minimal renal elimination, the standard dosages of 300/100 mg or 400 mg (unboosted) can be used in patients with renal impairment [36]. Previously it was reported that exposure in patients undergoing haemodialysis was decreased by 30–50% [35]. However, one case report described comparable clearance in patients with and without dialysis [37]. In view of the limited data available, and the potential for increased atazanavir clearance during haemodialysis, boosted atazanavir may be preferred to achieve adequate exposure in patients undergoing RRT.
3.2.2 Hepatic Recommendations
Atazanavir is primarily hepatically metabolised and increased plasma concentrations are observed in patients with hepatic impairment [34, 35]. The majority of clinical studies carried out in patients with advanced liver disease have been with unboosted atazanavir as exposure is increased in patients with impaired hepatic function, negating the need for boosting. The impact of moderate to severe hepatic impairment on atazanavir pharmacokinetics (without ritonavir) was evaluated in 16 patients with advanced liver disease (14 CPT B and 2 CPT C patients) after a single atazanavir 400-mg dose. The mean area under the plasma concentration curve (AUC) was 42% higher and mean half-life increased (12.1 h vs 6.4 h) in patients with hepatic impairment compared with healthy volunteers [35]. In a study of similar size (10 CPT B and 5 CPT C patients) following atazanavir 400 mg daily, median AUC and minimal plasma concentration (Cmin) values were similar to those in historical controls. Interpatient variability in AUC was high although most of the patients were also on concomitant tenofovir and/or acid-suppressing therapy, factors that will also affect exposure [38]. As atazanavir is an inhibitor of UGT1A1, physicians should be aware of increased bilirubin concentration; however, this does not affect liver function and liver function markers [39].
The recommendation is to use unboosted atazanavir at a dose of 400 mg daily in mild hepatic impairment with a reduction to 300 mg in moderate hepatic impairment. Atazanavir is not recommended by the manufacturer in severe hepatic impairment [35], although data from several small studies is reassuring. Large interpatient variability in atazanavir exposure has been observed [40]. Considering this, along with the short duration of therapy used for COVID-19, the impact of any increased atazanavir exposure is unlikely to be clinically significant. However, raised serum bilirubin concentrations strongly correlate with increased atazanavir concentrations [40]. Thus, we recommend that atazanavir can be considered in severe hepatic impairment (300 mg once daily) if clinical benefit is likely to outweigh the potential risk, with close monitoring of hepatic function during treatment.
3.3 Lopinavir/Ritonavir
Similar to atazanavir, lopinavir is a protease inhibitor given with the pharmacokinetic booster ritonavir as a fixed-dose tablet, licensed for HIV treatment. In adults, the recommended dose is 400/100 mg twice daily [41], which is also the dose used in COVID-19 treatment [42].
3.3.1 Renal Recommendations
Approximately 10.4% of lopinavir is renally cleared, of which 2.2% is the unchanged drug [41, 43]. Therefore, no dose adjustments are needed in patients with renal impairment. Gupta et al. [44] studied exposure of lopinavir/ritonavir in 13 patients undergoing haemodialysis and reported that the AUC and maximal plasma concentration (Cmax) were comparable with historical controls. The Cmin was lower than expected (44% decrease). However, the authors concluded that twice daily dosing would maintain adequate Cmin levels. We recommend that lopinavir/ritonavir 400/100 mg twice daily can be prescribed in patients undergoing RRT.
3.3.2 Hepatic Recommendations
Lopinavir/ritonavir is mainly hepatically cleared with 82.6% excreted in the faeces, 19.8% as unchanged drug [41]. It has not been studied in severe hepatic impairment and its use is contraindicated [41, 43]. Lopinavir/ritonavir pharmacokinetics were studied in patients with mild (n = 6) and moderate (n = 6) hepatic disease. Lopinavir pharmacokinetics were similar in both, with Cmax and AUC increased by 20% and 30%, respectively, compared with HIV-1-infected subjects with normal hepatic function. The effect of hepatic impairment on low-dose ritonavir, however, showed pharmacokinetic changes were more pronounced in the moderate impairment group (181% and 221% increase in AUC and Cmax, respectively) than in the mild impairment group (39% and 61% increase in AUC and Cmax, respectively) [45]. In severe hepatic impairment it is likely to have further significantly increased exposure and would not be recommended due to risk of hepatotoxicity even with short durations, largely due to the presence of ritonavir twice daily.
No dose reduction is needed in mild to moderate hepatic impairment; however, frequent monitoring of LFTs would be recommended.
3.4 Remdesivir
Remdesivir is a nucleotide analogue with broad-spectrum antiviral activity. In vitro it is effective against filoviruses and coronaviruses. Remdesivir is metabolised to the pharmacologically active nucleoside triphosphate metabolite (GS-441524). The recently available FDA and EMA prescribing information describe remdesivir to have linear pharmacokinetics, with remdesivir and GS-441524 being mainly renally excreted—49% and 10%, respectively, which is 74% of the total administered dose [46,47,48]. There is limited data available about the pharmacokinetics of remdesivir or dosing in special populations.
Prior to obtaining the licence, remdesivir was used as part of a compassionate use programme or via clinical trials for the treatment of COVID-19 [49], with patients treated for 10 days intravenously (200 mg loading dose followed 100 mg daily). Remdesivir was granted an Emergency Use Authorization (EUA) by the FDA on 2 May 2020 for treatment of patients hospitalised with COVID-19 [47], followed by a full FDA licence on 22 October 2020. On 6 July 2020, the EMA granted an EUA [48].
3.4.1 Renal Recommendations
Both EU and US licences state remdesivir should not be used in patients with estimated glomerular filtration rate (eGFR) < 30 mL/min. Remdesivir is formulated with sulfobutylether-β-cyclodextrin sodium salt (SBECD), which has reduced clearance and therefore accumulates in patients with renal impairment. Hoover et al. previously studied the accumulation of SBECD in patients with renal impairment and although it accumulates, its safety and toxicity profile seem unaffected [50]. In addition, it could also be that the main metabolite (GS-441524) accumulates in patients with eGFR < 30 mL/min as it is mainly renally cleared. Currently, there are no case reports or safety data in patients with eGFR < 30 mL/min and only limited data on the safety of the co-formulated sodium salt that accumulates in renal impairment; therefore, no recommendations can be made for use in these populations (see Table 1).
3.4.2 Hepatic Recommendations
The pharmacokinetics of remdesivir have not been evaluated in patients with hepatic impairment. However, it is shown that only 18% of the administered dose is recovered in faeces [47]. Remdesivir should not be commenced in patients with ALT ≥ 5 × ULN at baseline. It should be discontinued if ALT rises to ≥ 5 times ULN during treatment, although it can be restarted if ALT normalises [47]. Consideration should be given to stopping remdesivir if ALT elevation is accompanied by signs or symptoms of liver impairment. In study GS-US-540-5773 in 397 subjects with severe COVID-19 treated with remdesivir for 5 (n = 200) or 10 days (n = 197), 19/385 (5%) had grade 3 liver abnormalities and 9/385 (2%) had grade 4 [47] found during treatment. In the absence of contraindications and because it is mainly renally cleared, no dose change is advised at present in patients with hepatic impairment, but treatment should be reviewed on a case-by-case basis with advice from specialist hepatologists considered.
3.5 Favipiravir
Favipiravir is an antiviral drug registered in Japan with activity against coronaviruses. Favipiravir has extensive metabolism to two metabolites; M1 is mainly formed by aldehyde oxidase and xanthine oxidase and M2 is a glucuronide. Favipiravir used for the treatment of influenza is dosed at 1600 mg twice daily on Day 1, followed by 600 mg twice daily on Days 2–5 [51, 52]. For COVID-19 treatment, favipiravir is studied in different dosages varying from a maintenance dose of 200–600 mg twice daily for 10 days, with different loading dosages of 1600, 1800, and 2400 mg [51, 53].
3.5.1 Renal Recommendations
Favipiravir is mainly renally excreted (90.5%), of which the majority exists as M1 (82.0–92.4%). In the global phase III study, no patients with eGFR < 30 mL/min were included, one patient with eGFR 30–50 mL/min was included and there were 30 patients with eGFR 50–80 mL/min [51]. No PK data about the group of patients with eGFR 50–80 mL/min is reported. The label states M1 is increased 2.5 times in patients with moderate renal impairment; however, this is based on the clearance of favipiravir in one patient. Any toxicity of favipiravir is likely related to M1, as it accumulates in patients with renal impairment. However, no data is available to make any statement of safety in patients with renal impairment or dependent on RRT.
The manufacturer cites non-clinical pharmacokinetic data from the toxicity studies showing no observed adverse effects. They state it is unlikely that severe events would occur due to increased M1 levels; however, this is just based on data in one patient.
In addition, favipiravir increases uric acid levels in urine, which should be further investigated in patients with renal impairment; this is described in Mishima et al., 2020 [54]. In the phase III study, with a short treatment duration similar to use in COVID-19, adverse events in total occurred in 13/30 (43.4%) patients with mild renal impairment and in 110/363 (30.3%) patients with normal renal function. Overall, there is not enough data to recommendation use for patients with renal impairment or RRT [52].
3.5.2 Hepatic Recommendations
There has been one human study of favipiravir that looked specifically at hepatic impairment, clinical trial US109 [55]. Doses were reduced in severe hepatic impairment (CPT C). Mild and moderate hepatic impairment (CPT A and CPT B) resulted in 2.1- and 2.0-fold increases in favipiravir exposures, respectively, following single doses on Day 1. Severe hepatic impairment resulted in a 3.7-fold increase in total systemic exposure on Day 1, and 6.3- and 2.1-fold increases in AUC0–12 and peak exposure, respectively, following multiple oral doses on Day 3. Mean half-life (t½) values of favipiravir were generally longer in subjects with mild, moderate and severe hepatic impairment compared with healthy volunteers. Approximately 45.4%, 44.1% and 45.8% of the total favipiravir dose was recovered as the M1 metabolite in urine in subjects with mild, moderate and severe hepatic impairment, respectively, compared with 58.3%, 63.2% and 75.1% recovered from their respective healthy matches. Another recent study looked at treatment in CPT A patients with COVID-19 [56]. Despite earlier findings, dosing in CPT A patients was comparable for those with normal hepatic function. This study will provide information on whether increases in exposure in hepatic impairment could be an issue.
Previously, no effects on the liver were observed in monkeys treated with favipiravir for 6 weeks at a dose equivalent to above the maximum exposure in humans. In consideration of these results and currently available clinical data, the use of favipiravir in patients at the proposed dosage regimen and possible increases in exposure is unlikely to have serious effects on the liver [52]. Based on these in vitro findings, we recommend the doses from the original healthy volunteer study [55] as detailed in Table 3 with duration to 14 days in CPA patients as per ongoing study in COVID-19 in this patient group. Extension beyond 5 days can be considered in CPT B and CPT C patients.
3.6 Hydroxychloroquine
Hydroxychloroquine and chloroquine are antiviral/immune modulators that are used for the treatment and prophylaxis of malaria, rheumatoid arthritis, lupus erythematodes, photo dermatosis and liver amoebiasis. Since chloroquine was only used in early COVID-19 studies we are not considering it in this review. As of November 2020, there remains 101 actively recruiting studies on hydroxychloroquine on ClinicalTrials.gov and despite some published data, it remains the most studied drug for COVID-19, particularly in resource-poor countries as it is cheap and readily available. Hydroxychloroquine dosages begin at 400–600 mg/day, followed by daily dosages of 200–400 mg. For COVID-19 treatment, high dosing regimens have been used, with the mean dose studied being 596 mg [57] as well as prophylactic [58] dosages of 100 mg/day or 300 mg/week [26, 59, 60].
3.6.1 Renal Recommendations
Hydroxychloroquine has a very large volume of distribution with extreme accumulation in cells and tissues and a long elimination half-life. Jallouli et al. [61] studied 22 patients with systemic lupus erythematosus and chronic renal insufficiency (median serum creatinine clearance 52 mL/minute (range 23–58 mL/minute) who received 400 mg/day hydroxychloroquine. The median blood concentration was significantly higher than in patients with normal renal function (n = 509): 1338 ng/mL (range 504–2229 ng/mL]) versus 917 ng/mL (range 208–3316 ng/mL) but was still considered within the therapeutic window (high normal). Hydroxychloroquine does not appear to be dialysed. Plasma concentrations before and after dialysis were not significantly altered and hydroxychloroquine was not detected in the dialysate in three patients on dialysis (all on hydroxychloroquine therapy for at least 6 months) [61]. The FDA drug label states that no dose adaptations should be made in patients with impaired renal function as there is no correlation between creatinine clearance and renal clearance of hydroxychloroquine [62]. Therefore, patients with renal impairment and on RRT can be treated with standard-dose hydroxychloroquine without dose adjustment. It is recommended to monitor (short term) cardiotoxicity (i.e. QT prolongation).
The studies cited above were mainly done because of the severe long-term toxicity associated with hydroxychloroquine [63]. Retinopathy and cardiomyopathy risk increase in patients with chronic kidney disease, likely potentiated with longer term use. These toxicities are less likely to occur with COVID-19 treatment of only 5–14 days but may be of importance if hydroxychloroquine is used as prophylaxis for COVID-19. A risk–benefit analysis should be considered due to possible severe toxicity. These recommendations reflect guidance on short-term treatment courses.
3.6.2 Hepatic Recommendations
Hydroxychloroquine is metabolised by several CYP enzymes in the liver with desethylhydroxychloroquine being an active metabolite. SmPC and FDA prescribing information caution use in patients with existing liver disease and/or concomitant use with hepatotoxic drugs [62, 64]. Hydroxychloroquine is known to accumulate in the liver [65] and animal studies have shown that accumulation occurs rapidly in the first 2 weeks of treatment [66]. However, in a study by Tett et al. [67], hydroxychloroquine was found to have a low hepatic extraction ratio, indicating that a reduction in liver blood flow in cirrhosis may not directly result in increased exposure to the drug. Hydroxychloroquine is also known to be hydrophilic [68] and this should be a consideration in patients with ascites and decompensated cirrhosis. The manufacturer recommends that consideration should be given to dose reduction with or without estimation of plasma levels to guide dosing [64]; however, therapeutic drug monitoring is unlikely to have utility in the context of COVID-19 treatment. The American College of Rheumatology recommendations contraindicate the use of hydroxychloroquine in CPT C liver disease [69]; again, these recommendations are made with the assumption of longer-term dosing.
In summary, despite risks that accumulation in liver may be reduced in the setting of COVID-19 treatment due to the short treatment length, the cautions and risks for use in hepatic impairment suggest that hydroxychloroquine is not a preferred agent in this patient population. If treatment was to proceed, a conservative approach may be to use a loading dose with a reduction of 50% for maintenance dosing in patients with advanced liver disease (CPT C) and a maximum of no more than 400 mg per day. Other risks for toxicities such as concomitant QT prolongation drugs may also indicate need for dose reduction in patients with mild/moderate liver disease. Baseline monitoring of liver function is required [70] and ongoing monitoring of toxicities is essential.
3.7 Azithromycin
Azithromycin is a macrolide antibiotic licensed for use in treatment of various infections such as community-acquired pneumonia, bronchitis, soft tissue infections and uncomplicated genital infections due to Chlamydia trachomatis and Neisseria gonorrhoeae. Doses used are in the range of 1 g as a single dose to 500 mg once daily for 3 days. To date, in COVID-19 it continues as an arm in many multi-centre clinical trials, including RECOVERY, at doses of 500 mg daily on Days 1–5 or reducing to 250 mg daily for Days 2–5 [26].
3.7.1 Renal Recommendations
Azithromycin undergoes minimal renal elimination (6% unchanged following oral dosing, 11–14% unchanged following IV administration) [24]; the standard doses can be used in renal impairment. However, in severe renal impairment (GFR < 10 mL/min), it has been noted that there is increased exposure by 33–35% and therefore caution is advised. For patients undergoing haemodialysis or continuous veno-venous haemofiltration, the dialysability of azithromycin is unknown and it is known not to be removed in peritoneal dialysis. Therefore, standard doses can be used, proceeding with caution and monitoring for adverse effects, such as QT prolongation.
3.7.2 Hepatic Recommendations
The liver is the main site for metabolism of azithromycin and 50% is excreted unchanged in the bile, although some inactive metabolites are also found [24]. Azithromycin is known to rarely cause acute liver injury, often manifested as a self-limiting cholestatic hepatitis. Any appearance of jaundice or other liver dysfunction should lead to a prompt discontinuation of azithromycin [23, 71].
Azithromycin is not recommended in severe liver disease due to significant hepatic metabolism and the liver being the principal route of elimination. Mazzei et al. [72] found that pharmacokinetics did not differ significantly in patients with CTP A or B cirrhosis and therefore standard doses can be used in these patient groups. Dosing in CPT C patients, given the short courses used in COVID-19, could be considered with special hepatology input and monitoring of QTc prolongation.
3.8 Ribavirin
Ribavirin is a guanosine nucleoside analogue, approved for use in combination with direct acting antivirals or pegylated-interferon 2a or 2b for treatment of hepatitis C. In the treatment of hepatitis C, ribavirin is given orally and is dosed dependent on weight, ranging from 800 mg to 1200 mg daily in divided doses. In COVID-19, several ribavirin dosages are studied: 500 mg twice or three times daily intravenously or orally 400 mg twice daily in combination with lopinavir/ritonavir [73, 74].
3.8.1 Renal Recommendations
Ribavirin has been extensively studied and used in patients with impaired renal function. As ribavirin is primarily renally cleared (62%), drug exposure and related toxicities (anaemia) increase with declining renal function. Anaemia should be taken into account when choosing the dose (with low baseline haemoglobin, a reduced dose might be indicated) [75, 76]. Ribavirin is not cleared by haemodialysis [75]. Dose reductions are required for patients with impaired renal function and for those on RRT and these recommendations are outlined in Table 2.
3.8.2 Hepatic Recommendations
In single-dose control studies, no difference in pharmacokinetic parameters were noted when administered in patients with liver dysfunction classed by CPT score A, B or C [75]. Much of the use of ribavirin is in patients with underlying liver disease and it is not associated with liver injury. However, it is associated with a dose-dependent red cell haemolysis which can be accompanied by a mild increase in indirect bilirubin. In general, this effect is usually benign and resolves quickly on cessation of ribavirin [23, 77]. Full-dose ribavirin can be used in CPT A with caution and in CPT B and CPT C with appropriate dose reduction based on eGFR if there is assocated renal impairment.
3.9 Interferon-β
Interferon-β is produced by recombinant technology and is a cytokine with antiviral, immunomodulatory and antiproliferative properties. Interferon-β is available as 1a and 1b and pegylated β-1a. The letter identifies the placement of amino acid sequences at positions 1 and 17 and indicates if glycosylation is present [24]. Interferon-β is approved for use in multiple sclerosis where all of these preparations are used by either subcutaneous or intramuscular administration. In COVID-19 clinical trials, it has been used in both nebulised and intravenous forms [26, 60].
3.9.1 Renal Recommendations
It is estimated that approximately 40% of interferon-β is excreted renally. Increased exposure of interferon-β may be expected, particularly in severe renal impairment, which may increase the risk of dose-related adverse effects such as myelosuppression or hepatotoxicity [78]. The interferon molecule is too large to be dialysed and will not undergo renal degradation. In patients with severe renal dysfunction or those on RRT, it is recommended to use interferon-β with caution, with monitoring of renal function [22].
3.9.2 Hepatic Recommendations
Hepatic dysfunction has been noted in patients treated with interferons for prolonged courses for indications such as multiple sclerosis [79]. This dysfunction is usually seen as asymptomatic increase in liver enzymes, although rare cases of fulminant liver failure have been noted with mechanism of injury not known [23]. Therefore, the commercially available products advise caution for use in patients with established hepatic disease, chronic alcohol misuse and/or baseline increase in ALT (2.5 × ULN). Baseline and continued monitoring of transaminases is advised, and dose reductions are advised if ALT increased by 5 × ULN. Treatment should be discontinued if the patient develops jaundice or clinical symptoms of liver disease [80, 81].
In treatment of COVID-19 where short finite courses are proposed, interferon-β could be used with caution in patients with a baseline increase in serum ALT above 2.5 × ULN and after a careful assessment of balance of risks versus benefits if ALT is >5 × ULN. Prescribing could be considered in patients with established cirrhosis (CPT A) but use in decompensated cirrhosis is not advised.
3.10 Tocilizumab
Tocilizumab is an anti-human IL-6 receptor monoclonal antibody (mAb) approved for the treatment of rheumatoid arthritis and systemic juvenile idiopathic arthritis. Patients infected with COVID-19 experience an elevation of IL-6 (cytokine storm). It is usually dosed between 4 and 12 mg/kg every 2 or 4 weeks depending on indication, and is being studied for COVID-19 at 4- to 8-mg/kg single doses, with one additional dose if clinically indicated [60, 82]. As of November 2020, despite varying reports of beneficial effect, tocilizumab remains an active arm in many global clinical trials.
3.10.1 Renal Recommendations
Tocilizumab is not metabolised or excreted by the kidneys, instead it is broken down into peptides and amino acids and recycled, comparable with IgG; therefore, it is not expected to be affected by reduced renal function. No formal registration studies were conducted for renal impairment, although pharmacokinetics were not different in patients with mild renal impairment (creatinine clearance between 50 and 80 mL/min) [83, 84]. In addition, the large molecular weight of tocilizumab prevents clearance via glomerular filtration or RRT [85]. Based on this knowledge, no dose reductions are necessary in patients with impaired renal function or RRT.
3.10.2 Hepatic Recommendations
Tocilizumab has not been studied in patients with hepatic impairment, but it is expected to have minimal hepatic metabolism. No recommendations are in the label regarding dose adjustments in patients with established liver disease.
Tocilizumab may cause hepatoxicity reversible on discontinuation and should be used in caution in the setting of COVID-19 in those already presenting with acute liver injury. A total of 4171 patients on tocilizumab were evaluated in the setting of rheumatoid arthritis and ALT and AST elevations greater than the ULN occurred in 70.6% and 59.4% of patients, respectively, and > 5 × ULN in 2.9% and 0.9% of patients. Most elevations occurred during the first year of treatment [86]. The authors acknowledge the significantly shorter course used in COVID-19; however, close monitoring of LFTs are recommended for any patient starting tocilizumab where baseline transaminases are > 1.5 × ULN. The manufacturer recommends withholding treatment if LFTs rise beyond 3 × ULN, and to discontinue if they rise beyond 5 × ULN [83, 84].
mAbs have been thought not to be affected by chronic hepatic impairment due to their alternative metabolism. However, in a review of the pharmacokinetics of mAbs in hepatic impairment considering the available data from drug licences, published studies and pharmacokinetic modelling, Sun et al. [87] found a small amount of reduced drug exposure for some mAbs in patients with mild hepatic impairment, and a more significant reduction in exposure in moderate hepatic impairment. No specific data was found for tocilizumab and disease severity was not fully described, where we know that clearance of mAbs is higher in patients with more severe disease or lower albumin. More studies are required to explore this concept.
In summary, it is difficult to make a recommendation on the dosing of tocilizumab in chronic hepatic impairment. As there is no pharmacokinetic data available, it is unclear whether there is the potential for altered drug exposure, whilst there is also a risk of drug-induced hepatic injury. If use is considered necessary in hepatic impairment, consider using a full dose, provided AST and ALT are not significantly deranged (e.g. not > 2 × ULN) and the patient is not thrombocytopenic.
3.11 Anakinra
Anakinra is an analogue of the human IL-1 receptor antagonist. It blocks the activity of IL-1 by competitively inhibiting IL-1 binding to the IL-1 type I receptor (IL-1RI), which is expressed in a wide variety of tissues and organs. It is used in the treatment of rheumatoid arthritis and other inflammatory conditions. For rheumatoid arthritis, it is dosed at 100 mg/day subcutaneously, and 1–2 mg/kg/day in most other conditions [88, 89]. It is being investigated at a variety of doses for COVID-19, including 5 mg/kg twice daily intravenously, 100 mg 6-h intravenously after a 300 mg loading dose, and 100 mg subcutaneously once or twice daily [90, 91].
3.11.1 Renal Recommendations
Yang et al. [92] studied anakinra pharmacokinetics in patients with different stages of renal disease, including patients on RRT. They described the clearance of anakinra to be directly related to renal function and that dialysis (continuous ambulatory peritoneal dialysis/haemodialysis [CAPD/HD] < 2.5%) did not remove anakinra. They simulated every-other-day dosing and suggested that this might be appropriate for these patients. Comparable data is described in the drug label showing that subjects with eGFR 50–80 mL/min and eGFR 30–49 mL/min had reduced clearance of 16% and 50%, respectively. In addition, patients with eGFR < 30 mL/min and end-stage renal disease had declined clearance of 70% and 75%, respectively. For patients with an eGFR >30 mL/min, 100% of the dose is recommended and for eGFR <30 mL/min, a reduction to the same dose administered on alternate days [88].
3.11.2 Hepatic Recommendations
Studies in hepatic impairment are limited. The safety and efficacy have not been studied in patients with AST or ALT of ≥1.5 × ULN. Twelve patients with moderate hepatic dysfunction (CPT B) were given a single 1-mg/kg intravenous dose and pharmacokinetic parameters were not substantially different from healthy volunteers [88]. Therefore, no dosage adjustment is required in patients with hepatic impairment, with caution recommended in patients with CPT C cirrhosis or those with ALT elevation.
3.12 Sarilumab
Sarilumab is a recombinant human monoclonal antibody that blocks the activity of pro-inflammatory cytokines via IL-6 receptors. It is used in the treatment of moderate to severe rheumatoid arthritis. The usual dosage is 200 mg every 2 weeks via subcutaneous injection. Sarilumab is being investigated for COVID-19 at 200-mg and 400-mg single doses [60, 93,94,95]. Less commonly, protocols may include a further dose 24–48 h after the initial dose.
3.12.1 Renal Recommendations
As with tocilizumab, sarilumab is broken down to peptides and amino acids via catabolic pathways rather than via renal or hepatic pathways. In patients with mild or moderate renal impairment, pharmacokinetics of sarilumab were not affected. Patients with severe renal impairment were not reported in the drug label. No dose adjustment is recommended in renal impairment [96].
3.12.2 Hepatic Recommendations
There is limited evidence available for treating patients with hepatic impairment with sarilumab. Treatment is commonly associated with a reversible liver enzyme derangement which in clinical studies did not result in clinically significant hepatic injury. An ALT increase occurred in 48% of rheumatoid arthritis patients treated with sarilumab [97]. The licence recommends that it should not be initiated in patients with an AST or ALT > 1.5 × ULN [96]; however, as single doses are predominantly used in COVID-19, exclusion criteria in most clinical trial protocols include ALT or AST > 5 × ULN [96].
As the drug label does not include patients with hepatic impairment, and no data have been reported for sarilumab in the review by Sun et al. [87] of mAbs in hepatic impairment, It is unclear whether there could be an alteration in drug exposure in patients with significant hepatic impairment. As a result, it is difficult to make a dosage recommendation in this population. If treatment is required in hepatic impairment, consideration should be given to using full-dose sarilumab provided that ALT and AST are not significantly elevated (e.g. not > 2 × ULN) and there is no significant thrombocytopenia. These parameters, as with all immune modulators, should be reviewed in the context of the critical care setting.
4 Discussion
Data suggests that liver disease appears to be a risk factor for mortality in hospitalised patients with COVID-19 [12]; this includes longstanding organ damage or acute onset. Several physiological changes occur in a cirrhotic liver affecting the process of drug handling. These include liver cell necrosis, portal shunting of the blood, reduced production of drug-binding proteins (such as albumin and α1-acid glycoprotein, increasing unbound fractions of drug), abnormal drug volume of distribution, altered drug elimination and altered drug metabolism [4, 98]. Therefore, understanding detailed hepatic drug metabolism can provide a rationale for dosage adjustment in patients with hepatic impairment and the pharmacokinetic parameters of each drug were examined when making recommendations. Increased drug concentrations in patients with liver disease may result from different mechanisms, many of which have not been properly studied in these repurposed medications and further data in these areas would be welcomed. These include decreased clearance, increased absorption due to an altered vasculature around the stomach and intestines, or both. Associated renal failure and concomitant drug–drug interactions must also be considered, and it should be noted that liver disease not only affects pharmacokinetics but also pharmacodynamics, as with the worsening anaemia seen with ribavirin.
The impairment of drug metabolism is proportional to the degree of liver dysfunction, as illustrated with lopinavir/ritonavir, where a 39% and 181% increase in ritonavir AUC is seen in mild and moderate hepatic impairment, respectively [41]. Patients with compensated cirrhosis with normal synthetic function are likely to have minimal impairment of drug metabolism compared with patients with decompensated cirrhosis, and these recommendations reflect this. Despite this proportional effect, prescribing any drugs with potential hepatotoxicity in the cirrhotic population should be done with caution. Any drug-induced liver injury may precipitate hepatic decompensation in cirrhotic patients with previously normal synthetic function. A hepatologist should be consulted regarding the use of any of these medications in a patient with advanced liver disease. Additionally, it is important to consider drug–drug interactions [19] when instituting any treatment in liver transplant recipients with COVID-19. Despite the complexities associated with hepatic impairment, and the absence of data, particularly in advanced liver disease, these recommendations acknowledge the likely decreased risk of one-off or short-course dosing in COVID-19. Treatment decisions should be made on a case-by-case basis in patients with decompensated liver disease, which even in the absence of COVID-19 is associated with high short-term mortality.
Compared with hepatic impairment, the changes occurring in renal impairment are less complicated. Firstly, when the filtering capacity of the kidney decreases, drugs that are significantly dependent on renal clearance (glomerular filtration) will normally have decreased clearance resulting in higher plasma concentrations (unless there are any other compensatory clearance pathways). This is apparent with anakinra and ribavirin (predominantly renally cleared) where there is increased exposure as renal function decreases. Dose alterations are therefore required in these circumstances. An estimated glomerular filtration rate (eGFR) can be calculated using different equations such as Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) or Modification of Diet in Renal Disease (MDRD), although it is acknowledged that there are limitations here with respect to the elderly or obese, for example. Active tubular secretion and tubular reabsorption are also important for the renal clearance of drugs; however, these factors are not directly measured with eGFR.
Dialysis and other forms of RRT may be indicated in the COVID-19 population as previously mentioned. Flow, pore size of the membrane, and the characteristics of whether drugs are removed with dialysis or not were identified prior to making recommendations. Only unbound concentrations of small molecules can be dialysed and most biologics (due to being large proteins) are not dialysable. Additionally, water solubility and the volume of distribution are important. For example, ribavirin is mainly trapped in the red blood cell and only a small part is unbound and available for dialysis. This unbound fraction is removed effectively with haemodialysis (50%); however, this is not clinically relevant as the drug remains available in another compartment [75].
Physiologically based pharmacokinetic modelling (PBPK) is a tool which can be used to better inform on dosing recommendations in organ impairment. Anatomical, physiological and molecular changes related to liver and renal impairment have been quantitatively described and integrated into mechanistic pharmacokinetic modelling [99, 100]. The application of PBPK models can support the prediction of drug distribution in patients with various degrees of organ impairment and consequently allow the rational identification of suitable dosing regimens to avoid potential toxicities. The combination of multiple organ impairments can result in multifactorial effects on drug distribution that can complicate the application of PBPK modelling, which should be limited to scenarios that are fully characterised.
It should be noted that the majority of data obtained for this paper are from patients who did not have COVID-19. Dosages of repurposed antivirals that have been used in COVID-19 are largely based on exposure–response relationships from other viruses such as HIV and influenza. Even without the current pandemic, data is limited in these special populations who are often only studied in very small numbers, if at all. The presence of COVID-19 itself could independently influence the clearance and thus exposure (efficacy/toxicity) of drugs, and as yet there is minimal data in this context. In addition, COVID-19 patients admitted to the ICU that are acutely unwell will have altered pharmacokinetics, which has been well described in other critically ill patient populations with hepatic and renal dysfunction. Oxidative metabolism is the main clearance pathway for many prescribed medications and there is increasing recognition of the importance of decreased activity of the hepatic cytochrome P450 system in critically ill patients [101]. Renal failure in critical care is of equal importance with both altered filtration and secretion clearance mechanisms affecting the removal of parent drugs and their active metabolites. Use of repurposed therapies for COVID-19 in critical care should be carried out with particular caution.
5 Conclusion
There is growing evidence indicating hepatic and renal impairment, in both acute and chronic settings, are a common occurrence in the treatment of COVID-19. Dosing remains complex and often data is lacking even in drugs like hydroxychloroquine that have been in use for over 60 years. These recommendations review all available data. Where dosing has been suggested for advanced liver or kidney disease, often data is minimal, and prescribing should be undertaken in consultation with experienced hepatologists or nephrologists for these populations.
References
Ronco C, Reis T. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat Rev Nephro., 2020.
Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–30.
Marcellin P, Kutala BK. Liver diseases: A major, neglected global public health problem requiring urgent actions and large-scale screening. Liver Int. 2018;38(Suppl 1):2–6.
Qi X. COVID-19 in patients with pre-existing cirrhosis (COVID-Cirrhosis-CHESS2002): a multicentre observational study. 2020. https://clinicaltrials.gov/ct2/show/NCT04329559.
Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506.
Chen N, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Fan Z, et al. Clinical features of COVID-19-related liver damage. Clin Gastroenterol Hepatol. 2020.
Boettler T, et al. Care of patients with liver disease during the COVID-19 pandemic: EASL-ESCMID position paper. JHEP Rep. 2020;2(3):100113.
Phipps MM, et al. Acute liver injury in COVID-19: prevalence and association with clinical outcomes in a large US Cohort. Hepatology. 2020.
Fu Y, et al. Clinical features of COVID-19-infected patients with elevated liver biochemistries: a multicenter, retrospective study. Hepatology, 2020.
Liu W, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl). 2020;133(9):1032–8.
Collaborative TO, Williamson EW, Bhaskaran AJ, Bacon KJ, Bates S, Morton C, Curtis CE, Mehrkar HJ, Evans A, Inglesby D, Cockburn P, Mcdonald J, MacKenna HI, Tomlinson B, Douglas L, Rentsch IJ, Mathur CT, Wong R, Grieve A, Harrison R, Forbes D, Schultze H, Croker A, Parry RT, Hester J, Harper F, Perera S, Evans R, Smeeth S, Goldacre GB. OpenSAFELY: factors associated with COVID-19-related hospital death in the linked electronic health records of 17 million adult NHS patients. 2020.
Collaboration GCKD. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10225):709–33.
Goldfarb DS, et al. Impending shortages of kidney replacement therapy for COVID-19 patients. Clin J Am Soc Nephrol. 2020.
Wang D, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel coronavirus-infected pneumonia in Wuhan, China. JAMA, 2020.
Aggarwal S, et al. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): Early report from the United States. Diagnosis (Berl). 2020;7(2):91–6.
Volunteers A-N, et al. Caution on kidney dysfunctions of COVID-19 patients.
Pei G, et al. Renal involvement and early prognosis in patients with COVID-19 pneumonia. J Am Soc Nephrol. 2020.
Liverpool, U.o. COVID 19 Drug Interactions. 8/5/20 8/5/20]. https://www.covid19-druginteractions.org/.
Global Coronavirus COVID-19 Clinical Trial Tracker. 10/04/2020]. hhttps://covid19-trials.com/.
Zeitlinger MAK, Birgit CP, Brüggemann R, De Cock, Pieter, Felton, Timothy, Hites, Maya, Le, Jennifer, Luque, Sonia, MacGowan, Alasdair, Marriott, Deborah, Muller, Anouk E, Nadrah, Kristina, Paterson, David, Standing, Joseph F, Telles JP, Wölfl-Duchek, M, Thy MR, Jason A. Pharmacokinetics-pharmacodynamics of antiviral agents used to treat SARS-CoV-2 and their potential interaction with drugs and other supportive measures: a comprehensive review by the PK/PD of Anti-Infectives Study Group of the European Society of Antimicrobial Agents. 2020. p. 178.
Ashley C, Dunleavy A. The Renal Drug Handbook: The Ultimate Prescribing Guide for Renal Practitioners, vol. 5. Milton Park: Taylor & Francis Ltd.; 2018.
National Institute of Diabetes and Digestive and Kidney Diseases (U.S.), LiverTox : clinical and research information on drug-induced liver injury. 2012, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda (MD). p. 1 online resource (1 PDF file)
Truven Health Analytics Inc. and Micromedex Inc., Micromedex gateway. 2011, Truven Health Analytics.
Aspen. Dexamethasone 2mg tablets, Summary of Product Characteristics. 2020. https://www.medicines.org.uk/emc/product/5411/smpc. Accessed 10 Nov 2020.
Horby P. Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial. 2020. . 8 May 2020]. www.recoverytrial.net. Accessed 10 Nov 2020.
Workman RJ, Vaughn WK, Stone WJ. Dexamethasone suppression testing in chronic renal failure: pharmacokinetics of dexamethasone and demonstration of a normal hypothalamic-pituitary-adrenal axis. J Clin Endocrinol Metab. 1986;63(3):741–6.
Kawai S, Ichikawa Y, Homma M. Differences in metabolic properties among cortisol, prednisolone, and dexamethasone in liver and renal diseases: accelerated metabolism of dexamethasone in renal failure. J Clin Endocrinol Metab. 1985;60(5):848–54.
Cummings DM, et al. Characterization of dexamethasone binding in normal and uremic human serum. DICP. 1990;24(3):229–31.
Pandit SR, Vesole DH. Management of renal dysfunction in multiple myeloma. Curr Treat Options Oncol. 2003;4(3):239–46.
Zhao B, et al. Evaluation of the efficacy of steroid therapy on acute liver failure. Exp Ther Med. 2016;12(5):3121–9.
Heneghan MA, et al. Autoimmune hepatitis. Lancet. 2013;382(9902):1433–44.
Tomlinson ES, et al. Dexamethasone metabolism in vitro: species differences. J Steroid Biochem Mol Biol. 1997;62(4):345–52.
REYATAZ (atazanavir) capsules, US Prescribing Information. BMS.
Reyataz 300mg Hard Capsules, Summary of Product Characteristics. Last updated on emc: 25 Feb 2019, BMS.
EACS Guidelines version 10.0. November 2019.
Izzedine H, et al. Atazanavir: a novel inhibitor of HIV-protease in haemodialysis. Nephrol Dial Transplant. 2005;20(4):852–3.
Guaraldi G, et al. A pilot study on the efficacy, pharmacokinetics and safety of atazanavir in patients with end-stage liver disease. J Antimicrob Chemother. 2008;62(6):1356–64.
Guaraldi G, et al. Efficacy and safety of atazanavir in patients with end-stage liver disease. Infection. 2009;37(3):250–5.
Ray JE, et al. Therapeutic drug monitoring of atazanavir: surveillance of pharmacotherapy in the clinic. Br J Clin Pharmacol. 2005;60(3):291–9.
Kaletra 200 mg/50 mg film-coated tablets summary of product characteristics. 2019: AbbVie Ltd.
Cao B, et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020;382(19):1787–99.
Kaletra, US Prescribing information. 2019, Abbvie.
Gupta SK, et al. The pharmacokinetics and pharmacogenomics of efavirenz and lopinavir/ritonavir in HIV-infected persons requiring hemodialysis. AIDS. 2008;22(15):1919–27.
Peng JZ, et al. Pharmacokinetics of lopinavir/ritonavir in HIV/hepatitis C virus-coinfected subjects with hepatic impairment. J Clin Pharmacol. 2006;46(3):265–74.
(EMA) E.MA. Summary on compassionate use: Remdesivir, Gilead. 2020 12/5/2020]. https://www.ema.europa.eu/en/documents/other/summary-compassionate-use-remdesivir-gilead_en.pdf. Accessed 10 Nov 2020.
Emergency Use Authorisation (EUA) of remdsivir (GS-5734™). 2020, Gilead.
Gilead. Veklury (Remdesivir) 100mg concentrate for solution. 2020. www.medicines.org.uk/emc/product/11596/smpc. Accessed 10 Nov 2020.
Grein J, et al. Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med. 2020.
Hoover RK, et al. Clinical Pharmacokinetics of Sulfobutylether-β-Cyclodextrin in Patients With Varying Degrees of Renal Impairment. J Clin Pharmacol. 2018;58(6):814–22.
Du YX, Chen XP. Favipiravir: pharmacokinetics and concerns about clinical trials for 2019-nCoV Infection. Clin Pharmacol Ther. 2020.
Avigan (favipiravir) Tablet 200 mg. 2011, Toyama Chemical Co., Ltd.
Chen CZY. Favipiravir versus Arbidol for COVID-19: a randomized clinical trial. 2020.
Mishima E, et al. Uric Acid Elevation by Favipiravir, an Antiviral Drug. Tohoku J Exp Med. 2020;251(2):87–90.
Preston R. Pharmacokinetics of favipiravir in volunteers with hepatic impairment. 2015. https://clinicaltrials.gov/ct2/show/NCT01419457.
Fujifilm Pharmaceuticals U.S.A., I. Study of the Use of Favipiravir in Hospitalized Subjects With COVID-19. 2020. https://clinicaltrials.gov/ct2/show/NCT04358549.
Mehra, M., et al., Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet. 2020.
Gendrot M, et al. Chloroquine as a prophylactic agent against COVID-19? Int J Antimicrob Agents. 2020;55(6):105980
Zhou D, Dai SM, Tong Q. COVID-19: a recommendation to examine the effect of hydroxychloroquine in preventing infection and progression. J Antimicrob Chemother. 2020.
Bonten M. Randomised, embedded, multi-factorial, adaptive platform trial for community acquired pneumonia (REMAP-CAP) trial. 2020 8 May 2020]. https://www.remapcap.org/. Accessed 10 Nov 2020.
Jallouli M, et al. Determinants of hydroxychloroquine blood concentration variations in systemic lupus erythematosus. Arthritis Rheumatol. 2015;67(8):2176–84.
Plaquenil Hydroxychloroquine Sulfate Tablets US Prescribing Information. 2017.
Lee JY, et al. Factors associated with blood hydroxychloroquine level in lupus patients: renal function could be important. Lupus. 2013;22(5):541–2.
Plaquenil-Hydroxychloroquine sulfate 200mg Film-coated Tablets, Summary of Product Characteristics. 2020, Zentiva.
Dollery C. Therapeutic drugs. 2nd ed. London: Churchill Livingstone; 1999.
McChesney EW. Animal toxicity and pharmacokinetics of hydroxychloroquine sulfate. Am J Med. 1983;75(1A):11–8.
Tett SE, et al. Bioavailability of hydroxychloroquine tablets in healthy volunteers. Br J Clin Pharmacol. 1989;27(6):771–9.
Warhurst DC, et al. Hydroxychloroquine is much less active than chloroquine against chloroquine-resistant Plasmodium falciparum, in agreement with its physicochemical properties. J Antimicrob Chemother. 2003;52(2):188–93.
Saag KG, et al. American College of Rheumatology 2008 recommendations for the use of nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis. Arthritis Rheum. 2008;59(6):762–84.
FDA. Fact sheet for health care providers. Emergency use Authorisation (EUA) of hydroxychloroquine sulfate supplied supplied from the strategic national stockpile for treatment of COVID-19 in certain hospitalized patients. 2020, U.S. Food and Drug Administration (FDA).
Zentiva. Azithromycin 250mg capsules, Summary of Product Characteristics. 2020. https://www.medicines.org.uk/emc/product/8663/smpc.
Mazzei T, et al. Pharmacokinetics of azithromycin in patients with impaired hepatic function. J Antimicrob Chemother. 1993; 31 Suppl E: 57–63.
Kong, U.o.H. Lopinavir/ritonavir, ribavirin and IFN-beta combination for nCoV treatment. 2020. https://clinicaltrials.gov/ct2/show/NCT04276688
Khalili JS, et al. Novel coronavirus treatment with ribavirin: Groundwork for an evaluation concerning COVID-19. J Med Virol. 2020.
Rebetol 200 mg hard capsules Summary of Product Characteristics. 2019. https://www.medicines.org.uk/emc/product/3832/smpc.
Roche. COPEGUS® (ribavirin) Tablets, US Prescribing Information. Accessed 12/5/2020]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021511s023lbl.pdf.
Wong WM, et al. Temporal patterns of hepatic dysfunction and disease severity in patients with SARS. JAMA. 2003;290(20):2663–5.
Rieckmann P, et al. Haematological effects of interferon-beta-1a (Rebif) therapy in multiple sclerosis. Drug Saf. 2004;27(10):745–56.
Francis GS, et al. Hepatic reactions during treatment of multiple sclerosis with interferon-beta-1a: incidence and clinical significance. Drug Saf. 2003;26(11):815–27.
Rebif 22 micrograms solution for injection in cartridge. 2020, Merck.
Rebif US Prescribing Information. 2014: Pfizer.
A Study to Evaluate the Safety and Efficacy of Tocilizumab in Patients with Severe COVID-19 Pneumonia (COVACTA). 2020 30/03/2020 25/03/2020]. https://clinicaltrials.gov/ct2/show/NCT04320615
Actemra (tocilizumab) injection, for intravenous or subcutaneous use, US Prescribing Information. Genentech Inc. Roche.
RoActemra 20mg/ml Concentrate for Solution for Infusion Summary of Product Characteristics. 2019. https://www.medicines.org.uk/emc/product/6673/smpc. Accessed 10 Nov 2020.
Ternant D, et al. Clinical pharmacokinetics and pharmacodynamics of monoclonal antibodies approved to treat rheumatoid arthritis. Clin Pharmacokinet. 2015;54(11):1107–23.
Genovese MC, et al. Transaminase levels and hepatic events during tocilizumab treatment: pooled analysis of long-term clinical trial safety data in rheumatoid arthritis. Arthritis Rheumatol. 2017;69(9):1751–61.
Sun Q, et al. Does hepatic impairment affect the exposure of monoclonal antibodies? Clin Pharmacol Ther. 2020;107(5):1256–62.
Kineret (Anakinra)100 mg solution for injection in a pre-filled syringe. 2019, Swedish Orphan Biovitrum Ltd.
Kineret® (anakinra) for injection, for subcutaneous use. US Prescribing Information. Swedish Orphan Biovitrum AB.
Delaporte, A. Treatment of COVID-19 patients with anti-interleukin drugs (COV-AID). 2020. https://clinicaltrials.gov/ct2/show/NCT04330638.
Cavalli G, et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020.
Yang BB, Baughman S, Sullivan JT. Pharmacokinetics of anakinra in subjects with different levels of renal function. Clin Pharmacol Ther. 2003;74(1):85–94.
Pinedo M, Efficacy of subcutaneous sarilumab in hospitalised patients with moderate-severe COVID-19 Infection (SARCOVID) (SARCOVID). 2020.
Branch-Elliman W. Sarilumab for patients with moderate COVID-19 disease: a randomized controlled trial with a play-the-winner design. 2020 .https://clinicaltrials.gov/ct2/show/NCT04359901.
Evaluation of the Efficacy and Safety of Sarilumab in Hospitalized Patients With COVID-19. 2020; Available from
Kevzara (Sarilumab) 150 mg solution for injection in pre-filled syringe. 2020; https://www.medicines.org.uk/emc/product/762/smpc. Accessed 10 Nov 2020.
Fleischmann R, et al. Long-term safety of sarilumab in rheumatoid arthritis: an integrated analysis with up to 7 years’ follow-up. Rheumatology (Oxford). 2020;59(2):292–302.
Amarapurkar DN. Prescribing medications in patients with decompensated liver cirrhosis. Int J Hepatol. 2011;2011:519526.
Li R, Barton HA, Maurer TS. A mechanistic pharmacokinetic model for liver transporter substrates under liver cirrhosis conditions. CPT Pharmacometr Syst Pharmacol. 2015;4(6):338–49.
Rhee SJ, et al. Physiologically Based Pharmacokinetic Modelling and Prediction of Metformin Pharmacokinetics in Renal/Hepatic-Impaired Young Adults and Elderly Populations. Eur J Drug Metab Pharmacokinet. 2017;42(6):973–80.
Power BM, et al. Pharmacokinetics of drugs used in critically ill adults. Clin Pharmacokinet. 1998;34(1):25–56.
Czock D, et al. Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet. 2005;44(1):61–98.
FDA. Decadron (dexamethasone) tablets 2mg. US Prescribing Information. 2020. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2004/11664slr062_decadron_lbl.pdf. Accessed 10 Nov 2020.
Wishart DS, et al. DrugBank: a comprehensive resource for in silico drug discovery and exploration. Nucleic Acids Res. 2006;34(Database issue):D668–72.
Avonex US Prescribing Information. 2019: Biogen Inc.
Avonex 30 µg/0.5 mL solution for injection Summary of Product Characteristics. 2019: Biogen Idec Ltd.
Hegen H, Auer M, Deisenhammer F. Pharmacokinetic considerations in the treatment of multiple sclerosis with interferon-β. Expert Opin Drug Metab Toxicol. 2015;11(12):1803–19.
Kent JR, Almond MK, Dhillon S. Azithromycin: an assessment of its pharmacokinetics and therapeutic potential in CAPD. Perit Dial Int. 2001;21(4):372–7.
Alatrakchi N, et al. Strong CD4 Th1 responses to HIV and hepatitis C virus in HIV-infected long-term non-progressors co-infected with hepatitis C virus. AIDS. 2002;16(5):713–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
AB received research grant or personal fees from Abbvie and Gilead outside the submitted work. CM received support from the Adolf and Mary-Mil foundation. DBa received grants from AbbVie, Gilead, Novartis, BHIVA, and EACS during the conduct of the review and grants from Merck and ViiV outside the submitted work. FM received research grant or personal fees from Abbvie, Gilead, Janssen, MSD and ViiV outside the submitted work. KD received educational support from Gilead outside the submitted work. SK received grants from Abbvie, Gilead, Novartis, BHIVA and EACS during the conduct of the review and research grants and speakers’ honoraria from ViiV, Gilead and AbbVie outside the submitted work.ES, DBu, AS, OES, MS and SG declare no support from any organisation for the submitted work, no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
Funding
The preparation and writing of this review received no direct funding.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Code availability
Not applicable.
Authors’ contributions
FM conceived of the study. FM and ES performed the literature review. FM, ES, AB, AS, KD, CM, OES and DBa, SK and MS interpreted the data, FM and ES compiled the tables, FM and ES wrote the manuscript, and all authors revised the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Marra, F., Smolders, E.J., El-Sherif, O. et al. Recommendations for Dosing of Repurposed COVID-19 Medications in Patients with Renal and Hepatic Impairment. Drugs R D 21, 9–27 (2021). https://doi.org/10.1007/s40268-020-00333-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-020-00333-0