Abstract
Purpose of review
Despite the accumulation of a significant amount of data on pediatric headache, few studies have been conducted on its occurrence in children under 7 years of age. Within primary headaches in this age, migraine especially, turns out to be a disorder affecting up to 4% of the general population. An underestimate of its true prevalence can be due to lack of specific diagnostic markers, the frequent difficulty of describing pain in childhood, and the necessity of reliable parents’ reports. Thus, migraine in children under 7 years of age represents an important challenge for clinicians. The objective of this manuscript is to provide a comprehensive review of epidemiologic, clinic, and therapeutic aspects of migraine in this age.
Recent findings
Current literature data show that migraine has some differences, especially in clinical and therapeutic terms, in this age group compared to subsequent ages. Furthermore, some evidences showing that an early onset of migraine may play an unfavorable role in its natural history, suggest an early identification and management of migraine in younger children. Moreover, we highlight the role that factors of prenatal and perinatal development can play in the predisposition and anticipation of migraine onset. Finally, open questions related to the several undefined features of migraine in this age are reported.
Summary
Migraine in this pediatric population is absolutely not rare, represents an importan clinical challenge and probably has a negative predictive role.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Arruda MA, Guidetti V, Galli F, Albuquerque RC, Bigal ME. Primary headaches in childhood: a population-based study. Cephalalgia. 2010;30:1056–64.
Abu-Arafeh I, Russell G. Prevalence of headache and migraine in schoolchildren. BMJ. 1994;309:765–9.
Abu-Arafeh I, Howells R. Primary headaches in children under the age of 7 years. Curr Pain Headache Rep. 2014;18:401–8. This article is the first and only review describing preschoolar primary headaches.
Warner JF. Recurrent headaches in children and associated pathological conditions. BMJ. 1879;2:889–90.
Lahat E, Barr J, Barzilai A, Cohen H, Berkovitch M. Visual evoked potentials in the diagnosis of headache before 5 years of age. Eur J Pediatr. 1999;158:892–5.
Balottin U, Nicoli F, Pitillo G, Ferrari Ginevra O, Borgatti R, Lanzi G. Migraine and tension headache in children under 6 years of age. Eur J Pain. 2004;8:307–14.
Raieli V, Eliseo M, Pandolfi E, La Vecchia M, La Franca G, Puma D, et al. Recurrent and chronic headaches in children below 6 years of age. J Headache Pain. 2005;6:135–42.
Balottin U, Termine C, Vicoli F. Idiopathic headache in children under six years of age: a follow-up study. Headache. 2005;45:705–15.
Battistella PA, Fiumana E, Binelli M, Bertossi E, Battista P, Perakis E, et al. Primary headaches in preschool age children: clinical study and follow-up in 163 patients. Cephalalgia. 2006;26:162–71.
Virtanen R, Aromaa M, Rautava P, Metsähonkala L, Anttila P, Helenius H, et al. Changing headache from preschool age to puberty. A controlled study. Cephalalgia. 2007;27:294–303. This original prospective study compares migraine and tension-type headache in an unselected population of children assessed at 6 and 13 years of age. Moreover, it describes the changing clinical features and trigger factors during the 7 years follow-up.
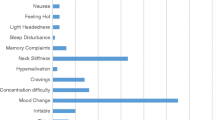
Eidlitz-Markus T, Gorali O, Haimi-Cohen Y, Zeharia A. Symptoms of migraine in the paediatric population by age group. Cephalalgia. 2008;28:1259–63.
Eidlitz-Markus T, Haimi-Cohen Y, Steier D, Zeharia A. Effectiveness of nonpharmacologic treatment for migraine in young children. Headache. 2010;50:219–23.
Ramdas S, Prasad M, Abu-Arefeh I. Primary headache disorders in children under 7 years of age. Scott Med J. 2013;58:26–9.
Raieli V, Pitino R, Giordano G, Spitalieri C, Consolo F, Puma D, et al. Migraine in a pediatric population: a clinical study in children younger than 7 years of age. Dev Med Child Neurol. 2015;57:585–8.
Torriero R, Capuano A, Mariani R, Frusciante R, Tarantino S, Papetti L, et al. Diagnosis of primary headache in children younger than 6 years: a clinical challenge. Cephalalgia. 2017;37:947–54.
Kang BS, Lee J, Choi JH, Kwon HH, Kang JW. Clinical manifestations of headache in children younger than 7 years. Korean J Pediatr. 2018;61:355–61.
Correnti E, Drago F, Messina LM, Rocchitelli L, D’Aiuto F, Vanadia F, et al. Headaches in preschoolers: are red flags predictive of positive neuroimaging in emergency department? SF J Headache Pain. 2018;1:1–5.
Straube A, Andreou A. Primary headaches during lifespan. J Headache Pain. 2019;20:35. https://doi.org/10.1186/s10194-019-0985-0.
GBD 2016 Headache Collaborators, Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954–76.
Headache Classification Subcommittee of the International Headache Society. The International Classification of headache disorders. 3nd edition. Cephalalgia. 2018;38:1–211.
Jernigan TL, Baaré WF, Stiles J, Madsen KS. Postnatal brain development: structural imaging of dynamic neurodevelopmental processes. Prog Brain Res. 2011;189:77–92.
Stiles J, Jernigan TL. The basics of brain development. Neuropsychol Rev. 2010;20:327–48.
Raieli V, Compagno A, Pandolfi E, La Vecchia M, Puma D, La Franca G, et al. Headache: what do children and mothers expect from pediatricians? Headache. 2010;50:290–300.
Sillanpaa M. The classification of migraine of headache. In: Guidetti V, Russell G, Sillanpaa M, Winner P, editors. Headache and migraine in childhood and adolescence. London: Martin Dunitz; 2002. p. 275–85.
Sillanpaa M. Prevalence of migraine and other headache in Finnish children starting school. Headache. 1976;15:288–90.
Sillanpaa M, Piekkala P, Kero P. Prevalence of headache at preschool age in an unselected child population. Cephalalgia. 1991;11:239–42.
Do TP, Remmers A, Schytz HW, Schankin C, Nelson SE, Obermann M, et al. Red and orange flags for secondary headaches in clinical practice SNNOOP10 list. Neurology. 2019;92:134–44.
Mortimer MJ, Kay J, Jaron A. Childhood migraine in general practice: clinical features and characteristics. Cephalalgia. 1992;12:238–43.
OstKirken G, Andler F, Hammer F, Pöhler KD, Snyder-Schendel E, Werner NK, et al. Prevalences of primary headaches symptoms at school-entry: a population-based epidemiological survey of preschool children in Germany. J Headache Pain. 2006;7:331–40.
Chu ML, Shinnar S. Headaches in children younger than 7 years of age. Arch Neurol. 1992;49:79–82.
Barlow CF. Migraine in the infant and toddler. J Child Neurol. 1994;9:92–4.
Cavestro C, Montrucchio F, Benci P, Pompilio D, Mandrino S, Cencio PG, et al. Headache prevalence and related symptoms, family history, and treatment habits in a representative population of children in Alba, Italy. Pediatr Neurol. 2014;51:348–53.
Vetri L, Messina LM, Drago F, D’Aiuto F, Vanadia F, Brighina F, et al. Are pediatric headaches in the emergency department increasing? An Italian experience. Funct Neurol. 2019;34:188-195.
Glover V, Fisk NM. Fetal pain: implications for research and practice. Br J Obstet Gynaecol. 1999;106:881–6.
Ken WS, Ashwell, Jürgen KMF, et al. Development of the central nervous system. In: The Human Nervous System (Third Edition); 2012. p. 31–79.
Derbyshire SW. Fetal pain: do we know enough to do the right thing? Reprod Health Matters. 2008;16:117–26.
American Academy of Pediatrics, Canadian Paediatric Society. Prevention and management of pain and stress in the neonate. Paediatrics. 2000;105:454–61.
Parida SK, Schneider DB, Stoss TD, Pauly TH, McGillis JP. Elevated circulating calcitonin gene-related peptide in umbilical cord and infant blood associated with maternal and neonatal sepsis and shock. Pediatr Res. 1998;43:276–82.
Bright FM, Vink R, Byard RW, Duncan JR, Krous HF, Paterson DS. Abnormalities in substance P neurokinin-1 receptor binding in key brainstem nuclei in sudden infant death syndrome related to prematurity and sex. PLoS One. 2017;20:e0184958. https://doi.org/10.1371/journal.pone.0184958.
Slater S, Crawford MJ, Kabbouche MA, LeCates SL, Cherney S, Vaughan P, et al. Effects of gender and age on paediatric headache. Cephalalgia. 2009;29:969–73.
Lidow MS. Long-term effects of neonatal pain on nociceptive systems. Pain. 2002;99:377–83.
Walker SM. Biological and neurodevelopmental implications of neonatal pain. Clin Perinatol. 2013;40:471–91.
Herlenius E, Lagercrantz H. Development of neurotransmitter systems during critical periods. Exp Neurol. 2004;190:S8–21.
Coq JO, Delcour M, Ogawa Y, Peyronnet J, Castets F, Turle-Lorenzo N, et al. Mild intrauterine hypoperfusion leads to lumbar and cortical hyperexcitability, spasticity, and muscle dysfunctions in rats: implications for prematurity. Front Neurol. 2018;15(9):423. https://doi.org/10.3389/fneur.2018.00423.
De Rogalski Landrot I, Roche F, Pichot V, Teyssier G, Gaspoz JM, Barthelemy JC, et al. Autonomic nervous system activity in premature and full-term infants from theoretical term to 7 years. Auton Neurosci. 2007;136:105–9.
Ploner M, Lee MC, Wiech K, Bingel U, Tracey I. Prestimulus functional connectivity determines pain perception in humans. PNAS. 2010;107:355–60.
Goksan S, Hartley C, Emery F, Cockrill N, Poorun R, Moultrie F, et al. fMRI reveals neural activity overlap between adult and infant pain. eLife. 2015;4:e06356. https://doi.org/10.7554/eLife.08663.
Goksan S, Baxter L, Moultrie F, Duff E, Hathway G, Hartley C, et al. The influence of the descending pain modulatory system on infant pain-related brain activity. Elife. 2018;11:7. https://doi.org/10.7554/eLife.37125.
Maneyapanda SB, Venkatasubramanian A. Relationship between significant perinatal events and migraine severity. Pediatrics. 2005;116:555–8.
Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10:895–926.
Kozlowska K, Palmer DM, Brown KJ, McLean L, Scher S, Gevirtz R, et al. Reduction of autonomic regulation in children and adolescents with conversion disorders. Psychosom Med. 2015;77:356–70.
Patel R, Qu C, Jennifer Y, Xie JY, Porreca F, Dickenson AH. Selective deficiencies in descending inhibitory modulation in neuropathic rats: implications for enhancing noradrenergic tone. Pain. 2018;159:1887–99.
Gotoh F, Komatsumoto S, Araki N, Gomi S. Noradrenergic nervous activity in migraine. Arch Neurol. 1984;41:951–5.
Benjelloun H, Birouk N, Slaoui I, Coghlan L. Autonomic profile of patients with migraine. Neurophysiol Clin. 2005;35:127–34.
Havanka-Kanniainen H, Tolonen U, Myllyla VV. Autonomic dysfunction in adult migraineurs. Headache. 1986;26:425–30.
Avnon Y, Nitzan M, Sprecher E, Rogowski Z, Yarnitsky D. Autonomic asymmetry in migraine augmented parasympathetic activation in left unilateral migraineurs. Brain. 2004;127:2099–108.
Hernandez-Latorre MA, Roig M. Natural history of migraine in childhood. Cephalalgia. 2000;20:573–9.
Marchese F, Rocchitelli L., Messina LM, Mangano GD, Nardello R, Vanadia F, Mangano S, Brighina F, Raieli V. Migraine in children under 6 years of age: a long-term follow-up study. Eur J. Paed Neurol. 2020; 27:67–71. This article is the first long term follow study in migrainous children under 7 years of age. Main findings are that early onset of migraine, familiarity of migraine and cranial autonomic symptoms are probable risk factors for persistence of migraine in adulthood.
Eidlitz-Markus T, Zeharia A. Symptoms and clinical parameters of pediatric and adolescent migraine, by gender -a retrospective cohort study. J Headache Pain. 2017;80. https://doi.org/10.1186/s10194-017-0789-z.
Eidlitz-Markus T, Haimi-Cohen Y, Zeharia A. Vomiting and migraine-related clinical parameters in pediatric migraine. Headache. 2017;57:899–907.
Raieli V, Compagno A, Brighina F, La Franca G, Puma D, Ragusa D, et al. Prevalence of red ear syndrome in the juvenile primary headaches. Cephalalgia. 2011;4:597–602.
Eidlitz-Markus T, Haimi-Cohen Y, Zeharia A. Association of age at onset of migraine with family history of migraine in children attending a pediatric headache clinic: a retrospective cohort study. Cephalalgia. 2015;35:722–7.
Eidlitz-Markus T, Zeharia A. Younger age of migraine onset in children than their parents: a retrospective cohort study. J Child Neurol. 2018;33:92–7.
Huang P, Kuo PH, Lee MT, Chiou LC, Fan PC. Age-dependent anti-migraine effects of valproic acid and topiramate in rats. Front Pharmacol. 2018;25(9):1095. https://doi.org/10.3389/fphar.2018.01095.
Powers SW, Coffey CS, Chamberlin LA, Ecklund DJ, Klingner EA, Yankey JW, et al. Trial of amitriptyline, topiramate, and placebo for pediatric migraine. N Engl J Med. 2017;12(376):115–24.
Hershey AD, Powers SW, Le Cates S, Bentti AL. Effectiveness of nasal sumatriptan in 5- to 12-year-old children. Headache. 2001;41:693–7.
Asuni C, Manchia M, Deidda A, Stochino ME, Cherchi A, del Zompo M. Mixture analysis of age at onset in migraine without aura: evidence for three subgroups. Headache. 2010;50:1313–9.
Guidetti V, Ottaviano S, Pagliarini M. Childhood headache risk: warning signs and symptoms present during the first six months of life. Cephalalgia. 1984;4:236–42.
Guidetti V, Cerutti R, Faedda N, Natalucci G. Migraine in childhood: an organic, biobehavioral, or psychosomatic disorder. Neurol Sci. 2019;40:93–8.
Author information
Authors and Affiliations
Contributions
Vincenzo Raieli conceived the review, Ettore Piro performed especially the section “Neuroanatomical and functional development of nervous system pathways and neurotransmitters involved in migraine,” Vincenzo Raieli and Antonina D’Amico performed the literature search and data analysis, and Vincenzo Raieli and Ettore Piro wrote the first draft of the manuscript and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Consent Form
Not applicable
Ethics Approval
Not applicable.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Childhood and Adolescent Headache
Rights and permissions
About this article
Cite this article
Raieli, V., D’Amico, A. & Piro, E. Migraine in Children Under 7 Years of Age: a Review. Curr Pain Headache Rep 24, 79 (2020). https://doi.org/10.1007/s11916-020-00912-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s11916-020-00912-5