Abstract
Background
Cryptococcal meningitis remains a common cause of mortality in low- and middle-income countries, where amphotericin B deoxycholate (amphotericin) plus fluconazole is the most common treatment. Flucytosine is almost uniformly absent as is outcome data on flucytosine use in routine care. The main goal of this study was identified the cumulative mortality at 2, 4, and 10 weeks after hospital admission.
Methods
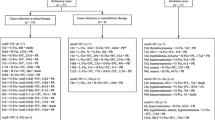
We conducted a retrospective, observational cohort study among HIV-infected adults with cryptococcal meningitis receiving amphotericin plus flucytosine as induction therapy in Brazil. We assessed cumulative mortality at 2, 4, and 10 weeks and the cumulative proportion discontinuating amphotericin or flucytosine due to toxicity at 2 weeks. We performed multiple logistic regression to identify variables associated with in-hospital mortality.
Results
In total, 77 individuals (n = 66 men) were included with median baseline CD4 of 29 (IQR, 9–68) cells/mcL. Twenty (26%) had at least one concurrent neurological disease diagnosed. Sixty (78%) patients received at least 14 days of amphotericin plus flucytosine. Cumulative mortality was 5% (4/77) at 2 weeks, 8% (6/77) at 4 weeks, and 19% (15/77) at 10 weeks. Cumulative proportion of patients that discontinuated amphotericin or flucytosine due to toxicity was 20% (16/77) at 2 weeks. In addition, in-hospital mortality was associated with receiving ≤ 10 days of induction therapy (odds ratio = 4.5, 95% CI 1.2–17.1, P = 0.028) or positive cerebrospinal fluid fungal culture after 2 weeks (odds ratio = 3.8, 95% CI 1.1–13.5, P = 0.035).
Conclusion
In this “real-world” study, amphotericin plus flucytosine shows low early mortality of patients with HIV-associated cryptococcal meningitis. Early discontinuation due to adverse events was moderate. More effective and safe antifungals are needed in order to improve the outcome of cryptococcal meningitis.
Similar content being viewed by others
Availability of Data and Material
All original data used in this study are available.
References
Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17:873.
Saag MS, Powderly WG, Cloud GA, et al. Comparison of amphotericin B with fluconazole in the treatment of acute AIDS-associated cryptococcal meningitis. The NIAID Mycoses Study Group and the AIDS Clinical Trials Group. N Engl J Med. 1992;326:83–9.
van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337:15–21.
Hamill RJ, Sobel JD, El-Sadr W, et al. Comparison of 2 doses of liposomal amphotericin B and conventional amphotericin B deoxycholate for treatment of AIDS associated acute cryptococcal meningitis: a randomized, double-blind clinical trial of efficacy and safety. Clin Infect Dis. 2010;51:225–32.
Brizendine KD, Baddley JW, Pappas PG. Predictors of mortality and differences in clinical features among patients with cryptococcosis according to immune status. PLoS ONE. 2013;8:e60431.
Spec A, Raval K, Powderly WG. End-Stage liver disease is strong predictor of early mortality in cryptococcosis. Open Forum Infect Dis. 2016;3:197.
Boulware DR, Meya DB, Muzoora C, COAT Trial Team, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med. 2014;370:2487–98.
Jarvis JN, Bicanic T, Loyse A, Namarika D, Jackson A, Nussbaum JC, et al. Determinants of mortality in a combined cohort of 501 patients with HIV-associated cryptococcal meningitis: implications for improving outcomes. Clin Infect Dis. 2014;58:736–45.
Beardsley J, Wolbers M, Kibengo FM, et al. CryptoDex investigators. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374:542–54.
Pyrgos V, Seitz AE, Steiner CA, Prevots DR, Williamson PR. Epidemiology of cryptococcal meningitis in the US: 1997–2009. PLoS ONE. 2013;8:e56269.
Vidal JE, de Oliveira ACP, Dauar RF, Boulware DR. Strategies to reduce mortality and morbidity due to AIDS-related cryptococcal meningitis in Latin America. Braz J Infect Dis. 2013;17:535–62.
Crabtree Ramírez B, Caro Vega Y, Shepherd BE, Le C, Turner M, Frola C, et al. Int J Infect Dis. 2017;63:57–63.
Firacative C, Lizarazo J, Illnait-Zaragozí MT, Castañeda E, Latin American Cryptococcal Study Group. The status of cryptococcosis in Latin America. Mem Inst Oswaldo Cruz. 2018;113:e170554.
Graybill JR, Sobel J, Saag M, van de Hoorst C, Powderly W, Cloud G, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. Clin Infect Dis. 2000;30:47–54.
Bahr NC, Rolfes MA, Musubire A, et al. Standardized electrolyte supplementation and fluid management improves survival during amphotericin therapy for cryptococcal meningitis in resource-limited settings. Open Forum Infect Dis. 2014;1:070.
Rolfes MA, Hullsiek KH, Rhein J, et al. The effect of therapeutic lumbar punctures on acute mortality from cryptococcal meningitis. Clin Infect Dis. 2014;59:1607–14.
Portegies P, Solod L, Cinque P, Chaudhuri A, Begovac J, Everall I, et al. Guidelines for the diagnosis and management of neurological complications of HIV infection. Eur J Neurol. 2004;11:297–304.
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Disease Society of America. Clin Infect Dis. 2010;50:291–322.
World Health Organization. Rapid advice: diagnosis, prevention, and management of cryptococcal disease in HIV-infected adults, adolescents and children. WHO Document Production Services, Geneva, Switzerland. 2011. pp 1–37. Available at: www.who.int/hiv/pub/cryptococcal_disease2011 Accessed 10 October 2012.
World Health Organization. WHO Guidelines for the diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children. 2018. vol. 2018, pp. 1–51.
Tenforde MW, Shapiro AE, Rouse B, Jarvis JN, Li T, Eshun-Wilson I, et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018;7:CD005647.
Department of Health and Human Services. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers of Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed in 10/12/2019.
Bennett JE, Dismukes WE, Duma RJ, Medoff G, Sande MA, Gallis H, et al. A comparison of amphotericin B alone and combined with flucytosine in the treatment of cryptococcal meningitis. N Engl J Med. 1979;301:126–31.
Brouwer AE, Rajanuwong A, Chierakul W, Griffin GE, Larsen RA, White NJ, et al. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomised trial. Lancet. 2004;363:1764–7.
Bicanic T, Wood R, Meintjes G, Rebe K, Brouwer A, Loyse A, et al. High-dose amphotericin B with flucytosine for the treatment of cryptococcal meningitis in HIV-infected patients: a randomized trial. Clin Infect Dis. 2008;47:123–30.
Day JN, Chau TT, Wolbers M, Mai PP, Dung NT, Mai NH, et al. Combination antifungal therapy reduces mortality in severe cryptococcal meningitis. N Engl J Med. 2013;368:1291–302.
Molloy SF, Kanyama C, Heyderman RS, Loyse A, Kouanfack C, Chanda D, et al. ACTA Trial Study Team antifungal combinations for treatment of cryptococcal meningitis in Africa. N Engl J Med. 2018;378:1004–17.
Dromer F, Mathoulin-Pélissier S, Launay O, Lortholary O, French Cryptococcosis Study Group. Determinants of disease presentation and outcome during cryptococcosis: the CryptoA/D study. PLoS Med. 2007;4(2):e21.
Luz PM, Girouard MP, Grinsztejn B, Freedberg KA, Veloso VG, Losina E, et al. Survival benefits of antiretroviral therapy in Brazil: a model based analysis. J Int AIDS Soc. 2016;19:20623.
Brasil. Ministério da Saúde. Departamento de Vigilância, Prevenção e Controle das IST, do HIV/Aids e das Hepatites Virais. Relatório de Monitoramento Clínico do HIV. Brasília: Ministério da Saúde; 2018. http://www.aids.gov.br/pt-br/pub/2018/relatorio-de-monitoramento-clinico-do-hiv-2018. Accessed 27 July 2020.
Coelho L, Cardoso SW, Amancio RT, Moreira RI, Campos DP, Veloso VG, et al. Trends in AIDS-defining opportunistic illnesses incidence over 25 years in Rio de Janeiro, Brazil. PLoS ONE. 2014;9:e98666.
Ford N, Shubber Z, Meintjes G, Grinsztejn B, Eholie S, Mills EJ, et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. Lancet HIV. 2015;2:e438–44.
Coelho LE, Cardoso SW, Amancio RT, Moreira RI, Ribeiro SR, Coelho AB, et al. Predictors of opportunistic illnesses incidence in post combination antiretroviral therapy era in an urban cohort from Rio de Janeiro, Brazil. BMC Infect Dis. 2016;16:134.
Manzardo C, Del Mar Ortega M, Sued O, Garcia F, Moreno A, Miro JM. Central nervous system opportunistic infections in developed countries in the highly active antiretroviral therapy era. J Neurovirol. 2005;11(suppl 3):72–82.
Oliveira JF, Greco DB, Oliveira GC, Christo PP, Guimarães MD, Oliveira RC. Neurological disease in HIV-infected patients in the era of highly active antiretroviral treatment: a Brazilian experience. Rev Soc Bras Med Trop. 2006;39:146–51.
Lizarazo J, Castro F, de Arco M, Chaves O, Peña Y. Infecciones oportunistas del sistema nervioso central en pacientes con VIH atendidos en el Hospital Universitario Erasmo Meoz de Cúcuta (1995–2005). Infectio. 2006;10:226–31.
Ávila G, González G. Algunas manifestaciones neurológicas del síndrome de inmunodeficiencia adquirida (SIDA) en pacientes del Hospital Universitario Hernando Moncaleano Perdomo de Neiva 2001–2004. Acta Neurol Colomb. 2007;23:90–4.
Vidal JE, de Oliveira ACP, Fink MC, Pannuti CS, Trujillo JR. AIDS related progressive multifocal leukoencephalopathy: a retrospective study in a referral center in São Paulo, Brazil. Rev Inst Med Trop Sao Paulo. 2008;50:209–12.
Mantilla JC, Cárdenas N. Colomb Med. 4. Vol. 40. Cali: 2009. Hallazgos neuropatológicos de la infección por VIH-SIDA: estudio de autopsias en el Hospital Universitario de Santander, Bucaramanga, Colombia; pp 422–431.
Lamotte JA. Caracterización de los pacientes en fase sida con infecciones del sistema nervioso central. Medisan. 2014;18:469–75.
Arechavala A, Negroni R, Messina F, Romero M, Marín E, Depardo R, et al. Cryptococcosis in an infectious diseases Hospital of Buenos Aires, Argentina. Revision of 2041 cases: diagnosis, clinical features and therapeutics. Rev Iberoam Micol. 2018;35:1–10.
Azambuja AZ, Wissmann Neto G, Watte G, Antoniolli L, Goldani LZ. Cryptococcal meningitis: a retrospective cohort of a brazilian reference hospital in the post-HAART era of universal access. Can J Infect Dis Med Microbiol. 2018;2018:6512468.
Falci DR, Lunardi LW, Ramos CG, Bay MB, Aquino VR, Goldani LZ. Continuous infusion of amphotericin B deoxycholate in the treatment of cryptococcal meningoencephalitis: analysis of safety and fungicidal activity. Clin Infect Dis. 2010;50:e26–9.
Pappalardo MC, Paschoal RC, Melhem MS. AIDS-associated central nervous system cryptococcosis: a Brazilian case study. AIDS. 2007;21:1971–2.
Vidal JE, Gerhardt J, de Miranda EJP, Dauar RF, Oliveira Filho GS, de Oliveira ACP, et al. Role of quantitative CSF microscopy to predict culture status and outcome in HIV-associated cryptococcal meningitis in a Brazilian cohort. Diagn Microbiol Infect Dis. 2012;73:68–73.
de Oliveira RB, Atobe JH, Souza SA, de Castro Lima Santos DW. Epidemiology of invasive fungal infections in patients with acquired immunodeficiency syndrome at a reference hospital for infectious diseases in Brazil. Mycopathologia. 2014;178:71–8.
Chagas OJ, Buccheri R, Melhem MSC, Szeszs W, Martins MA, de Oliveira L, Marcusso R, Santos DW. Useful of yeast cell counting and lack of clinical correlation of the antifungal susceptibility testing results in management of AIDS-associated cryptococcal meningitis. Curr Fung Infect Rep. 2020;14:1–8.
Metta HA, Corti ME, Negroni R, Helou S, Arechavala A, Soto I, et al. Disseminated cryptococcosis in patients with AIDS. Clinical, microbiological, and immunological analysis of 51 patients. Rev Argent Microbiol. 2002;34:117–23.
Pasqualotto AC, Bittencourt Severo C, de Mattos Oliveira F, Severo LC. Cryptococcemia. An analysis of 28 cases with emphasis on the clinical outcome and its etiologic agent. Rev Iberoam Micol. 2004;21:143–6.
Moreira TA, Ferreira MS, Ribas RM, Borges AS. Cryptococcosis: clinical epidemiological laboratorial study and fungi varieties in 96 patients. Rev Soc Bras Med Trop. 2006;39:255–8.
Leimann BC, Koifman RJ. Cryptococcal meningitis in Rio de Janeiro State, Brazil, 1994–2004. Cad Saude Publica. 2008;24:2582–92.
Mónaco LS, Tamayo Antabak N. Cryptococcosis in AIDS patients: case study from 1996 to 2006 in Paroissien Hospital. Rev Argent Microbiol. 2008;40:218–21.
Lindenberg Ade S, Chang MR, Paniago AM, Lazéra Mdos S, Moncada PM, Bonfim GF, Nogueira SA, Wanke B. Clinical and epidemiological features of 123 cases of cryptococcosis in Mato Grosso do Sul, Brazil. Rev Inst Med Trop Sao Paulo. 2008;50:75–8.
Mora DJ, da Cunha Colombo ER, Ferreira-Paim K, Andrade-Silva LE, Nascentes GA, Silva-Vergara ML. Clinical, epidemiological and outcome features of patients with cryptococcosis in Uberaba, Minas Gerais, Brazil. Mycopathologia. 2012;173:321–7.
Meintjes G, Kerkhoff AD, Burton R, Schutz C, Boulle A, Van Wyk G, et al. HIV-related medical admissions to a South African District Hospital remain frequent despite effective antiretroviral therapy scale-up. Medicine (Baltimore). 2015;94:e2269.
Vidal JE, de Oliveira ACP, Pellegrino D, et al. Complicações neurológicas em pacientes infectados pelo HIV e fatores associados a óbito na era CART: estudo observacional prospectivo no Instituto de Infectologia Emílio Ribas. Braz J Infect Dis. 2011;15(1):23.
Telles JP, Fernandes R, Barros TD, et al. The continuous challenging of neuroepidemiology in people living with HIV/AIDS in the late antiretroviral therapy in Brazil. In: 29th European congress of clinical microbiology and infectious diseases, 2019. Amsterdam, The Netherlands. Poster P0724.
Musubire AK, Boulware DR, Meya DB, Rhein J. Diagnosis and management of cryptococcal relapse. J AIDS Clin Res 2013;3(Suppl 3):S3-003.
Robinson PA, Bauer M, Leal MA, et al. Early mycological treatment failure in AIDS-associated cryptococcal meningitis. Clin Infect Dis. 1999;28:82–92.
Pitisuttithum P, Tansuphasawadikul S, Simpson AJ, et al. A prospective study of AIDS-associated cryptococcal meningitis in Thailand treated with high-dose amphotericin B. J Infect. 2001;43:226–33.
Chang CC, Dorasay AA, Gosnell BI, et al. Clinical and mycological predictors of cryptococcosis-associated Immune reconstitution inflammatory syndrome (C-IRIS). AIDS. 2013;27:2089–99.
Rolfes MA, Rhein J, Schutz C, Taseera K, Nabeta HW, Huppler Hullsiek K, et al. Cerebrospinal fluid culture positivity and clinical outcomes after amphotericin-based induction therapy for cryptococcal meningitis. Open Forum Infect Dis. 2015;2:157.
Acknowledgements
DRB is supported by the Fogarty International Center and National Institute of Neurologic Disorders and Stroke (R01NS086312-07).
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
José E. Vidal and Camila de Albuquerque Moraes contributed to the study conception and design. Material preparation, data collection, and analysis were performed by José E. Vidal, Camila de Albuquerque Moraes, Renata Elisie Barbalho de Siqueira, Nathalya Fernanda Brito Miranda, David R Boulware, Augusto C. Penalva de Oliveira, and Rosa Marcusso. The first draft of the manuscript was written by José E. Vidal, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics Approval
Approval was obtained from the Ethics Committee of Instituto de Infectologia Emílio Ribas, São Paulo, Brazil.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Handling Editor: Rosely Maria Zancope-Oliveira.
Rights and permissions
About this article
Cite this article
Vidal, J.E., de Albuquerque Moraes, C., de Siqueira, R.E.B. et al. HIV-Associated Cryptococcal Meningitis Patients Treated with Amphotericin B Deoxycholate Plus Flucytosine under Routine Care Conditions in a Referral Center in São Paulo, Brazil. Mycopathologia 186, 93–102 (2021). https://doi.org/10.1007/s11046-020-00512-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-020-00512-2