Abstract
Antibiotic resistance surveillance through regional and up-to-date testing of clinical isolates is a foundation for implementing effective empirical treatment. Surveillance data also provides an overview of geographical and temporal changes that are invaluable for guiding interventions. Still, due to limited infrastructure and resources, clinical surveillance data is lacking in many parts of the world. Given that sewage is largely made up of human fecal bacteria from many people, sewage epidemiology could provide a cost-efficient strategy to partly fill the current gap in clinical surveillance of antibiotic resistance. Here we explored the potential of sewage metagenomic data to assess clinical antibiotic resistance prevalence using environmental and clinical surveillance data from across the world. The sewage resistome correlated to clinical surveillance data of invasive Escherichia coli isolates, but none of several tested approaches provided a sufficient resolution for clear discrimination between resistance towards different classes of antibiotics. However, in combination with socioeconomic data, the overall clinical resistance situation could be predicted with good precision. We conclude that analyses of bacterial genes in sewage could contribute to informing management of antibiotic resistance.
Similar content being viewed by others
Introduction
Antibiotics are critical for the prevention and treatment of bacterial infections. The global rise in antibiotic resistance is therefore threatening large parts of modern health care. Regional, up-to-date surveillance data on resistance levels to different antibiotics in different pathogens is critical for guiding optimal empirical antibiotic treatment1. Surveillance also serves the purpose of identifying temporal resistance trends that can be used to guide or evaluate interventions to reduce the development of multiresistant bacteria.
Traditional surveillance data are based on data from a large number of clinical isolates, each subjected to susceptibility testing with standardized methods. As this approach is labor intensive, expensive and needs specialized infrastructure2, surveillance data are lacking or very limited in many parts of the world, not least in low- and middle-income countries3. In addition, the collection of resistance data from clinical isolates is far from standardized across the world4, making comparisons between countries challenging and hampering global efforts to tackle the resistance crisis.
For decades, municipal sewage has been used to monitor poliovirus at a community level5. More recently, a similar approach has been taken to capture regional development of SARS-CoV-2 prevalence6,7. Sewage epidemiology has also been proposed as an alternative or complementary method to overcome some of the challenges in antibiotic resistance surveillance, particularly the need for extensive patient sampling and the limited resources and infrastructure in low- and middle-income countries. In addition, sewage epidemiology can be used to sample entire populations without linking data to individuals, avoiding ethical challenges related to traditional surveillance1,2,4 and even serve as an early warning system for new or rare forms of antibiotic resistance8,9. Clinical resistance surveillance is often biased to more severe cases as only a minority of non-hospitalized patients are being sampled and samples taken after initial treatment failure are overrepresented2. In contrast, sewage-based surveillance covers the whole population served by the sewage network and therefore presents a less-biased picture of regional resistance levels8,9,10,11. The differences in resistance prevalence in hospital and community waste waters also demonstrate the bias in clinical settings2,8,9.
There are at least two main approaches for sewage-based antibiotic resistance monitoring; isolate-based approaches or gene-based analyses of complex microbial communities. Some of the advantages and disadvantages of both approaches have recently been reviewed12. In short, the isolate-based approach uses susceptibility testing of many individual bacterial isolates and thus offers direct information about the resistance phenotype, including multi-resistance patterns in clinically relevant species. However, although a large number of isolates can be efficiently collected and managed as recently indicated by a global monitoring of cefotaxime-resistant coliforms from sewage13, this approach can be as labor intensive as clinical surveillance with regard to the susceptibility testing part. The gene-based approach, on the other hand, uses the metagenomic DNA of the sewage community and can either target the whole resistome (shotgun sequencing) or focus on a specific set of resistance genes (PCR). Therefore, the gene-based approach reflects the genetic basis for resistance in all species present in the sewage, but cannot offer direct information on resistance phenotype. The infrastructure for sequencing and bioinformatic analyses could easily be centralized and only sampling would need to be done locally, further reducing the costs and infrastructure needed and making the method easier to standardize4. There are, however, several conceptual limitations with a metagenomic approach. These include (1) prediction from genotype to phenotype (2) challenge to identify point mutations leading to antibiotic resistance, (3) shotgun sequencing makes it hard to assign resistance genes and thus predicted resistances to specific species, and (4) the challenge to identify multi-resistance patterns without data on isolates.
Depending on the intended purpose of surveillance and thus the need for precision, metagenomic analyses may still prove to be valuable, but until now, an evaluation of how well such data correlates to regional clinical surveillance data has been lacking4. Some data do suggest that it could be possible to predict clinical resistance levels from sewage data. In a trans-European high-throughput PCR-array based surveillance study, the abundance of sewage antibiotic resistance genes (ARGs) was shown to mirror the north-to-south clinical resistance gradient in Europe14. Furthermore, resistance levels of Escherichia coli isolated from sewage have recently been shown to correlate with the resistance levels in clinical isolates1,2.
Recently, a global monitoring of ARGs in sewage was conducted, including over 60 countries15. There were systematic differences in ARG prevalence between continents; Asia, Africa, and South America having a higher incidence of ARGs in sewage compared with Europe, North-America, and Oceania. Antibiotic usage is often considered to be the most important factor driving resistance, but in this study the differences in sewage resistance could be best explained with socioeconomic factors15. Another study came to similar conclusions when analyzing global clinical resistance data; antibiotic use was not the best predictor, but rather socioeconomic factors16. Both Collignon et al.16 and Hendriksen et al.15 observed that factors related to sanitation/hygiene are significantly associated with antibiotic resistance, both when expressed in terms of ARG abundances in sewage and when expressed in terms of the proportion of resistant E. coli in clinical isolates. Thus, both studies hypothesized that contagion, the spread of resistant bacteria, could be one of the most important drivers of the prevalence of clinical resistance globally. Poor hygiene, poor sanitation, and poor infrastructure enhance contagion, resulting in more individuals being infected with/carriers of resistant strains17. This could, in turn, lead to increased shedding of resistant bacteria on a community level, which could be reflected in sewage. Resistance in sewage bacteria is, conceptually, a more direct measure of resistance in a population than both antibiotic use or social factors, mirroring insufficient transmission control. Data from sewage therefore has the potential to reflect clinical resistance levels regardless of drivers, and possibly better than previous models based on social factors.
As metagenome-based surveillance data quantify the whole-community resistome, it is not obvious which genetic markers correlate best with clinical resistance to the different classes of antibiotics in infections caused by a given pathogen. An optimal marker should be both specific and sensitive to be able to accurately reveal the local clinical resistance levels in a given species to a given antibiotic. One apparent approach would be to quantify ARGs for each class of antibiotic in sewage metagenomes separately, but given that ARGs are unequally distributed across species, this might be misleading when correlating the sum of ARGs to the resistance in clinical isolates of a given species. A way to at least partly circumvent this could be to use only ARGs commonly found in a given species, e.g., ARGs in the E. coli accessory genome. Still, a large portion of the ARGs known to occur in E. coli may actually be present in other species in the sewage community, thus likely reducing the correlation. As a broad indication of resistance, the prevalence of class 1 integrons, more specifically the intI1 integrase gene, has previously been linked to phenotypic resistance in E. coli18,19, hence the correlation to this gene could be worthwhile investigating.
Here, we aimed to explore whether sewage metagenomic data reflect clinical antibiotic resistance on a global scale and if so, how accurately it is possible to predict clinical resistance using models based on sewage metagenomic data. To achieve this, we investigated the correlation between reported clinical resistance prevalence in bloodstream infections of E. coli or an aggregated resistance index from16 and either (1) total ARGs, (2) total ARGs for each antibiotic class separately, (3) the 10 most abundant ARGs that are known to be present in the E. coli pangenome, (4) the 10 most abundant E. coli ARGs separated by antibiotic class, (5) IntI1 integron gene abundances in sewage. Furthermore, we (6) compared whether sewage data correlated better to the prevalence of clinical resistance compared with socioeconomic factors. Last, we (7) explored if models based on both sewage data and socioeconomic factors would give the best model for clinical resistance prevalence in terms of model fit. After a leave-one-out cross-validation of the models, we (8) used sewage data together with socioeconomic factors to predict clinical antibiotic resistance in countries where surveillance data are lacking.
Results and discussion
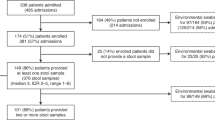
In this study, we explored the possibility to use country level relative abundance of ARGs in sewage metagenomic data to predict country level proportion of antibiotic-resistant clinical isolates. We annotated the total acquired resistance gene abundance and the class 1 integron (intI1) integrase gene abundance from recently published global sewage metagenomic data set from ref. 15. Publicly available country level data on the proportion of resistant invasive E. coli clinical isolates was collected based on availability for four different antibiotic classes; aminopenicillins, fluoroquinolones, third-generation cephalosporins and aminoglycosides. In addition, we used the “aggregate resistance” index as generated by Collignon et al.16, representing the combined average prevalence of E. coli and Klebsiella spp resistant to third-generation cephalosporins, fluoroquinolones, and carbapenems, and meticillin-resistant Staphylococcus aureus.
First, the annotated acquired ARGs in the sewage metagenomic data were correlated with the proportion of resistant clinical E. coli using a beta regression model. The relative abundance of all ARGs could, however, not to a large extent, explain the variability in the clinical resistance patterns (p value < 0.05, R2 0.12–0.24, Table 1). A similar result was obtained when separating the ARGs into individual resistance classes (i.e., beta-lactam, fluoroquinolone, third-generation cephalosporin, and aminoglycoside resistance genes). Here, only the models where beta-lactam ARGs were correlated with clinical aminopenicillin resistance had a noticeable higher model fit than when using all combined ARGs (p value < 0.05, R2 0.31, Supplementary Fig. 2 and Table 1). Next, in an effort to further reduce the noise in the data, only the ten most common acquired ARGs found in all sequenced E. coli genomes were used. These models showed higher model fits for all resistance classes compared with the models using all ARGs found in the metagenomic data (R2 0.41, 0.49, 0.39, and 0.20 for the clinical aminopenicillin, fluoroquinolone, third-generation cephalosporin and aminoglycoside resistance, respectively, Fig. 1, Table 1).
Proportion of resistant invasive E. coli clinical isolates to aminopenicillins a, fluoroquinolones b, third generation cephalosporins c, and aminoglycosides d against the relative abundance of the 10 most common ARGs in E. coli. The blue line shows the fitted clinical resistance from the beta regression model with resistance gene abundance as explanatory variable. Note that for some countries, data on clinical resistance was not available for all classes.
We observed that one country, Malta, created an outlier that strongly affected the models with the ten most common E. coli ARGs. When Malta was excluded from the analysis, the model fit increased substantially for all clinical resistance classes (R2 values of 0.72, 0.67, 0.72, and 0.44 for the aforementioned clinical resistance profiles, Supplementary Fig. 3). However, as we had no prior reason to believe that the data obtained for Malta is erroneous, we chose to keep it in the model. When using the ten most abundant ARGs in E. coli separated by the antibiotic class they confer resistance to, a better model fit was achieved for the beta-lactam and third generation cephalosporin ARGs predicting aminopenicillin and third generation cephalosporin resistance (R2 values of 0.48 and 0.53, respectively). It should be noted that cross-correlations (using ARGs for one antibiotic class to correlate with clinical resistance to another class) was approximately as good, or even better (e.g., beta-lactam ARG model for clinical fluoroquinolone resistance) than within-class correlations (Table 1). Although this may appear counterintuitive, this could have multiple explanations. Even with the attempt to use only ARGs found in E. coli, a large portion of the ARGs could very well be present in other species in the sewage. The relative abundance of the genus E. coli in the sewage metagenomes varied from 0.1 to 10%, with a mean of 1%15. Our inability to capture mutation-based resistance, the dominant factor behind, e.g., fluoroquinolone resistance, is another possible reason. It should be noted that clinical resistance prevalence to the investigated antibiotic classes were strongly correlated to each other (Supplementary Fig. 1). With such close correlation, it becomes more difficult to find models that can explain resistance to individual classes of antibiotics with high specificity.
Given that the class-related information on ARGs had a limited contribution to the correlations, the correlation between intI1 integrase gene abundance and prevalence of resistance to different classes of antibiotics in clinical E. coli isolates was investigated. Here, the level of correlation varied substantially between antibiotic classes (p value < 0.01, R2 0.31–0.66, Fig. 2, Table 1). The best model was found for fluoroquinolone (R2 0.66) and third-generation cephalosporin (R2 0.62) resistance in clinical isolates. The model for aminoglycoside resistance had the lowest model fit (R2 0.31). Although total acquired ARG and intI1 gene counts were correlated in the sewage data (p < 0.01, R2 0.42, Suppl. Material), intI1 overall performed better. The association of intI1 to phenotypic resistance in E. coli18,19 might have less noise compared with the resistance gene approach, which is hampered by the broad distribution of ARGs in bacteria, explaining the overall better performance. This, in turn, would mean that this approach might not be optimal for other clinically relevant pathogens.
Proportion of resistant invasive E. coli clinical isolates to aminopenicillins a, fluoroquinolones b, third-generation cephalosporins c, and aminoglycosides d against intI1 integrase gene abundance. The blue line shows the fitted clinical resistance from the beta regression model with intI1 abundance as explanatory variable. Note that for some countries, data on clinical resistance was not available for all classes.
When modeling the aggregated resistance index, neither the intI1 abundance nor the acquired E. coli ARGs had as good model fit as for E. coli clinical resistance patterns. However, they were still significantly associated (p value < 0.01, R2 0.24 and 0.30, respectively, Table 1, Fig. 3a and Supplementary Fig. 4). In the intI1 model, two outlier data points (Nigeria and Peru) had very high intI1 abundance, whereas the aggregated resistance index was moderate. Removing these two data points enhanced the model considerably (p value < 0.01, R2 0.43, Fig. 3b). There was no clinical resistance surveillance data for E. coli available from these two countries. The outliers could, potentially, be caused by an error in the aggregated resistance index data since higher values, at least for Peru, were already reported in 2008–200920. There is only sparse data on clinical resistance prevalence for Nigeria, but very high resistance levels for E. coli and Klebsiella against third-generation cephalosporins (80–90%) have been reported21.
Aggregated resistance index as described in Collignon et al.16 correlated with normalized intI1 gene abundance in sewage. All data in a and two outliers (Nigeria and Peru) removed in b. The blue line shows the fitted clinical resistance from the beta regression model with intI1 abundance in sewage as an explanatory variable.
Taken together, the total abundance of all acquired ARGs, the top ten most common E. coli associated acquired ARGs and intI1 gene counts could be used to predict clinical resistance prevalence with varying precision. Sewage metagenomic data also appears to provide more accurate predictions of clinical resistance levels to some antibiotic classes than others. As intI1 integrase gene counts overall performed the best in our analysis, and is a considerably simpler measure than a large set of ARGs, it was used in further analyses. These results should therefore be interpreted as indications of the overall resistance prevalence. Therefore, resistance patterns to any antibiotic classes that do not follow the overall resistance pattern would be predicted less accurately.
Although sewage metagenome data alone correlated with clinical resistance with reasonably high precision in most cases, there was still a lot of variability in the data that could not be explained with the sewage data alone. Socioeconomic factors have been shown to be good predictors of clinical resistance16,17. Previous results suggest that contagion may be one of the most important factors contributing to the prevalence of clinical resistance17. Countries with better sanitation and better health care infrastructure, and therefore less contagion in, e.g., hospitals, could have lower clinical resistant prevalence despite the higher resistance levels in the overall population. Since socioeconomic factors, most likely, have an indirect influence on the clinical resistance levels, the sewage data could be a more direct measure reflecting the prevalence of resistance in local populations.
To compare correlations between sewage data and prevalence of clinical resistance to correlations between socioeconomical factors and clinical resistance prevalence, we collected selected socioeconomic factors for all included countries from the World Bank database. Gross domestic product (GDP) and the proportion of the population living in urban areas correlated with each other and the factors related to basic living conditions; access to electricity, basic sanitation index and availability of clean drinking water were strongly correlated with each other (Suppl. Fig. 5). Owing to the correlations between the collected socioeconomical factors, only basic sanitation, GDP and proportion of urban population were used in modeling clinical resistance rates. Models based on these three socioeconomical factors performed better than models based on sewage data only (R2 0.68–0.84, Suppl. Table 1). This showed that although being indirect measures of clinical resistance, socioeconomical factors correlated with clinical antibiotic resistance prevalence on country level, thus confirming the results by16,17.
To explore if we could refine our models further, we proceeded by combining socioeconomic factors with our sewage-based models. The simplistic intI1 model performed better or equally well as the different ARG models and was therefore used in the combined models. Relative intI1 abundance in the sewage metagenomes, the logarithm of GDP, basic sanitation index and the proportion of urban population were included in all models of clinical resistance. The socioeconomical factors were negatively correlated with clinical resistance; more urban population, better sanitation and bigger GDP predicted lower clinical resistance rates, whereas higher sewage resistance predicted higher clinical resistance (Figs. 4 and 5). In all models, except for aminoglycoside resistance, a combined model with sewage data and socioeconomical factors gave a better model fit than using either alone (Table 1, Supplementary Table 1). Already in the sewage data alone model, the aminoglycoside resistance model had the lowest model fit and the combination with socioeconomic factors did not give a better model fit than using socioeconomic factors alone (Table 1 and Fig. 4d).
Proportion of clinical resistant invasive E. coli isolates to aminopenicillins a, fluoroquinolones b, third-generation cephalosporins c, and aminoglycosides d against relative intI1 integrase gene abundance in sewage. Proportion of urban population is shown with different shades of blue and size of point corresponds to basic sanitation index. The blue lines show the fitted clinical resistance from the beta regression model with socioeconomical factors and relative intI1 abundance (see text for details). Three different socioeconomical scenarios (blue lines) have been fitted to the model to shown how sewage data correlates with clinical resistance. Dark blue line: lower quartile (25%), blue: mean quantile (50%) and light blue: upper quantile (75%) of socioeconomical factors fitted to the model. Note that GDP is not shown in the plots, but is included in all models and fitted lines.
Aggregated resistance index as described in Collignon et al.16 against relative intI1 integrase gene abundance in sewage. Proportion of urban population is shown with different shades of blue and size of point corresponds to basic sanitation index. The blue lines show the fitted clinical resistance from the beta regression model with socioeconomical factors and relative intI1 abundance (see text for details). Three different socioeconomical scenarios (blue lines) have been fitted to the model to shown how sewage data correlates with clinical resistance. Dark blue line: lower quartile (25%), blue: mean quantile (50%) and light blue: upper quantile (75%) of socioeconomical factors fitted to the model. Note that GDP is not shown in the plots, but is included in all models and fitted lines. Data from Nigeria and Peru are not included.
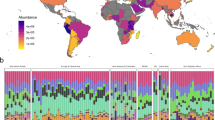
Based on the best combined models, we assessed how well clinical resistance could be predicted in countries where we did not have clinical surveillance data. To estimate how good the models are at predicting clinical resistance, a leave-one-out cross-validation was performed. From the cross-validation, the mean absolute error (MAE) was calculated for each resistance profile (aminopenicillin, fluoroquinolone, third-generation cephalosporins, aminoglycoside and aggregated resistance index). In general, all models performed well in predicting clinical resistance with the MAE ([%]) ranging from 5.99 (aminopenicillin) to 8.27 (fluoroquinolone) (Methods, Supplementary Table 2, Supplementary Fig. 6). Next, using the combined models with socioeconomic factors and sewage data for each resistance class, we predicted the proportions of resistant clinical isolates for all countries where clinical resistance data were lacking from any of the classes included in this study. Not surprisingly, the models predict the highest resistance rates for countries in Africa, South Africa being an exception (Fig. 6). For Georgia and Macedonia, the clinical resistance data was based on very few isolates (<100), so these countries were not included in the original models. However, our models predict lower clinical resistance levels in these two countries than the surveillance data, suggesting that the data based on only a few isolates was potentially biased towards more severe clinical cases and does not reflect the real prevalence of clinical resistance in these countries (Fig. 6). As stated earlier, Nigeria and Peru seemed to be outliers with high intI1 abundance in sewage, but only moderate aggregated resistance index. Our combined models predict very high clinical resistance levels in Nigeria and Peru (Fig. 6). There is also support in the literature for the higher clinical resistance levels for these two countries20,21. Clinical resistance data obtained from ResistanceMap22 for Nigeria shows a high level resistance in E. coli against third-generation cephalosporins and fluoroquinolones (>75% in 2017), in line with the predictions made by our model. Resistance data for Peru is lacking from ResistanceMap.
Predictions for countries where we did not have clinical resistance data from at least one of the resistance classes, including the aggregated resistance index, based on the final beta regression models including both relative abundance of relative intI1 integrase gene abundance in sewage and socioeconomic data. In cases where there was clinical surveillance data for some antibiotic classes available, only the surveillance data are shown as proportion. The numbers shown for Georgia and Macedonia are based on very few (<100) isolates, so they were not included in the models, but were included in the predictions. The values from surveillance are displayed in top of the predicted ones. Pred AP predicted aminopenicillin, Pred FQ predicted fluoroquinolone, Pred 3rd GC predicted third-generation cephalosporin, Pred AG predicted aminoglycoside, Pred Agg predicted aggregated resistance index.
To get an overview of the global clinical resistance we used the model for the aggregated resistance index (from ref. 16) for all countries where sewage resistance and socioeconomical data were available (Fig. 7, for other classes see Supplementary Fig. 7). Our global predictions were in line with previous literature and showed that the clinical resistance levels are highest in South America, Africa, and Asia16,23. Of course, these are predictions rather than direct observations. Although the leave-one-out cross-validation added confidence to the predictive power of the model, and could reflect accurately the overall clinical resistance situation in these countries, values should be interpreted with caution.
Sewage metagenomic data certainly have limitations and cannot directly replace clinical surveillance. For example, current methods are unable to link resistance genes found in sewage metagenomes to their bacterial hosts. As resistance patterns in different pathogens are correlated (Supplementary Figs. 9–12) it is plausible that the resistance of additional species also could be predicted by sewage metagenomics data, but such models would need further optimization and validation. With our models, some resistance patterns are better predicted than others and the results most likely will provide more information about the overall prevalence of antibiotic resistance than giving a high resolution of specific resistance profiles for a given species. As mentioned, many resistance phenotypes are a result of point mutations, and detecting these with a metagenomics approach is challenging. From a conceptual point of view, isolate-based approaches are therefore likely needed for sufficient precision for all classes of antibiotics. A metagenomic approach could still provide important and cost-efficient information on geographical and temporal trends, thereby indicating where stewardship actions are effective, ineffective or particularly needed.
In conclusion, sewage data alone correlated to the overall clinical resistance levels. However, despite efforts to use the information from the abundances of separate ARG classes, the correlations to clinical resistance did not improve. A model based only on relative abundance of intI1 performed better or on par with all tested approaches based on ARGs. Models based on sewage metagenomic data had, furthermore, a lower model fit than models based on socioeconomic factors. One important reason for this is likely the differences in bacterial populations between those causing disease and those contributing to gene counts in the sewage metagenomes, e.g., not all E. coli strains cause disease in humans. Another reason is the difficulties to translate abundances of disconnected single resistance genes into bacterial phenotypes, including the inability to detect mutation-based resistance. There are also differences in the human populations covered, as sewage is usually from one or a few cities covering all inhabitants including carriers without disease, whereas clinical resistance data are usually generated on a country-wide basis but with a bias towards hospitalized, sick patients. In here, the sewage data were from one to few sewage treatment plants and then extrapolated to represent the whole country, as the clinical data were on country level. Optimal data would include time-matched, clinical resistance data representing the same population served by the sewage treatment plant. The best models were achieved by combining sewage metagenomic data with socioeconomic data. Such a model could, as demonstrated here, be used for clinical resistance prevalence predictions to get a view of global clinical resistance prevalence including countries where surveillance data on clinical resistance is lacking.
Methods
Data extraction
All data used in this study were retrieved from public databases or published articles (Table 2).
Metagenome sequence analysis
Raw sequencing data were downloaded from ENA under the project accession ERP015409. Remaining adapter sequences were removed with cutadapt v. 2.724. The trimmed reads were searched for ARGs against the ResFinder database v.3.1.025 using DIAMOND v. 0.9.l1426 with parameters “–id 90 –min-orf 20 –seq no” and the ARG counts in each sample were normalized with the total sequencing effort (M bases). Sum of normalized gene counts was used as a proxy for sewage resistance load. The intI1 integrase gene abundance was determined in similar fashion (except “—id 95”) using the MobileGeneticElementDatabase from ref. 27 and adding up the intI1 integrase gene counts. For countries with more than one metagenome, the mean of counts was used.
To determine which ARGs that were connected to E. coli, all genomes annotated as E. coli were downloaded from NCBI genbank in December 2019. The genomes were then searched for ARGs against the Resfinder database using DIAMOND v. 0.9.14 with parameters “blastx –max-target-seq 0 –subject-cover 70”. The best scoring hits with a sequence identity higher than 98% at a given position in the genome were then extracted and used in the subsequent analysis. The most common ARGs in the available E. coli genomes were determined through counting the occurrence of each extracted hit.
Statistics and reproducibility
The prevalence of clinical resistance was modeled using beta regression with log-log link function using function betareg from betareg v. 3.1–2. We used the pseudo R2 values calculated by betareg function and referred to them as R2 values for clarity throughout the manuscript. The difference in model fit between nested beta regression models were assessed using likelihood ratio test with function lrtest from package lmtest (v.0.9.37). The PCA ordinations were calculated using function rda from vegan v. 2.5–6. The correlation plots were drawn using function ggpairs from GGally v.1.4.0. The heatmap was produced with package pheatmap v. 1.0.12. All other figures were produced with ggplot2 v. 3.2.1.
The leave-one-out cross-validation was performed as follows. For each type of clinical resistance, the sewage data together with the socioeconomic data were modeled as above but with one country excluded. The level of clinical resistance was then predicted for the excluded country using the obtained model. This was repeated for each country in the data set. For each country the absolute error, consisting of the absolute value of the difference of the real value and the predicted value, was calculated. The mean absolute error (MAE) was then calculated based on the average over the absolute error for all countries.
All data analysis steps were done in R v. 3.6.2. For more-detailed data analysis see the project analysis repository at: www.github.com/karkman/GlobalSewage. The project repository also contains all needed numerical data to reproduce the analyses in this project.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data sets analyzed during the current study are publicly available and listed under Data extraction in Methods.
Code availability
Detailed data analysis for this study can be found from: www.github.com/karkman/GlobalSewage.
References
Huijbers, P. M. C., Larsson, D. G. J. & Flach, C.-F. Surveillance of antibiotic resistant Escherichia coli in human populations through urban wastewater in ten European countries. Environ. Pollut. 261, 114200 (2020).
Hutinel, M. et al. Population-level surveillance of antibiotic resistance in Escherichia coli through sewage analysis. Euro Surveill. 24, 1800497 (2019).
World Health Organization. Global antimicrobial resistance and use surveillance system (GLASS) report (2020).
Aarestrup, F. M. & Woolhouse, M. E. J. Using sewage for surveillance of antimicrobial resistance. Science 367, 630–632 (2020).
Hovi, T. et al. Role of environmental poliovirus surveillance in global polio eradication and beyond. Epidemiol. Infect. 140, 1–13 (2012).
Kitajima, M. et al. SARS-CoV-2 in wastewater: state of the knowledge and research needs. Sci. Total Environ. 739, 139076 (2020).
Medema, G., Heijnen, L., Elsinga, G., Italiaander, R., & Brouwer, A. Presence of SARS-coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ. Sci. Technol. Lett. acs.estlett.0c00357 (2020).
Kwak, Y.-K. et al. Surveillance of antimicrobial resistance among Escherichia coli in wastewater in Stockholm during 1 year: does it reflect the resistance trends in the society? Int. J. Antimicrobial Agents 45, 25–32 (2015).
Paulshus, E. et al. Diversity and antibiotic resistance among Escherichia coli populations in hospital and community wastewater compared to wastewater at the receiving urban treatment plant. Water Res. 161, 232–241 (2019).
Kühn, I. Comparison of enterococcal populations in animals, humans, and the environment - a European study. Int. J. Food Microbiol. 88, 133–145 (2003).
Reinthaler, F. F. et al. Resistance patterns of Escherichia coli isolated from sewage sludge in comparison with those isolated from human patients in 2000 and 2009. J. Water Health 11, 13–20 (2013).
Huijbers, P. M. C., Flach, C.-F. & Larsson, D. G. J. A conceptual framework for the environmental surveillance of antibiotics and antibiotic resistance. Environ. Int. 130, 104880 (2019).
Marano, R. B. M. et al. A global multinational survey of cefotaxime-resistant coliforms in urban wastewater treatment plants. Environ. Int. 144, 106035 (2020).
Pärnänen, K. M. M. et al. Antibiotic resistance in European wastewater treatment plants mirrors the pattern of clinical antibiotic resistance prevalence. Sci. Adv. 5, eaau9124 (2019).
Hendriksen, R. S. et al. Global monitoring of antimicrobial resistance based on metagenomics analyses of urban sewage. Nat. Commun. 10, 1124 (2019).
Collignon, P., Beggs, J. J., Walsh, T. R., Gandra, S. & Laxminarayan, R. Anthropological and socioeconomic factors contributing to global antimicrobial resistance: a univariate and multivariable analysis. Lancet Planet. Health 2, e398–e405 (2018).
Collignon, P. & Beggs, J. J. Socioeconomic enablers for contagion: factors impelling the antimicrobial resistance epidemic. Antibiotics 8, 86 (2019).
Skurnik, D. et al. Integron-associated antibiotic resistance and phylogenetic grouping of escherichia coli isolates from healthy subjects free of recent antibiotic exposure. AAC 49, 3062–3065 (2005).
Skurnik, D. et al. Characteristics of human intestinal Escherichia coli with changing environments. Environ. Microbiol. 10, 2132–2137 (2008).
García, C. et al. Antimicrobial drug resistance in Peru. Emerg. Infect. Dis. 18, 520–521 (2012).
Bernabé, K. J., Langendorf, C., Ford, N., Ronat, J.-B. & Murphy, R. A. Antimicrobial resistance in West Africa: a systematic review and meta-analysis. Int. J. Antimicrob. Agents 50, 629–639 (2017).
CDDEP, T.C. for D., Dynamics Economics & Policy. ResistanceMap: Antibiotic resistance (2020).
Laxminarayan, R. et al. Antibiotic resistance—the need for global solutions. Lancet Infect. Dis. 13, 1057–1098 (2013).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet. J. 17, 10 (2011).
Zankari, E. et al. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 67, 2640–2644 (2012).
Buchfink, B., Xie, C. & Huson, D. H. Fast and sensitive protein alignment using DIAMOND. Nat. Methods 12, 59–60 (2015).
Pärnänen, K. et al. Maternal gut and breast milk microbiota affect infant gut antibiotic resistome and mobile genetic elements. Nat. Commun. 9, 3891 (2018).
Acknowledgements
The authors thank Dr Patricia M. Huijbers for valuable discussions during the initiation of this study. The authors also wish to acknowledge CSC – IT Center for Science, Finland, for generous computational resources. This work was funded by the Swedish Research Council (VR) (2018-02835 and 2018-05771 to D.G.J.L.) and the Region Västra Götaland under the ALF agreement (grant number ALFGBG-717901). A.K. was supported by Academy of Finland, grant number 315678.
Funding
Open Access funding provided by Gothenburg University Library.
Author information
Authors and Affiliations
Contributions
Design of the study: A.K., F.B., E.K., C.F.F., D.G.J.L. Data collection and analyses: A.K., F.B. Interpreting results: A.K., F.B., E.K., C.F.F., D.G.J.L. A.K. drafted the manuscript, with contributions from all of the authors. All of the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karkman, A., Berglund, F., Flach, CF. et al. Predicting clinical resistance prevalence using sewage metagenomic data. Commun Biol 3, 711 (2020). https://doi.org/10.1038/s42003-020-01439-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-020-01439-6
This article is cited by
-
Global within-species phylogenetics of sewage microbes suggest that local adaptation shapes geographical bacterial clustering
Communications Biology (2023)
-
Social demographics determinants for resistome and microbiome variation of a multiethnic community in Southern Malaysia
npj Biofilms and Microbiomes (2023)
-
Antibiotic resistance in the environment
Nature Reviews Microbiology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.