Abstract
Repeated bolus injections are associated with higher costs and poor compliance and can hinder the implementation of global immunization campaigns. Here, we report the development and preclinical testing of patches of transdermal core–shell microneedles—which were fabricated by the micromoulding and alignment of vaccine cores and shells made from poly(lactic-co-glycolic acid) with varying degradability kinetics—for the preprogrammed burst release of vaccine payloads over a period of a few days to more than a month from a single administration. In rats, microneedles loaded with a clinically available vaccine (Prevnar-13) against the bacterium Streptococcus pneumoniae induced immune responses that were similar to immune responses observed after multiple subcutaneous bolus injections, and led to immune protection against a lethal bacterial dose. Microneedle patches delivering preprogrammed doses may offer an alternative strategy to prophylactic and therapeutic protocols that require multiple injections.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The main data supporting the results in this study are available within the paper and its Supplementary Information. All data generated in this study, including source data and the data used to generate the figures, are available at Figshare under the identifier https://doi.org/10.6084/m9.figshare.12951794.
References
Ochoa, T. J. et al. Vaccine schedule compliance among very low birth weight infants in Lima, Peru. Vaccine 33, 354–358 (2015).
Majumder, M. S., Cohn, E. L., Mekaru, S. R., Huston, J. E. & Brownstein, J. S. Substandard vaccination compliance and the 2015 measles outbreak. JAMA Pediatr. 169, 494–495 (2015).
Pierce, C. et al. The impact of the standards for pediatric immunization practices on vaccination coverage levels. JAMA 276, 626–630 (1996).
Simonsen, L., Kane, A., Lloyd, J., Zaffran, M. & Kane, M. In focus—unsafe injections in the developing world and transmission of bloodborne pathogens: a review. Bull. World Health Organ. 77, 789–800 (1999).
Dicko, M. et al. Safety of immunization injections in Africa: not simply a problem of logistics. Bull. World Health Organ. 78, 163–169 (2000).
Bloom, B. R. Vaccines for the third world. Nature 342, 115–120 (1989).
McHugh, K. J., Guarecuco, R., Langer, R. & Jaklenec, A. Single-injection vaccines: progress, challenges, and opportunities. J. Control. Release 219, 596–609 (2015).
Hutin, Y. & Chen, R. T. Injection safety: a global challenge. Bull. World Health Organ. 77, 787–788 (1999).
Kermode, M. Unsafe injections in low-income country health settings: need for injection safety promotion to prevent the spread of blood-borne viruses. Health Promot. Int. 19, 95–103 (2004).
Tzeng, S. Y. et al. Stabilized single-injection inactivated polio vaccine elicits a strong neutralizing immune response. Proc. Natl Acad. Sci. USA 115, E5269–E5278 (2018).
Li, W. et al. Rapidly separable microneedle patch for the sustained release of a contraceptive. Nat. Biomed. Eng. 3, 220–229 (2019).
Joyce, J. C. et al. A microneedle patch for measles and rubella vaccination is immunogenic and protective in infant rhesus macaques. J. Infect. Dis. 218, 124–132 (2018).
Wang, C., Ye, Y., Hochu, G. M., Sadeghifar, H. & Gu, Z. Enhanced cancer immunotherapy by microneedle patch-assisted delivery of anti-PD1 antibody. Nano Lett. 16, 2334–2340 (2016).
Yu, J. et al. Microneedle-array patches loaded with hypoxia-sensitive vesicles provide fast glucose-responsive insulin delivery. Proc. Natl Acad. Sci. USA 112, 8260–8265 (2015).
van der Maaden, K., Jiskoot, W. & Bouwstra, J. Microneedle technologies for (trans) dermal drug and vaccine delivery. J. Control. Release 161, 645–655 (2012).
Moga, K. A. et al. Rapidly-dissolvable microneedle patches via a highly scalable and reproducible soft lithography approach. Adv. Mater. 25, 5060–5066 (2013).
Sullivan, S. P. et al. Dissolving polymer microneedle patches for influenza vaccination. Nat. Med. 16, 915–920 (2010).
Chen, M.-C., Huang, S.-F., Lai, K.-Y. & Ling, M.-H. Fully embeddable chitosan microneedles as a sustained release depot for intradermal vaccination. Biomaterials 34, 3077–3086 (2013).
DeMuth, P. C., Min, Y., Irvine, D. J. & Hammond, P. T. Implantable silk composite microneedles for programmable vaccine release kinetics and enhanced immunogenicity in transcutaneous immunization. Adv. Healthc. Mat. 3, 47–58 (2014).
Hong, X. et al. Dissolving and biodegradable microneedle technologies for transdermal sustained delivery of drug and vaccine. Drug Des. Devel. Ther. 7, 945–952 (2013).
Grayson, A. C. R. et al. Multi-pulse drug delivery from a resorbable polymeric microchip device. Nat. Mater. 2, 767–772 (2003).
Stevenson, C. L., Santini, J. T. Jr & Langer, R. Reservoir-based drug delivery systems utilizing microtechnology. Adv. Drug Deliv. Rev. 64, 1590–1602 (2012).
Goole, J. & Amighi, K. 3D printing in pharmaceutics: a new tool for designing customized drug delivery systems. Int. J. Pharm. 499, 376–394 (2016).
Zhang, J. et al. 3D-printed magnetic Fe3O4/MBG/PCL composite scaffolds with multifunctionality of bone regeneration, local anticancer drug delivery and hyperthermia. J. Mater. Chem. B 2, 7583–7595 (2014).
Curry, E. J., Henoun, A. D., Miller, A. N. & Nguyen, T. D. 3D nano- and micro-patterning of biomaterials for controlled drug delivery. Ther. Deliv. 8, 15–28 (2016).
Tran, K. T. & Nguyen, T. D. Lithography-based methods to manufacture biomaterials at small scales. J. Sci. Adv. Mater. Devices 2, 1–14 (2017).
McHugh, K. J. et al. Fabrication of fillable microparticles and other complex 3D microstructures. Science 357, 1138–1142 (2017).
Deegan, R. D. et al. Capillary flow as the cause of ring stains from dried liquid drops. Nature 389, 827–829 (1997).
Park, J.-H., Allen, M. G. & Prausnitz, M. R. Biodegradable polymer microneedles: fabrication, mechanics and transdermal drug delivery. J. Control. Release 104, 51–66 (2005).
Davis, S. P., Landis, B. J., Adams, Z. H., Allen, M. G. & Prausnitz, M. R. Insertion of microneedles into skin: measurement and prediction of insertion force and needle fracture force. J. Biomech. 37, 1155–1163 (2004).
Chen, M.-C., Chan, H.-A., Ling, M.-H. & Su, L.-C. Implantable polymeric microneedles with phototriggerable properties as a patient-controlled transdermal analgesia system. J. Mater. Chem. B 5, 496–503 (2017).
Bronaugh, R. L., Stewart, R. F. & Congdon, E. R. Differences in permeability of rat skin related to sex and body site. J. Soc. Cosmet. Chem. 34, 127–135 (1983).
O’hagan, D. et al. Biodegradable microparticles as controlled release antigen delivery systems. Immunology 73, 239–242 (1991).
Draize, J. H., Woodard, G. & Calvery, H. O. Methods for the study of irritation and toxicity of substances applied topically to the skin and mucous membranes. J. Pharmacol. Exp. Ther. 82, 377–390 (1944).
ACIP Preventing Pneumococcal Disease Among Infants and Young Children. Recommendations of the Advisory Committee on Immunization Practices (ACIP). Recommendations and Reports: Morbidity and Mortality Weekly Report 49, 1–38 (MMWR, 2000).
Darkes, M. J. & Plosker, G. L. Pneumococcal conjugate vaccine (Prevnar™1; PNCRM7). Pediatr. Drugs 4, 609–630 (2002).
Elert, G. Temperature of a Healthy Human (Skin Temperature) (The Physics Factbook, 2007); http://hypertextbook.com/facts/2001/AbantyFarzana.shtml
Ripolin, A. et al. Successful application of large microneedle patches by human volunteers. Int. J. Pharm. 521, 92–101 (2017).
Li, W. et al. Long-acting reversible contraception by effervescent microneedle patch. Sci. Adv. 5, eaaw8145 (2019).
Levine, M. M. Can needle-free administration of vaccines become the norm in global immunization? Nat. Med. 9, 99–103 (2003).
Nossal, G. J. The Global Alliance for Vaccines and Immunization—a millennial challenge. Nat. Immunol. 1, 5–8 (2000).
Boopathy, A. V. et al. Enhancing humoral immunity via sustained-release implantable microneedle patch vaccination. Proc. Natl Acad. Sci. USA 116, 16473–16478 (2019).
ThIel, M. & Hermatschweiler, M. Three-dimensional laser lithography: a new degree of freedom for science and industry. Opt. Photon. 6, 36–39 (2011).
Rolland, J. P. et al. Direct fabrication and harvesting of monodisperse, shape-specific nanobiomaterials. J. Am. Chem. Soc. 127, 10096–10100 (2005).
Romero-Steiner, S. et al. Standardization of an opsonophagocytic assay for the measurement of functional antibody activity against Streptococcus pneumoniae using differentiated HL-60 cells. Clin. Diagn. Lab. Immunol. 4, 415–422 (1997).
Acknowledgements
We thank staff at the UConn Clean room and IVIS SpectrumCT facilities for equipment support on the microfabrication and in vivo imaging, respectively; C. Schondelmeyer and staff at the University of Connecticut Animal Facility for training and support for our animal research; staff at the UConn/Thermo Fisher Scientific Center for Advanced Microscopy and Materials Analysis for SEM imaging; staff at the UConn Machine shop, K. S. Wrobel, N. Romano and A. N. Miller for making the custom-built alignment device; F. Almonte for his assistance with mechanical testing; the undergraduate students A. Johnson, K. Berkery, E. Grandell, N. Pasnoori and H. Patel for help with the fabrication process, biological experiments and measuring release time points. The initial funding of this project was provided by Bio pipeline CT and Start-up funding from University of Connecticut (USA). This work was performed in part at the Advanced Science Research Center NanoFabrication Facility of the Graduate Center at the City University of New York, USA.
Author information
Authors and Affiliations
Contributions
K.T.M.T. and T.D.N. designed the concepts and research studies. K.T.M.T., S.M.S. and T.D.N. conceived the experiments. K.T.M.T., T.D.G., N.J.F., E.J.C., A.B.M., A.P., L.B., S.K., N.M. and R.P. performed the research and experiments. T.D.G., S.M.S. and T.D.N. provided reagents, advice and materials. K.T.M.T., T.D.G., S.M.S. and T.D.N. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–19, Tables 1–3 and references.
Supplementary Video 1
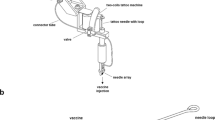
Fabrication process for the core–shell microneedles.
Supplementary Video 2
Administration of the microneedles into rat skin using a commercial applicator.
Rights and permissions
About this article
Cite this article
Tran, K.T.M., Gavitt, T.D., Farrell, N.J. et al. Transdermal microneedles for the programmable burst release of multiple vaccine payloads. Nat Biomed Eng 5, 998–1007 (2021). https://doi.org/10.1038/s41551-020-00650-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41551-020-00650-4
This article is cited by
-
Microneedle-mediated nanomedicine to enhance therapeutic and diagnostic efficacy
Nano Convergence (2024)
-
Digital automation of transdermal drug delivery with high spatiotemporal resolution
Nature Communications (2024)
-
Non-invasive transdermal delivery of biomacromolecules with fluorocarbon-modified chitosan for melanoma immunotherapy and viral vaccines
Nature Communications (2024)
-
Smart and versatile biomaterials for cutaneous wound healing
Biomaterials Research (2023)
-
Microneedle biomedical devices
Nature Reviews Bioengineering (2023)