Abstract
One of the most common bath solutions used in musculoskeletal mechanical testing is phosphate buffered saline (PBS). In tendon, swelling induced by physiological PBS results in decreased tendon modulus and induces microstructural changes. It is critical to evaluate the multiscale mechanical behavior of tendon under swelling to interpret prior work and provide information to design future studies. We compared the effects of physiological PBS and 8% polyethylene glycol and saline bathing solutions on tendon multiscale tendon mechanics and damage as well as microstructure with TEM in order to understand the effect of swelling on tendon. At the tissue level, tendons in PBS had a lower modulus than SPEG samples. PBS samples also showed an increased amount of non-recoverable sliding, which is an analog for microscale damage. SPEG had a higher microscale to tissue-scale strain ratio, showing the fibrils experienced less strain attenuation. From the TEM data, we showed the fibril spacing of SPEG samples was more similar to fresh control than PBS. We concluded that swelling alters multiscale mechanics and damage in addition to tendon microstructure. Future mechanical testing should consider using SPEG as a bath solution with an osmotic pressure which preserves fresh tissue water content.
Similar content being viewed by others
Introduction
Bath solutions are frequently necessary during tissue mechanical testing in order to maintain tissue hydration, mechanics, and microstructure. One of the most common bath solutions used for tendon and other musculoskeletal samples is phosphate buffered saline (PBS). However, even at physiological concentrations (15 mM), PBS causes tissue swelling. In tendon, this swelling results in decreased tendon modulus and induces microstructural changes.6,22 SEM images of tendon equilibrated in PBS show that collagen fibril diameter is increased and fibril packing density is decreased in rat tail tendon.22 The swelling effect of PBS has been observed in other collagenous tissues as well, including ligament, annulus fibrosus, and meniscus.1,3,6 Along with inducing swelling, solutes present in buffer may diffuse into tissue and alter structure and mechanics.2,4,7,8,29
With evidence of PBS solution altering tissue-level mechanics and microscale structure, it is critical to evaluate the multiscale mechanical behavior of tendon under these conditions. We have previously investigated multiscale mechanics and damage in tendon by comparing sequential loading curves and microscale recovery.11,13,27 In these experiments, microscale damage was related to changes in tissue-level mechanical parameters after loading. By using a similar multiscale approach, it is possible to link the observed PBS related changes in structure to changes in mechanical behavior.
For many tests, using a bath solution is not optional, either as a result of sample cross section or test duration. The duration of our multiscale experiments is long enough that a buffer solution is necessary to avoid tissue drying (> 55 min), thus no buffer-free “fresh” control can exist. Our group previously investigated possible bath alternatives to PBS. We showed that a combination of 8% weight polyethylene glycol (PEG) by volume of Tris-buffered saline maintained physiological levels of tissue hydration.20 PEG was selected because the available large particle size (~ 20 kDa) does not readily diffuse into the tissue.10,26 In addition to its large size restricting diffusion, PEG is a hydrophilic polymer, contributing to its ability to maintain tissue hydration.17,19,24,25 Using the PEG and saline solution (SPEG) as a bathing solution to prevent swelling facilitates investigation of the difference in mechanics between swollen and non-swollen tissue. Previous studies on multiscale mechanics and damage were completed with PBS,12,13,27 and understanding this effect of swelling offers a lens to interpret prior work as well as providing information to better design future studies.
The objective of this study was to compare the effects of PBS and 8% SPEG bathing solutions on multiscale tendon mechanics and damage as well as tendon microstructure to understand the effect of osmotic pressure on tendon. We hypothesized that increased tendon swelling due to the use of physiological PBS causes microstructural changes that alter microscale sliding and increase tendon damage during tensile loading compared with a bath that maintains fresh tendon hydration.
Materials and Methods
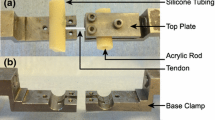
Sample Preparation
Rat tail tendon samples were harvested from fresh-frozen female Long-Evans rats, aged 4-7 months, which were obtained from another study not affecting musculoskeletal tissues. The samples were limited to a maximum of 2 freeze-thaw cycles, and a maximum storage time 4 months at − 20 °C, with all tendons coming from frozen, undissected animals.11 The entire tail was removed, with the 80 mm proximal section preserved with skin intact. Tendon fascicles were individually removed from the proximal tail portion using forceps. A centimeter from each end of the tendon was removed in order to eliminate any tissue possibly damaged during sample preparation. Each sample was stained with a 10 μg/ml solution of DTAF (5-(4,6-dichlorotriazinyl) Aminofluorescein) (5-DTAF, Life Technologies) for 30 min to prepare the sample for photobleaching.11,13
Samples were split into two groups, PBS or SPEG, where samples equilibrated in either 15 mM PBS solution (n = 8), or an 8% weight by volume solution of PEG and 15 mM Tris-buffered saline (n = 7).20 The Tris buffer, which is monovalent, was used with PEG instead of the phosphate buffer in PBS, which is divalent. This selection was made in order to compare to prior work.20 A fresh control, or one tested without the presence of a buffer, is not viable for the mechanical tests due to the duration of the mechanical tests. Two ink markers were made on the tendon surface at the midportion to allow for digital image correlation. All samples were kept at room temperature after thawing and throughout mechanical testing. Each sample was equilibrated in its bath solution for at least 90 min before testing, with some samples equilibrating for up to 6 hours, depending on testing order in a single day. As tendon equilibrates in PBS after 15 min, with no change seen at 8 hours, this variation is reasonable.20
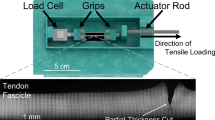
Mechanical Testing Protocol
The testing protocol was similar to that used in prior studies.11,28 There are known mechanical differences between testing at room temperature and at physiological temperature; however, we completed our experiments at room temperature as we were interested in comparing our results to similar prior studies.5,9,11,12,20,22,27 Each sample was tested using a custom uniaxial testing device mounted on an inverted confocal microscope (LSM 5 LIVE, objective Plan-Apochromat 10×/0.45), which allows for simultaneous imaging and mechanical loading. The sample was gripped and loaded to a reference length by applying a 5 mN (0.5 g) preload. Each sample was then preconditioned with 5 cycles between 0 and 2% strain. Following preconditioning, four parallel photobleached lines were made on the midportion of the tendon, between the ink markers, equally spaced 200 μm apart. Each sample was then ramped to 6% strain (Baseline), held for 15 min at constant 6% grip strain, and unloaded back to the reference length. The sample remained at the reference length for a 40-min recovery period before undergoing a second ramp (Diagnostic) until failure (Fig. 1). All loading and unloading rates were 0.1%/s. We chose 6% strain as our previous study indicated it was sufficient to induce damage.11,13,27 While the applied grip strain was 6%, post-test optical imaging indicated that tissue strain was 3.9 ± 0.4 and 3.6 ± 0.4% for the PBS and SPEG groups, respectively, with no difference between groups (t test, p > 0.1).
(a) Mechanical loading protocol used in experiment, showing the time points for confocal imaging with blue circles. The Baseline and Diagnostic ramps are indicated in green and red, respectively. PC = Preconditioning. (b) A representative stress-strain curve, showing the Baseline and Diagnostic curves. Transition point (blue circle), modulus (dashed line), and inflection point (purple square) are indicated, as well as the Δ value difference between them. (c) Confocal images of a sample tendon at the reference, end of ramp, end of stress-relaxation, and end of rest. Microscale strain (ε) and microscale sliding (γ) are also indicated.
Imaging and Data Acquisition
To measure the tissue strain, we imaged the tendon with a CCD camera to track displacement of the ink markers on the midportion surface using digital image correlation (Vic 2D, Correlated Solutions). For microscale analysis, confocal image stacks were taken after preconditioning, at the beginning and end of loading, immediately after unloading, and every 10 min during the recovery (blue dots in Fig. 1a). The cross-sectional area was calculated using confocal imaging of the major and minor axes of each sample at the reference length and an ellipse fitted to obtain area of the cross-section.
Tissue-Level Data Analysis
Tissue-level strain (\(\varepsilon\)) was measured from tracking displacement of surface ink markers, while tissue-level stress (\(\sigma\)) was calculated by dividing the tensile force by the initial cross-sectional area. Transition point, inflection point, and linear region modulus were all calculated from the \(\sigma - \varepsilon\) curve, with the transition point defined as the end of the toe region and inflection point as the change between strain-stiffening and strain-softening behavior (Fig. 1b). The inflection point was calculated by fitting a cubic smoothing spline with the csaps function in MATLAB and finding the first zero crossing point of the second derivative. The stress-strain curve between zero and the inflection point was fit to a nonlinear exponential constitutive model which was optimized to obtain the transition strain (p), transition stress (q), and linear region modulus (E):
The optimization was performed on three of the parameters (p, A, B) and was completed using the MATLAB function fmincon to minimize the mean square error. Optimization was performed for both the Baseline and Diagnostic ramps. The change in these measures between the Baseline and Diagnostic ramp was quantified as a delta value (∆), of the Baseline–Diagnostic, where a non-zero delta values indicates damage as a result of mechanical loading (Fig. 1b). Conversely, when ∆ = 0, or Baseline and Diagnostic measures are the same, no damage is observed.
Microscale Data Analysis
The microscale parameters were measured from the photobleached lines, where the deformation was tracked to calculate microscale strain and sliding. Microscale strain was calculated from the average displacement of the photobleached lines, while microscale sliding was calculated as the average tortuosity of the lines (Fig. 1c). Sliding recovery after unloading was decomposed into elastic recovery, viscous recovery, and non-recoverable, using the sliding measured at the end of loading (EL), start of rest (SR), and end of the rest (ER). Elastic recovery, the sliding that immediately recovered after unloading, was calculated as:
The viscoelastic recovery, or the sliding recovered during the rest period after subtracting the elastic recovery, was calculated as:
The non-recoverable sliding was the residual sliding remaining at the end of the rest period, calculated as the sliding value at EL minus the elastic and viscous recovery.
In order to evaluate the strain transfer between the tissue and microscale levels, the ratio of microscale strain to tissue strain was calculated at the end of the Baseline ramp (beginning of stress-relaxation period).
Transmission Electron Microscopy (TEM)
Samples were prepared for TEM without any mechanical testing. Samples were in 3 different groups: PBS, SPEG, and Fresh (n = 3/group). For the PBS and SPEG samples, a single fascicle was bisected, with one half going to each group. Samples in PBS and SPEG were equilibrated in the appropriate buffer for 90 min prior to processing, while the Fresh group was processed immediately following dissection. Each sample was fixed with 2% glutaraldehyde and 2% paraformaldehyde in 0.1 M sodium cacodylate buffer overnight at 4 °C. The next day, the sample was cut to 1 mm segments and fixed for an additional hour in the fixative solution. The sample spent 2 hours in a 1% osmium tetroxide in 0.1 M sodium cacodylate buffer before being washed with DI water three times for 15 min each. Next, dehydration was completed in an ascending acetone series, including a 95% acetone step lasting 48 hours. Dehydration was finished with two 30-min fixations in 100% anhydrous acetone. The sample was finally subjected to multiple ascending steps of first polypropylene oxide and the EMBed-812 Resin before polymerization in a vacuum. After processing, the sample was ultramicrotomed before TEM imaging (Libra 120 TEM, Zeiss). TEM images were segmented manually using GIMP software (GIMP 2.10.12), and the distributions of fibril diameter and area density calculated using FIJI.21 Images with artifacts or other features which might affect the density calculation, such as cells or large gaps, were excluded.
Statistical Analysis
The difference in mechanical parameters between the SPEG and PBS groups was determined using a two-tailed Student’s t test with significance set to 0.05. A Kolmogorov-Smirnov test was performed to evaluate the normality of all data. Of the forty-eight measured parameters, all were normally distributed except four. The non-normal measured data were PBS Diagnostic Transition Strain, and PBS microscale strain at three of the seven time points. For any comparisons involving these data, a nonparametric two-tailed Mann-Whitney test was used with significance set to 0.05. Additionally, the ∆ values comparing the differences between Baseline and Diagnostic between the two ramps in a single group were evaluated using a one-sample t test to determine if a statistically significant difference from zero existed (p < 0.05). All statistical tests were completed in GraphPad Prism.
Results
Tissue-Level Parameters
For the tissue-level parameters, we first compared the SPEG and PBS mechanical parameters from the Baseline ramps, which represented a pre-mechanically damaged state (Fig. 2). The SPEG samples had a higher linear region modulus, consistent with prior literature (p = 0.0003).20 SPEG also had a higher inflection point stress compared to the PBS samples (p = 0.009), while there were no differences between the groups for inflection point strain, transition strain, or transition stress.
The Baseline values for (a) transition strain, (b) transition stress, (c) inflection point strain, (d) inflection point stress, and (e) modulus were calculated for both for SPEG (n = 7) and PBS (n = 8) groups. There was no difference between groups for transition strain, transition stress, or inflection point strain. * (p < 0.05). Error bars represent 95% confidence interval.
In order to compare the effect of swelling on damage in the tissue, the change in mechanical parameters was calculated using a ∆ parameter (calculated as difference between Baseline and Diagnostic) (Fig. 3). A non-zero ∆ value indicates tissue-level damage, while a zero ∆ indicates no damage induced by mechanical loading. For transition strain, SPEG and PBS showed damage (p = 0.003, p = 0.053). Additionally, the ∆ transition strain was higher in SPEG samples than in PBS (p = 0.014). For transition stress, neither group showed damage and were not different from each other (p = 0.22, p = 0.64, p = 0.15). For inflection point strain, both SPEG and PBS showed damage (p = 0.007, p = 0.001), though were not different from each other (p = 0.42). For inflection point stress, SPEG did not show damage, though PBS did (p = 0.70, p = 0.008). Consequently, the ∆ inflection point stress was higher in PBS (p = 0.043). For modulus, both SPEG and PBS showed damage (p = 0.0002, p = 0.006). Additionally, SPEG showed greater damage than PBS (p = 0.0002). This modulus result is consistent with previous work using this loading regime.11,13
The Baseline and Diagnostic values for (a) transition strain, (b) transition stress, (c) inflection point strain, (d) inflection point stress, and (e) modulus were calculated for both SPEG and PBS. (f–j) The difference between Baseline and Diagnostic was calculated as a Δ value. * (p < 0.05), # significantly different from zero (p < 0.05). Error bars indicate the 95% confidence interval.
Microscale Parameters
In order to evaluate the microscale mechanics, we measured mechanical changes using photobleached lines on the midportion of the tendon. Microscale results were calculated for each time point of confocal imaging. Microscale strain was calculated as the average strain between the photobleached lines. SPEG samples experienced higher microscale strain during the end of the ramp (p < 0.05), at the end of stress relaxation (p < 0.05), and throughout the relaxation period, excepting the time point at 25 min (p = 0.39) (Fig. 4a). While neither group returned to zero strain, the SPEG group had a greater partial recovery with a final mean strain of -0.0031 and the PBS group with a final mean strain of -0.0094 (Fig. 4a). Microscale sliding was calculated as the average tortuosity of the photobleached lines, normalized to the reference measurements. Microscale sliding only partially recovered for both groups and sliding was not different between groups at any time point (Fig. 4b, p > 0.10).
Microscale mechanical behavior for SPEG and PBS. (a) Both groups experienced partial recovery of microscale strain after unloading, with significantly different magnitudes throughout recovery (p < 0.02). This suggests that collagen fibrils experienced more damage with PBS incubation. (b) Microscale sliding also showed only partial recovery for both groups. * (p < 0.05).
The microscale sliding recovery was decomposed into elastic recovery, viscous recovery, and non-recoverable sliding (Fig. 5). There was no difference between the groups for both elastic and viscous recovery (p > 0.20 and p > 0.80). The amount of non-recoverable sliding, a measure for microscale damage, was lower in SPEG samples compared to PBS samples (p < 0.05).
Decomposed recovery for microscale sliding for SPEG and PBS. (a) Elastic and (b) viscous recovery showed no significant differences between groups. (c) Non-recoverable sliding (residual sliding at the end of recovery) was higher in the PBS group. Error bars represent the 95% confidence interval. * (p < 0.05).
In order to evaluate the transfer of strain between the different hierarchical levels of tendon, we calculated the strain ratio from the microscale measurements to the tissue-level measurements. The time point for which we have simultaneous strain measurements was at the end of the Baseline ramp. The microscale to tissue strain ratio at this time point was higher in SPEG compared to PBS (Fig. 6, p < 0.001).
TEM
Representative images and segmented masks from each group show the effect of bath solution on image quality (Figs. 7a–7f). The distributions of fibril diameters for each group were all found. (Figs. 7g–7i). The medians of the distribution of fibril diameter and the % area density (Figs. 7j–7k) were measured for SPEG, PBS, and Fresh.
Representative TEM images from (a) Fresh (fixed immediately after dissection), (b) SPEG, and (c) PBS groups. (d–f) Masks of representative images. Fibril diameter distribution for (g) Fresh, (h) SPEG, and (i) PBS. The distributions were all significantly different from each other as determined by a one-way ANOVA (p = 0.0009). The solid line indicates the combined distribution mean, while the dashed line indicated the median. (j) The % area of fibrils was not different between Fresh and SPEG, though Fresh and SPEG both had % area densities larger than PBS. (k) The fibril diameter distribution medians were not different between any groups.
Discussion
In this study, we have shown that a PBS bathing solution alters tendon multiscale mechanics and increases microscale damage compared to an SPEG bathing solution. At the tissue level, tendons in the PBS group had a lower modulus than SPEG samples for their baseline curves. PBS samples also showed an increased amount of non-recoverable sliding, which was an analog for microscale damage. In relation to load transfer between hierarchical levels, SPEG had a higher microscale to tissue strain ratio, which was close to 1. Thus, fibrils in SPEG experienced less strain attenuation between hierarchical levels than those in PBS.
The tissue-level mechanical behavior for PBS was consistent with previous findings,10,11,–13,20 as was the baseline tissue-level behavior for the SPEG samples.11,20 We showed that using PBS decreases the baseline modulus of tendon, which is consistent with prior findings.22,23 We were particularly interested in any effects on transition and inflection point strains, as the stresses were all calculated using the cross-sectional area measured at the reference length, thus, it is unclear whether bath solution influenced changes in the behavior of cross-sectional area during loading, apart from the already increased cross-sectional area as a result of swelling. Although the transition and inflection point strains were not different between groups at the baseline, the ∆ value for transition strain was different. The ∆ measurements, meant to evaluate the mechanical damage induced in the tissue as a result of mechanical loading, showed some differences between groups. Thus, PBS alters the tissue-level mechanical behavior beyond the previously observed decreases in modulus. Specifically, these changes for transition point strain suggest that bath solution may have an effect on collagen fiber recruitment in the tissue.
At the microscale, SPEG samples illustrated a greater ability to recover microscale strain and sliding compared to PBS. PBS samples also showed a lower magnitude of microscale strain during mechanical loading compared to SPEG, further supporting our conclusion from the micro:tissue-scale strain ratio that PBS samples have reduced loading of the fibrils. As PBS increases the interfibrillar spacing of collagen fibrils, the ability of the tissue to bear load via interfibrillar shear could be restricted, leading to the observed reduction in load-bearing capacity, tissue level modulus, and microscale to tissue strain ratio.18,22,27
Unexpectedly, SPEG samples had larger magnitude ∆ values for modulus, transition point strain, and inflection point stress. The larger ∆, which corresponds to an increased amount of tissue-level damage, could be a result of the changes induced in the PBS samples from swelling prior to mechanical loading. That is, the ∆ modulus for the SPEG group as a result of mechanical loading is larger in magnitude because the PBS modulus was already reduced as a result of swelling prior to mechanical loading. Whether or not this apparent decrease in material properties due to tissue swelling is reversible is a point for further investigation, though these effects have been seen to be reversible in other fibrous tissues.6
The TEM images illustrate the structural changes as a result of bath solution on collagen fibril diameter and density. The % area density of fibrils was larger in both Fresh and SPEG groups than in PBS, showing that the tissue swelling decreases the collagen fibril density. This decrease in density reduces the amount of possible shear transfer by reducing contact between fibrils, altering the load sharing between collagen fibrils and influencing the observed changes in mechanical behavior and damage. Contrary to our expectation, the fibril diameter medians showed no difference between any groups, though the distributions were all different. It is possible that there is a difference which is lost due to the relatively low sample size for medians (n = 3/group). Additionally, the high diameter distributions of Fresh and SPEG samples may be affected by their high densities. The high densities decrease resolution, first by hindering the perfusion of staining medium and resin into the tissue; second, the high-density samples have fibrils in much more direct contact with each other. Both of these limitations make the defined boundaries between fibrils harder to define in the Fresh and SPEG samples, particularly for the boundaries of smaller fibrils. (Supplementary Fig. 1). It is also possible that the large PEG molecules restrict diffusion of the fixation solutions into the tendon, further hindering image quality. The resulting distributions may thus not be adequately reporting the amount of smaller diameter fibrils in the Fresh and SPEG samples. Though the resolution challenges made the definition of distinct boundaries difficult, the difference between fibril and matrix was still clear, and thus the % area density measurement was not affected to nearly the same extent by the resolution change. Overall, these TEM results show clear structural changes to tendon fascicles as a result of bath solution choice, with SPEG appearing to more similar to Fresh, which may help explain the altered mechanical behavior with PBS.
The use of various salts and differing hydration levels has been shown to alter the self-assembly of collagen fibrils, as well as mechanics of collagen’s molecular triple helix.14,15 It thus possible that the large, hydrophilic PEG molecules present in the SPEG buffer may alter the surface hydration of the collagen triple helix.14 Also, the difference between the Tris and phosphate ions in the respective buffers could alter the intrafibrillar collagen mechanics.15 However, this study was focused on the geometric changes induced by the buffers and the resulting effect on mechanics. A discussion of the chemical mechanisms within the collagen fibrils is beyond the scope of this study.
The mechanical effects of altered water content have been observed in other tissues.3,6 Tendon’s uniaxial fibers leave the tissue relatively unrestrained to swell in the lateral direction. Tissues which have a more complex fiber network, such as articular cartilage or cornea, may therefore experience less swelling. A study with annulus fibrosus showed swelling in PBS; however, the samples were excised and sectioned to release residual stress in the fibers and thus freed the tissue for lateral swelling.6 While some of these previous studies were able to have a fresh-frozen control,6,20,21,–23 our test duration and the small cross-section of rat tail tendon made this unfeasible. A recent study done in human iliotibial band investigated the effect of water content on tissue and microscale properties using atomic force microscopy and tensile testing. The results of this study similarly found that micro- and tissue level mechanics were altered with changes in water content.16 The effect of choice of bath solution on swelling and mechanics in the rat tail tendon demonstrated here are likely to also occur in other fibrous tissues, as PBS equilibration effects the interfibrillar space of collagen in annulus fibrosus, meniscus, human tendon, and ligament.1,3,6,16 However, the magnitude of these effects are likely to be tissue and species specific due to differences in composition, fiber density and alignment, and size.
With this study, we have shown that the osmotic pressure of bath solution changes the microscale loading and mechanical damage in tendon, in addition to altering microstructure and tissue-level mechanical behavior. The mechanical protocol completed in this study was about an hour in duration following at least an hour of bath equilibration, and involved only a single ramp, hold, and recovery period before the Diagnostic ramp. Longer duration tests or tests with repeated loading such as cyclic fatigue may be further affected by bath osmotic pressure. Rat tail tendon is a commonly used model for studying tendon mechanics and degeneration, and due to its small size and diameter may be especially susceptible to bath solution effects.
In conclusion, this study demonstrates the differences between a PBS and SPEG bath on tendon microstructure and mechanical behavior. The TEM imaging, in which tendon microstructure in SPEG appears similar to Fresh tendon, suggests that SPEG bath may better represent Fresh tissue mechanical behavior by reducing the swelling that occurs with PBS. Thus, SPEG may be a more appropriate choice for bathing solution for mechanical testing of tendon, especially for samples with a small cross section. Previous tests completed in PBS are still valid as long as appropriate control groups were used; however, true tissue properties measured from experiments with PBS baths should be used with careful consideration for modeling. Although previous studies have illustrated that PBS alters tendon modulus, hydration, and microstructure, our study shows that PBS also increases microscale damage in tendon and alters multiscale mechanics, compared to an SPEG bath that does not induce swelling. Future mechanical testing should consider using SPEG as a bath solution with an osmotic pressure which preserves fresh tissue water content.
References
Andrews, S. H. J., J. B. Rattner, N. G. Shrive, and J. L. Ronsky. Swelling significantly affects the material properties of the menisci in compression. J. Biomech. 48:1485–1489, 2015.
Baylon, E. G., and M. E. Levenston. Osmotic swelling responses are conserved across cartilaginous tissues with varied sulfated-glycosaminoglycan contents. J. Orthop. Res. 2018. https://doi.org/10.1101/459115.
Chimich, D., N. Shrive, C. Frank, L. Marchuk, and R. Bray. Water content alters viscoelastic behaviour of the normal adolescent rabbit medial collateral ligament. J. Biomech. 25:831–837, 1992.
Eisenberg, S. R., and A. J. Grodzinsky. Swelling of articular cartilage and other connective tissues: electrornechanochemical forcesat. J. Orthop. Res. 1985. https://doi.org/10.1002/jor.1100030204.
Han, W. M., S. J. Heo, T. P. Driscoll, J. F. Delucca, C. M. McLeod, L. J. Smith, R. L. Duncan, R. L. Mauck, and D. M. Elliott. Microstructural heterogeneity directs micromechanics and mechanobiology in native and engineered fibrocartilage. Nat. Mater. 15:477–484, 2016.
Han, W. M., N. L. Nerurkar, L. J. Smith, N. T. Jacobs, R. L. Mauck, and D. M. Elliott. Multi-scale structural and tensile mechanical response of annulus fibrosus to osmotic loading. Ann. Biomed. Eng. 40:1610–1621, 2012.
Hannafin, J. A., and S. P. Arnoczky. Effect of cyclic and static tensile loading on water content and solute diffusion in canine flexor tendons: Anin Vitro study. J. Orthop. Res. 12:350–356, 1994.
Hara, O., J. P. G. Urban, and A. Maroudas. Influence of cyclic loading on the nutrition of articular cartilage. Ann. Rheum. Dis. 49:536–539, 1990.
Karis Allen, J. J., and S. P. Veres. Effect of testing temperature on the nanostructural response of tendon to tensile mechanical overload. J. Biomech. 2020. https://doi.org/10.1016/j.jbiomech.2020.109720.
Katz, E. P., and S. T. Li. The intermolecular space of reconstituted collagen fibrils. J. Mol. Biol. 73:351–369, 1973.
Lee, A. H., and D. M. Elliott. Freezing does not alter multiscale tendon mechanics and damage mechanisms in tension. Ann. N. Y. Acad. Sci. 1409:85–94, 2017.
Lee, A. H., and D. M. Elliott. Multi-scale loading and damage mechanisms of plantaris and rat tail tendons. J. Orthop. Res. 2019. https://doi.org/10.1002/jor.24309.
Lee, A. H., S. E. Szczesny, M. H. Santare, and D. M. Elliott. Investigating mechanisms of tendon damage by measuring multi-scale recovery following tensile loading. Acta Biomater. 57:363–372, 2017.
Leikin, S., V. A. Parsegian, W.-H. Yang, and G. E. Walrafen. Raman spectral evidence for hydration forces between collagen triple helices. Proc. Natl. Acad. Sci. U.S.A. 94:11312–11317, 1997.
Li, Y., and E. P. Douglas. Effects of various salts on structural polymorphism of reconstituted type I collagen fibrils. Colloids Surf. B 112:42–50, 2013.
Lozano, P. F., M. Scholze, C. Babian, H. Scheidt, F. Vielmuth, J. Waschke, B. Ondruschka, and N. Hammer. Water-content related alterations in macro and micro scale tendon biomechanics. Sci. Rep. 9:7887, 2019.
Lujan, T. J., C. J. Underwood, H. B. Henninger, B. M. Thompson, and J. A. Weiss. Effect of dermatan sulfate glycosaminoglycans on the quasi-static material properties of the human medial collateral ligament. J. Orthop. Res. 25:894–903, 2007.
Muench, J. R., D. G. Thelen, and C. R. Henak. Interfibrillar shear behavior is altered in aging tendon fascicles. Biomech: Model. Mechanobiol, 2019. https://doi.org/10.1007/s10237-019-01251-0.
Parsegian, V. A., R. P. Rand, N. L. Fuller, and D. C. Rau. Osmotic stress for the direct measurement of intermolecular forces. Methods Enzymol. 127:400–416, 1986.
Safa, B. N., K. D. Meadows, S. E. Szczesny, and D. M. Elliott. Exposure to buffer solution alters tendon hydration and mechanics. J. Biomech. 2017. https://doi.org/10.1016/j.jbiomech.2017.06.045.
Schindelin, J., I. Arganda-Carreras, E. Frise, V. Kaynig, M. Longair, T. Pietzsch, S. Preibisch, C. Rueden, S. Saalfeld, B. Schmid, J. Tinevez, D. J. White, V. Hartenstein, K. Eliceiri, P. Tomancak, and A. Cardona. Fiji: an open-source platform for biological-image analysis. Nature Methods. 9:676–682, 2012.
Screen, H. R. C., V. H. Chhaya, S. E. Greenwald, D. L. Bader, D. A. Lee, and J. C. Shelton. The influence of swelling and matrix degradation on the microstructural integrity of tendon. Acta Biomater. 2:505–513, 2006.
Screen, H. R. C., J. C. Shelton, V. H. Chhaya, M. V. Kayser, D. L. Bader, and D. A. Lee. The influence of noncollagenous matrix components on the micromechanical environment of tendon fascicles. Ann. Biomed. Eng. 33:1090–1099, 2005.
Shahmirzadi, D., and A. H. Hsieh. An efficient technique for adjusting and maintaining specific hydration levels in soft biological tissues in vitro. Med. Eng. Phys. 32:795–801, 2010.
Steuter, A. A., A. Mozafar, and J. R. Goodin. Water potential of aqueous polyethylene glycol. Plant Physiol. 67:64–67, 1981.
Sverdlik, A., and Y. Lanir. Time-dependent mechanical behavior of sheep digital tendons, including the effects of preconditioning. J. Biomech. Eng. 124:78, 2002.
Szczesny, S., and D. Elliott. Interfibrillar shear stress is the loading mechanism of collagen fibrils in tendon. Acta Biomater. 86:3279–3288, 2008.
Szczesny, S. E., K. L. Fetchko, G. R. Dodge, and D. M. Elliott. Evidence that interfibrillar load transfer in tendon is supported by small diameter fibrils and not extrafibrillar tissue components HHS public access. J. Orthop. Res. 35:2127–2134, 2017.
Travascio, F., A. R. Jackson, M. D. Brown, and W. Y. Gu. Relationship between solute transport properties and tissue morphology in human annulus fibrosus. J. Orthop. Res. 27:1625–1630, 2009.
Acknowledgments
This research was supported by National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases Grant No. AR070966, and a Delaware INBRE Core Access award supported by National Institutes of Health, National Institute of General Medical Sciences Grant No. P20GM103446. We thank the Bioimaging Center at the Delaware Biotechnology Institute for data acquisition, and Shannon Modla for the electron microscopy work.
Conflict of interest
The authors have no conflicts of interest related to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Peter E. McHugh oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bloom, E.T., Lee, A.H. & Elliott, D.M. Tendon Multiscale Structure, Mechanics, and Damage Are Affected by Osmolarity of Bath Solution. Ann Biomed Eng 49, 1058–1068 (2021). https://doi.org/10.1007/s10439-020-02649-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-020-02649-z