Abstract
Background
Sexual dysfunction (SD) is reported in neurological conditions similar to Friedreich ataxia (FRDA). Anecdotally individuals with FRDA report SD including erectile dysfunction and altered genital sensation. Understanding SD in FRDA assists health professionals identify SD issues and improve healthcare for individuals with FRDA.
Objective
To quantify if, and to what extent, people with FRDA experience challenges with sexual function and intimate relationships as a result of primary (genital function), secondary (physical) and tertiary (psychosocial) dysfunction.
Methods
An online purpose designed anonymous questionnaire explored SD and intimate relationships. Invitations to participate were sent to individuals with FRDA aged 18 years and over on the Ataxia UK and Friedreich Ataxia Research Alliance databases. Date collection occurred between January and July, 2017.
Results
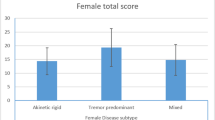
One-hundred-and-seventy-nine adults with FRDA participated, of which 107 reported current or previous sexual activity. Erectile dysfunction was reported in 57% (20/35) of males, inadequate vaginal lubrication interfering with sexual responsiveness was reported in 57.7% (26/45) of females, and 47% (51/107) reported reduced genital sensation. In addition, 88% (94/107) reported problems moving their body during sexual activity and 73% (78/107) reported reduced confidence about their sexuality due to FRDA. A significant negative relationship was shown between younger age of disease onset and SD.
Conclusion
This study confirmed FRDA impacts sexual functioning, sexual satisfaction and the capacity to form intimate relationships. Understanding the nature and extent of SD is critical to developing interventions and recommendations designed to enhance sexual function, sexuality, and intimate relationships for individuals with FRDA.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Delatycki MB, Corben LA (2012) Clinical features of Friedreich ataxia. J Child Neurol 27:1133–1137
Calabro RS, Russo M, Dattola V et al (2018) Sexual function in young individuals with multiple sclerosis: does disability matter? J Neurosci Nurs 50:161–166
Nasimbera A, Rosales J, Silva B et al (2018) Everything you always wanted to know about sex and Neurology: neurological disability and sexuality. Arq Neuropsiquiatr 76(7):430–435
Khan F, Pallant JF, Ng L, Whishaw M (2011) Sexual dysfunction in multiple sclerosis. Sex Disabil 29:101–111
Rosen RC, Fisher WA, Eardley I et al (2004) The multinational Men’s Attitudes to Life Events and Sexuality (MALES) study: I. Prevalence of erectile dysfunction and related health concerns in the general population. Curr Med Res Opin 20(5):607–617
Ishak IH, Low WY, Othman S (2010) Prevalence, risk factors, and predictors of female sexual dysfunction in a primary care setting: a survey finding. J Sex Med 7(9):3080–3087
Lad M, Parkinson MH, Rai M et al (2017) Urinary, bowel and sexual symptoms in a cohort of patients with Friedreich’s ataxia. Orphanet J Rare Dis 12:158
Nortvedt MW, Riise T, Frugård J et al (2007) Prevalence of bladder, bowel and sexual problems among multiple sclerosis patients two to five years after diagnosis. Multiple Sclerosis 13:106–112
Esmail S, Munro B, Gibson N (2007) Couple’s experience with multiple sclerosis in the context of their sexual relationship. Sex Disabil 25:163–177
Schairer L, Foley F, Zemon V et al (2014) The impact of sexual dysfunction on health-related quality of life in people with multiple sclerosis. Multiple Sclerosis 20:610–616
O’Dea S, Shuttleworth R, Wedgwood N (2012) Disability, doctors and sexuality: do healthcare providers influence the sexual wellbeing of people living with a neuromuscular disorder? Sex Disabil 30:171–185
Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Sanders A, Foley F, LaRocca N, Zemon V (2000) The multiple sclerosis intimacy and sexuality questionnaire-19 (MSISQ-19). Sex Disabil 18:3–26
Foley F, Sanders A (1997) Sexuality, multiple sclerosis, and women. MS Manage 4:1–10
Rosen R, Cappelleri J, Smith M, Lipsky J, Peña B (1999) Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 11:319–326
Rosen R, Brown C, Heiman J et al (2000) The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Mar Ther 26:191–208
Quirk F, Haughie S, Symonds T (2005) The use of the sexual function questionnaire as a screening tool for women with sexual dysfunction. J Sex Med 2:469–477
Musegante A, Almeda P, Monteiro R, Bassoro U (2013) Urinary symptoms and urodynamics findings in patients with Friedreich’s ataxia. Int Braz J Urol 39:867–874
Avery K, Donovan J, Peters T, Shaw C, Gotoh M, Abrams P (2004) ICIQ: a brief and robust measure for evaluatating the symptoms and impact of urinary incontinence. Neurourol Urodynam 23:322–330
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psych 4:561–571
Spencer RMC, Ivry RB (2013) Cerebellum and timing. In: Manto M, Schmahmann JD, Rossi F, Gruol DL, Koibuchi N (eds) Handbook of the cerebellum and cerebellar disorders. Springer, Dordrecht
Taleporos G, McCabe M (2002) Body image and physical disability: personal perspectives. Soc Sci Med 54:971–980
McCabe M, Taleporos G (2003) Sexual esteem, sexual satisfaction and sexual behaviour amoung people with physical disability. Arch Sex Beh 32:359–369
Epstein E, Farmer JM, Tsou A et al (2008) Health related quality of life measures in Friedreich Ataxia. J Neurol Sci 272:123–128
Nieto A, Hernandez-Torres A, Perez-Flores J, Monton F (2018) Depressive symptoms in Friedreich ataxia. Int J Clin Health Psychol 18:18–26
Wilson C, Fahey MC, Corben LA et al (2007) Quality of life in Friedreich Ataxia: what clinical, social and demographic factors are important? Europ J Neurol 14:1040–1047
Tepper M (2000) Sexuality and disability: the missing discouse of pleasure. Sex Disabil 18:283–290
Corben LA, Lynch DR, Pandolfo M, Schulz J, Delatycki MB (2014) Consensus clinical management guidelines for Friedreich ataxia. Orph J Rare Dis 9:184
Lundberg PO, Ertekin C, Ghezzi A, Swash M, Vodusek D (2001) Neurosexology. Eur J Neurol 8:2–24
Basson R, Bronner G (2015) Management and rehabilitation of neurologic patients with sexual dysfunction. Handb Clin Neurol 130:415–434
Acknowledgements
The authors wish to thank Ms Jen Farmer, Chief Executive Officer, Friedreich Ataxia Research Alliance (USA) and Dr Julie Greenfield, Ataxia-UK for their assistance in distributing information regarding the survey. The authors are grateful to all respondents to the survey for their time and insightful comments. We would also like to acknowledge the Friedreich Ataxia Research Alliance (USA) for their support of our work.
Funding
Associate Professor Louise Corben is supported by a Medical Research Futures Fund Next Generation Career Development Fellowship under Grant APP1143098.
Author information
Authors and Affiliations
Contributions
LAC was responsible for the conception, organisation and execution of the research study, design and execution of the statistical analysis and writing of first draft of the manuscript. MMH was responsible for the organisation and execution of the research study, and review and critique of the manuscript. AM was responsible for the organisation and execution of the research study, and review and critique of the manuscript. LMC was responsible for the organisation and execution of the research study, review of the statistical analysis and review and critique of the manuscript. MBD was responsible for the conception, organisation and execution of the research study and review and critique of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None to report.
Ethical approval
This study was approved by the Royal Children’s Hospital, Victoria Australia, Human Research Ethics Committee (HREC 35276 A).
Rights and permissions
About this article
Cite this article
Corben, L.A., Hermans, M.M., Marks, A. et al. Sexual function, intimate relationships and Friedreich ataxia. J Neurol 268, 1088–1095 (2021). https://doi.org/10.1007/s00415-020-10258-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10258-y