Abstract
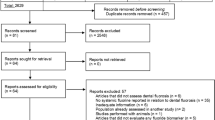
Exposure to mercury is an important risk to dentists health. The aim of the present study was to assess the pooled mean mercury level (MML) in the urine, blood, nail, and hair of Iranian dentists (IDs) through the meta-analysis technique. Comprehensive and systematic searches were performed in main local databases including SID, Magiran, Iran medex, and ISC as well as internationally available databases including Embase, PubMed and Scopus for all the relevant studies up to 2018. In order to prevent bias in this study and identify eligible studies, various steps of the study was performed independently by two researchers. Out of 13 studies in the meta-analysis process which included 1499 IDs, the mean of the mercury level in the urine, nail, and blood was estimated to be 6.29 (95% CI: 2.61–9.97, I-square: 62.7%, P: 0.006), 3.54 (95% CI: 2.81–4.28, I-square: 0.0%, P: 0.968), 11.20 (95% CI: 2.28–20.13, I-square: 59.9%, P: 0.082), respectively. The mean mercury level (MML) in the biological samples of IDs was higher than the standard of World Health Organization (WHO). So, in accordance with Article 10 of the European Union Regulations (EUR), in the context of the Minamata Convention (MC) on Dental Amalgam (DA), in order to avoid the dangers of mercury exposure in dentists, it is necessary for Iran and other countries to approve laws and to implement a national plan to reduce mercury levels and replace the appropriate materials.







Similar content being viewed by others
Abbreviations
- BML:
-
Blood Mercury Level
- UML:
-
Urine Mercury Level
- HML:
-
Hair Mercury Level
- IDs:
-
Iranian Dentists
- MML:
-
Mean Mercury Level
- MC:
-
Minamata Convention
- SD:
-
Standard Deviation
- EMVs:
-
Elemental Mercury Vapors
- DA:
-
Dental Amalgam
References
Streets DG, Horowitz HM, Jacob DJ, Lu Z, Levin L, ter Schure AFH, et al. Total Mercury Released to the Environment by Human Activities. Environ Sci Technol. 2017;51(11):5969–77.
Duffus John H. Heavy metal” a meaningless term? (IUPAC Technical Report). Pure Appl Chem. 2002. p 793.
Engwa GA, Ferdinand PU, Nwalo FN, Unachukwu MN. Mechanism and Health Effects of Heavy Metal Toxicity in Humans. In: Karcioglu, Ozgur and Arslan, Banu, editors. Poisoning in the Modern World - New Tricks for an Old Dog? : IntechOpen; 2019.
Saleh HN, Panahande M, Yousefi M, Asghari FB, Conti GO, Talaee E et al. Carcinogenic and non-carcinogenic risk assessment of heavy metals in groundwater wells in Neyshabur Plain, Iran. Biological trace element research. 2019;190(1):251–61.
Rahman Z, Singh VP. The relative impact of toxic heavy metals (THMs) (arsenic (as), cadmium (cd), chromium (Cr)(VI), mercury (hg), and lead (Pb)) on the total environment: an overview. Environ Monit Assess. 2019;191(7):419.
Bjorklund G, Bengtsson U, Chirumbolo S, Kern JK. Concerns about environmental mercury toxicity: do we forget something else? Environ Res. 2017;152:514–6.
Bjørklund G, Hilt B, Dadar M, Lindh U, Aaseth J. Neurotoxic effects of mercury exposure in dental personnel. Basic Clin Pharmacol Toxicol. 2019;124(5):568–74.
Mishra S, Bharagava RN, More N, Yadav A, Zainith S, Mani S, et al. Heavy metal contamination: an alarming threat to environment and human health. In: Sobti RC, Arora NK, Kothari R, editors. Environmental biotechnology: for sustainable future. Singapore: Springer Singapore; 2019. p. 103–25.
Mahmoudi N, Jonidi Jafari A, Moradi Y, Esrafili A. The mercury level in hair and breast milk of lactating mothers in Iran: a systematic review and meta-analysis. J Environ Health Sci Eng. 2020
ATSDR. The priority list of hazardous substances that will be the candidates for toxicological profiles. Agency for Toxic Subs and Disease Registry. 2015.
ATSDR. “Toxicological Profile for Mercury.” Atlanta, Georgia Agency for Toxic Substances and Disease Registry, Ctr Dis Control Prev. 1999.
Basu N, Horvat M, Evers DC, Zastenskaya I, Weihe P, Tempowski J. A state-of-the-science review of mercury biomarkers in human populations worldwide between 2000 and 2018. Environ Health Perspect. 2018;126(10):106001.
Clarkson TW, Magos L. The Toxicology of Mercury and Its Chemical Compounds. Crit. Rev Toxicol 2006;36(8):609–62.
Eagles-Smith CA, Silbergeld EK, Basu N, Bustamante P, Diaz-Barriga F, Hopkins WA, et al. Modulators of mercury risk to wildlife and humans in the context of rapid global change. Ambio. 2018 March 01;47(2):170–97.
Ha E, Basu N, Bose-O’Reilly S, Dórea JG, McSorley E, Sakamoto M, et al. Current progress on understanding the impact of mercury on human health. Environ Res 2017;152:419–33.
JECFA. Methylmercury (addendum). In: Safety Evaluation of Certain Food Additives and Contaminants. Prepared by the sixty-seventh meeting of the Joint FAO/WHO Expert Committee on Food Additives(JECFA). Food Additives Series 58. Geneva, Switzerland: World Health Organization, 269–315. http://www.inchem.org/documents/jecfa/jecmono/v58je01.pdf [Accessed 14 December 2019]; 2007a.
JECFA. “Methylmercury Evaluation of Certain Food Additives and Contaminants.” Sixty-seventh Report of the Joint FAO/WHO Expert Committee on Food Additives. WHO Technical Report Series 940. . Geneva, Switzerland: World Health Organization/Food and Agriculture Organization. http://apps.who.int/iris/bitstream/10665/43592/1/WHO_TRS_940_eng.pdf [Accessed 14 December 2019]. 2007b.
JECFA. “Safety Evaluation of Certain Contaminants in Food.” Prepared by the Seventy-second meeting of the Joint FAO/WHO Expert Committee on Food Additives(JECFA). Food Additives Series 63. Geneva, Switzerland: World Health Organization. http://www.inchem.org/documents/jecfa/jecmono/v63je01.pdf [Accessed 14 December 2019]; 2011.
NRC. Toxicological Effects of Methylmercury. Washington, DC: National Academies Press. National Research Council 2000.
U.S.EPA. Mercury Study Report to Congress. U.S. Environmental Protection Agency. https://www.epa.gov/mercury/mercury-study-report-congress [Accessed 14 December 2019]; 1997.
U.S.EPA. Chapter 4: risk assessment for methylmercury. In: “Water Quality Criterion for the Protection of Human Health: Methylmercury.” EPA-823-R-01-001 Washington, DC: U.S. EPA, Office of Science and Technology, Office of Water; 2001
WHO. “Methylmercury”. Environmental Health Criteria 101. . Geneva, Switzerland: World Health Organization, International Program on Chemical Safety. http://www.inchem.org/documents/ehc/ehc/ehc101.htm [Accessed 14 December 2019]. 1990.
WHO. “Elemental Mercury and Inorganic Mercury Compounds: Human Health Aspects.” Concise International Chemical Assessment Document No. 50. Geneva, Switzerland World Health Organization, International Program on Chemical Safety. http://www.who.int/ipcs/publications/cicad/en/cicad50.pdf?ua=1 [Accessed 14 December 2019]. 2003.
Rice KM, Walker EM Jr, Wu M, Gillette C, Blough ER. Environmental mercury and its toxic effects. J Prev Med Public Health. 2014;47(2):74–83.
Lamborg CH, Hammerschmidt CR, Bowman KL, Swarr GJ, Munson KM, Ohnemus DC, et al. A global ocean inventory of anthropogenic mercury based on water column measurements. Nature. 2014;512(7512):65–8.
Sundseth K, Pacyna JM, Pacyna EG, Pirrone N, Thorne RJ. Global sources and pathways of mercury in the context of human health. Int J Environ Res Public Health. 2017;14(1):105. https://doi.org/10.3390/ijerph14010105.
Ali W, Junaid M, Aslam MW, Ali K, Rasool A, Zhang H. A review on the status of mercury pollution in Pakistan: sources and impacts. Arch Environ Contam Toxicol. 2019 May 01;76(4):519–27.
Park J-D, Zheng W. Human exposure and health effects of inorganic and elemental mercury. J Prev Med Public Health. 2012;45(6):344–52.
Service BI. Study on the potential for reducing mercury pollution from dental amalgam and batteries Brussels Final report prepared for the European Commission – Directorate General for Environment: https://ec.europa.eu/environment/chemicals/mercury/pdf/final_report_110712.pdf; 2012.
Berlin M, Zalups RK, Fowler BA. Chapter 46 - mercury. In: Nordberg GF, Fowler BA, Nordberg M, editors. Handbook on the toxicology of metals (Fourth Edition). San Diego: Academic Press; 2015. p. 1013–75.
Nagpal N, Bettiol SS, Isham A, Hoang H, Crocombe LA. A Review of Mercury Exposure and Health of Dental Personnel. Saf Health Work. 2017;8(1):1–10.
Bernhoft RA. Mercury Toxicity and Treatment: A Review of the Literature. J Environ Public Health. 2012;2012:Article ID 460508:10.
Assari MJ, Fatemi F. A guide to mercury exposure in the workplace. Tehran, Ministry of health and medical education(MHME), Environmental and occupational health center: Institute for environment research (Tehran university of medical science); 2015.
Gibb H, O’Leary KG. Mercury exposure and health impacts among individuals in the artisanal and small-scale gold mining community: a comprehensive review. Environ Health Perspect. 2014;122(7):667–72.
Tchounwou PB, Yedjou CG, Patlolla AK, Sutton DJ. Heavy metal toxicity and the environment. In: Luch A, editor. Molecular, clinical and environmental toxicology: volume 3: environmental toxicology. Basel: Springer Basel; 2012. p. 133–64.
Andreoli V, Sprovieri F. Genetic aspects of susceptibility to mercury toxicity: an overview. Int. J Environ Res Public Health. 2017;14(1):93. https://doi.org/10.3390/ijerph14010093.
Bjørklund G, Tinkov AA, Dadar M, Rahman MM, Chirumbolo S, Skalny AV, et al. Insights into the potential role of mercury in Alzheimer’s disease. J Mol Neurosci. 2019;67(4):511–33.
Bravo M, Parra S, Quiroz W, Neaman A. Human exposure assessment to mercury through hair analysis in coastal villages of the valparaiso region (CHILE). J Chil Chem Soc. 2019;64(2):4480–3.
Genchi G, Sinicropi MS, Carocci A, Lauria G, Catalano A. Mercury Exposure and Heart Diseases. Int J Environ Res. Public Health. 2017;14(1):74.
Henriques MC, Loureiro S, Fardilha M, Herdeiro MT. Exposure to mercury and human reproductive health: A systematic review Reprod Toxicol. 2019;85:93–103.
Hong Y-S, Kim Y-M, Lee K-E. Methylmercury exposure and health effects. J Prev Med Public Health. 2012;45(6):353–63.
Rana MN, Tangpong J, Rahman MM. Toxicodynamics of lead, cadmium, mercury and arsenic-induced kidney toxicity and treatment strategy: a mini review. Toxicol Rep. 2018;5:704–13.
Smiechowicz J, Skoczynska A, Nieckula-Szwarc A, Kulpa K, Kübler A. Occupational mercury vapour poisoning with a respiratory failure, pneumomediastinum and severe quadriparesis. SAGE Open Med Case Rep. 2017;5:2050313X17695472–2050313X.
Xu X, Nie S, Ding H, Hou FF. Environmental pollution and kidney diseases. Nat Rev Nephrol. 2018;14(5):313–24.
Kim J-J, Kim Y-S, Kumar V. Heavy metal toxicity: An update of chelating therapeutic strategies. J Trace Elem Med Biol. 2019;54:226–31.
Kim K-H, Kabir E, Jahan SA. A review on the distribution of Hg in the environment and its human health impacts. J. Hazard. Mater. 2016;306:376–85.
Turaga RMR, Howarth RB, Borsuk ME. Perceptions of Mercury Risk and Its Management. Human and Ecological Risk Assessment. An International Journal. 2014;20(5):1385–405.
Bengtsson UG, Hylander LD. Increased mercury emissions from modern dental amalgams. BioMetals. 2017 April 01;30(2):277–83.
WHO. “INORGANIC MERCURY”. Environmental Health Criteria 118. . Geneva, Switzerland: World Health Organization, International Program on Chemical Safety. http://www.inchem.org/documents/ehc/ehc/ehc118.htm [accessed 14 December 2019]. 1991.
WHO. Exposure to mercury: a major public health concern. Public Health and Environment, Geneva, Switzerland: World Health Organization: https://www.who.int/ipcs/features/mercury.pdf?ua=1; 2007.
Aaseth J, Hilt B, Bjørklund G. Mercury exposure and health impacts in dental personnel. Environ. Res. 2018;164:65–9.
Haque N, Yousaf S, Nejatian T, Youseffi M, Mozafari M, Sefat F. 6 - Dental amalgam. In: Khurshid Z, Najeeb S, Zafar MS, editors. Sefat F, editors. Advanced Dental Biomaterials: Woodhead Publishing; 2019. p. 105–25.
Environment Mot. Bans mercury in products. Press release: Ministry of the Environment: https://www.regjeringen.no/en/historical-archive/Stoltenbergs-2nd-Government/Ministry-of-the-Environment/Nyheter-og-pressemeldinger/pressemeldinger/2007/Bans-mercury-in-products/id495138/ (Accessed 1 December 2019); 2007.
Agency SC. The Swedish Chemicals Agency’s Chemical products and biotechnical Organisms regulations. KIFS 2008: 2 in English, consolidated up to KIFS 2012: 3. 2008-2012.
Coulter MA. Minamata Convention on Mercury. International Legal Materials, Cambridge University Press. 2017;55(3):582–616. Epub 01/20.
You M. Interpretation of the source-specific substantive control measures of the Minamata Convention on Mercury. Environ Int. 2015;75:1–10.
Mahmoudi N, Jonidi Jafari A, Moradi Y, Esrafili A. The mercury level in hair and breast milk of lactating mothers in Iran: a systematic review and meta-analysis. J Environ Health Sci Eng. 2020;18(1):355–66.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Wells G. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomised studies in meta-analyses. http://wwwohrica/programs/clinical_epidemiology/oxfordasp. 2001.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Accessed 14 December 2019]. 2011.
Wang Q, Huang Q, Zeng Y, Jj L, Sy L, Gu X, et al. Parity and osteoporotic fracture risk in postmenopausal women: a dose-response meta-analysis of prospective studies. Osteoporos. Int. 2016;27(1):319–30.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005;5(1):13.
Shirkhanloo H, Fallah Mehrjerdi MA, Hassani H. Identifying occupational and nonoccupational exposure to mercury in dental personnel. Arch Environ Occup Health. 2017;72(2):63–9.
Kasraei S, Mortazavi H, Vahedi M, Bakianian Vaziri P, Assary M. Blood Mercury Level and Its Determinants among Dental Practitioners in Hamadan. Iran. J Dent (Tehran). 2010;Spring;7(2):55–63.
Sadeghneiat K, Pahlevan D. Blood mercury levels of dental students and dentists at Dental School of Tehran University. koomesh. 2007;8(4):223–8. eng.
Ostadi A, Falsafi P, Pourzare Mehrbani S, Dolatkhah H, Fakhrzadeh V, Motamed A, et al. Dental amalgam exposure and urinary mercury levels in dentists. Pharmacophore. 2017;8(6S):e-117356.
Daghayeghi AH, Ashraf H, Darmiani S. Evaluation of urinary mercury levels in dentists of dentistry department of Ahvaz oil industrys health care, in 2010. International Research Journal of Applied and Basic Sciences. 2014;8(8):1140–3.
Akbari M, Velayati Moghadam F, Ahmadi A. Evaluation of factors influencing urine mercury levels of general dentists and restorative specialists in Mashhad in a one-year period. Journal of Isfahan Dental School. 2013;8(7):652–61.
Neghab M, Choobineh A, Hassan Zadeh J, Ghaderi E. Symptoms of intoxication in dentists associated with exposure to low levels of mercury. Ind Health. 2011;49(2):249–54 Epub 2010/12/22. eng.
Zavvar Mousavi H, Rouhollahi A, Shirkhanloo H. Determination of mercury concentration in the air of dental clinics and the urines of their personnel with cold vapor atomic absorption spectrometry. Iranian Journal of Toxicology. 2009;2(4):287–91.
Zolfaghari G, Esmaili-Sari A, Ghasempouri SM, Faghihzadeh S. Evaluation of environmental and occupational exposure to mercury among Iranian dentists. Science of The Total Environment. 2007;381(1):59–67.
Hasani-Tabatabaei M, Golbabaei F, Shariatei B. Evaluation of urine mercury level of dentists in Tehran and its influencial factors. J. Dent. Med. 2006;19(3):66–75.
Esmaili Sari A, Zolfaghari G, Ghasempouri SM, Shayegh S, Shojaeddin HTM. Effect of Age, Gender, Years of Practice, Specialty and Number of Amalgam restorations on Mercury Concentration in Nails of dentists practicing in Tehran. The Journal of Islamic Dental Association of IRAN (JIDA). 2007;19(1):97–104.
Khamverdi Z, Assari MJ, Maleki K. Evaluation of urinary mercury concentration of dentists with more than 4 years experience in Hamadan. Journal of islamic dental association of iran. 2004;16(2):42–8.
Nasiri P, Golbabaie F, Mahmodi M. Occupational health Analysis in dentists of Tehran. J. Dent. Med. 1993;6(2):26–33.
Warwick D, Young M, Palmer J, Ermel RW. Mercury vapor volatilization from particulate generated from dental amalgam removal with a high-speed dental drill – a significant source of exposure. Journal of Occupational Medicine and Toxicology. 2019;14(1):22.
Burke FT. Minamata: what the practising dentist needs to know. Dental Update. 2018;45(6):579–80.
UNEP. “INC7”. Minamata Convention on Mercury Geneva, Switzerland: United Nations Environmental Program: http://www.mercuryconvention.org/Countries/tabid/3428/Default.aspx [accessed 24 December 2019].
Goodrich JM, Chou H-N, Gruninger SE, Franzblau A, Basu N. Exposures of dental professionals to elemental mercury and methylmercury. J. Expo. Sci. Environ. Epidemiol. 2016;26(1):78–85.
Jamil N, Baqar M, Ilyas S, Qadir A, Arslan M, Salman M, et al. Use of mercury in dental silver amalgam: an occupational and environmental assessment. Biomed Res Int. 2016;2016:6126385.
Bjorklund G. [Mercury in the dental office. Risk evaluation of the occupational environment in dental care]. Tidsskrift for den Norske laegeforening : tidsskrift for praktisk medicin, ny raekke. 1991 Mar 20;111(8):948–51. Epub 1991/03/20. Kvikksolv i tannhelsepersonalets arbeidsmiljo. En risikovurdering av arbeidsmiljoet innen tannhelsetjenesten. nor.
Al-Saleh I, Aa A-S, Elkhatib R. Effect of mercury (Hg) dental amalgam fillings on renal and oxidative stress biomarkers in children. Sci. Total Environ. 2012;431:188–96.
Cesbron A, Saussereau E, Mahieu L, Couland I, Guerbet M, Goullé J-P. Metallic profile of whole blood and plasma in a series of 106 healthy volunteers. J Anal Toxicol. 2013;37(7):401–5.
U.S.FDA. epidemiological evidence on the adverse health effects reported in relation to mercury from dental amalgam: systematic literature review. U.S. Food and Drug Administration: https://www.fda.gov/media/131151/download. [accessed 24 December 2019]; 2019.
Samir AM, Aref WM. Impact of occupational exposure to elemental mercury on some antioxidative enzymes among dental staff. Toxicol Ind Health. 2011;27(9):779–86.
Tezel H, Ertas OS, Erakin C, Kayali A. Blood mercury levels of dental students and dentists at a dental school. Br Dent J. 2001;191(8):449–52.
Atesagaoglu A, Omurlu H, Ozcagli E, Sardas S, Ertas N. Mercury exposure in dental practice. Oper Dent. 2006;31(6):666–9.
Ngim CH, Foo SC, Boey KW, Jeyaratnam J. Chronic neurobehavioural effects of elemental mercury in dentists. Br J Ind Med. 1992;49(11):782–90.
Battistone GC, Hefferren JJ, Miller RA, Outright DE. Mercury: its relation to the dentist’s health and dental practice characteristics. J Am Dent Assoc. 1976;92(6):1182–8.
Parajuli RP, Goodrich JM, Chou H-N, Gruninger SE, Dolinoy DC, Franzblau A, et al. Genetic polymorphisms are associated with hair, blood, and urine mercury levels in the American Dental Association (ADA) study participants. Environ. Res. 2016;149:247–58.
Yilmaz H, Tutkun E, Demiralp KO, Yilmaz FM, Aliyev V, Soylemezoglu T. Exposure to mercury among dental health workers in Turkey: correlation with amalgam work and own fillings. Toxicol Ind Health. 2015;31(10):951–4.
Moller-Madsen B, Hansen JC, Kragstrup J. Mercury concentrations in blood from Danish dentists. Scand J Dent Res. 1988;96(1):56–9.
UNEP, WHO. Guidance for identifying populations at risk from mercury exposure. Issued by UNEP DTIE Chemicals Branch and WHO Department of Food Safety, Zoonoses and Foodborne Diseases. . Geneva, Switzerland: United Nations Environment Programme / World Health Organization: https://www.who.int/foodsafety/publications/risk-mercury-exposure/en/; 2008.
Martin S, Griswold W. Human health effects of heavy metals. Environmental Science and Technology briefs for citizens. 2009;15:1–6.
Morton J, Mason HJ, Ritchie KA, White M. Comparison of hair, nails and urine for biological monitoring of low level inorganic mercury exposure in dental workers. Biomarkers. 2004;9(1):47–55.
Karahalil B, Rahravi H, Ertas N. Examination of urinary mercury levels in dentists in Turkey. Hum. Exp. Toxicol. 2005;24(8):383–8.
Herber RF, de Gee AJ, Wibowo AA. Exposure of dentists and assistants to mercury: mercury levels in urine and hair related to conditions of practice. Community Dent Oral Epidemiol. 1988;16(3):153–8.
Chaari N, Chebel S, Merchaoui I, Kerkeni A, Neffati F, Najjar F, et al. Neuropsychological effects of mercury exposure among dentists in Monastir City. Recent Patents Inflamm Allergy Drug Discov. 2015;9(2):151–8 Epub 2015/11/20. eng.
Chaari N, Kerkeni A, Saadeddine S, Neffati F, Khalfallah T, Akrout M. Mercury impregnation in dentists and dental assistants in Monastir city, Tunisia. Rev Stomatol Chir Maxillofac. 2009;110(3):139–44.
Echeverria D, Woods JS, Heyer NJ, Rohlman DS, Farin FM, Bittner AC, et al. Chronic low-level mercury exposure, BDNF polymorphism, and associations with cognitive and motor function. Neurotoxicol. Teratol. 2005;27(6):781–96.
Padilla Millán MA, Granados Correa F. Determination of mercury in urine of Mexican dentists. J. Radioanal. Nucl. Chem. 2002;254(2):305–9.
Wang Y, Goodrich JM, Werner R, Gillespie B, Basu N, Franzblau A. An investigation of modifying effects of single nucleotide polymorphisms in metabolism-related genes on the relationship between peripheral nerve function and mercury levels in urine and hair. Sci. Total Environ. 2012;417–418:32–8.
Ritchie KA, Burke FJ, Gilmour WH, Macdonald EB, Dale IM, Hamilton RM, et al. Mercury vapour levels in dental practices and body mercury levels of dentists and controls. Br Dent J. 2004;197(10):625–32.
Chopp GF, Kaufman EG. Mercury vapor related to manipulation of amalgam and to floor surface. Oper. Dent. 1983;8(1):23–7.
Powell L, Johnson G, Yashar Y, Bales D. Mercury vapor release during insertion and removal of dental amalgam. Oper. Dent. 1994;19:70.
Harris D, Nicols JJ, Stark R, Hill K. The dental working environment and the risk of mercury exposure. J. Am. Dent. Assoc. 1978;97(5):811–5.
Nilsson B, Nilsson B. Mercury in dental practice. II. Urinary mercury excretion in dental personnel. Swed Dent J. 1986;10(6):221–32.
Nixon G, Whittle C, Woodfin A. Mercury levels in dental surgeries and dental personnel. Br Dent J. 1981;151(5):149–54.
Harakeh S, Sabra N, Kassak K, Doughan B. Factors influencing total mercury levels among Lebanese dentists. Sci. Total Environ. 2002;297(1):153–60.
Harakeh S, Sabra N, Kassak K, Doughan B, Sukhn C. Mercury and arsenic levels among Lebanese dentists: a call for action. Bull Environ Contam Toxicol. 2003 April 01;70(4):0629–35.
Wijesekara LA, Usoof R, Gamage SST, Jayasinghe R, Gamage N, De Silva D, et al. Mercury levels in hair samples of dentists: a comparative study in Sri Lanka. J Investig Clin Dent. 2018;9(2):e12302.
Wranova K, Cejchanova M, Spevakova V, Korunova V, Vobecky M, Spevacek V. Mercury and methylmercury in hair of selected groups of Czech population. Cent Eur J Public Health. 2009;17(1):36–40.
Rodushkin I, Axelsson MD. Application of double focusing sector field ICP-MS for multielemental characterization of human hair and nails Part II A study of the inhabitants of northern Sweden. Sci. Total Environ. 2000;262(1):21–36.
Wilhelm M, Müller F, Idel H. Biological monitoring of mercury vapour exposure by scalp hair analysis in comparison to blood and urine. Toxicol Lett. 1996;88(1):221–6.
Al-Saleh I, Al-Doush I. Mercury content in skin-lightening creams and potential hazards to the health of Saudi women. J Toxicol Environ Health. 1997;51(2):123–30.
Acknowledgements
The authors want to thank authorities of Iran University of Medical Sciences for their comprehensives support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this article declare that they have no conflict of interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jonidi Jafari, A., Esrafili, A., Moradi, Y. et al. Mercury level in biological samples of dentists in Iran: a systematic review and meta-analysis. J Environ Health Sci Engineer 18, 1655–1669 (2020). https://doi.org/10.1007/s40201-020-00558-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40201-020-00558-w