Abstract
Purpose
The involvement of the intestinally expressed xenobiotic transporters P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP) have been implicated in apixaban disposition based on in vitro studies. Recommendations against co-administration of apixaban with inhibitors of these efflux transporters can be found throughout the literature as well as in the apixaban FDA label. However, the clinical relevance of such findings is questionable due to the high permeability and high solubility characteristics of apixaban.
Methods
Using recently published methodologies to discern metabolic- from transporter- mediated drug-drug interactions, a critical evaluation of all published apixaban drug-drug interaction studies was conducted to investigate the purported clinical significance of efflux transporters in apixaban disposition.
Results
Rational examination of these clinical studies using basic pharmacokinetic theory does not support the clinical significance of intestinal efflux transporters in apixaban disposition. Further, there is little evidence that efflux transporters are clinically significant determinants of systemic clearance.
Conclusions
Inhibition or induction of intestinal CYP3A4 can account for exposure changes of apixaban in all clinically significant drug-drug interactions, and lack of intestinal CYP3A4 inhibition can explain all studies with no exposure changes, regardless of the potential for these perpetrators to inhibit intestinal or systemic efflux transporters.

Similar content being viewed by others
Abbreviations
- AUC :
-
Area under the concentration-time curve
- AUMC :
-
Area under the moment-time curve
- BCRP:
-
Breast Cancer Resistance Protein
- BDDCS:
-
Biopharmaceutics Drug Disposition Classification System
- CL :
-
Clearance
- CL/F :
-
Apparent clearance
- C max :
-
Maximum concentration in systemic circulation
- C max,u :
-
Maximum unbound concentration in systemic circulation
- CYP:
-
Cytochrome P450
- DDI:
-
Drug-drug interaction
- F :
-
Bioavailability
- FDA:
-
Food and Drug Administration
- f u,plasma :
-
Fraction unbound in plasma
- IC 50 :
-
Half maximal inhibitory concentration
- I gut :
-
Maximum perpetrator concentration in the gut
- IV:
-
Intravenous
- k a :
-
Absorption rate constant
- MAT :
-
Mean absorption time
- MRT :
-
Mean residence time
- P-gp:
-
P-glycoprotein
- t max :
-
Time to maximum concentration
- t 1/2,z :
-
Terminal half-life
- V ss :
-
Volume of distribution at steady-state
- Vss/F:
-
Apparent volume of distribution at steady-state
References
ELIQUIS. (apixaban) [package insert]. Princeton: Bristol-Myers Squibb Company; 2012.
Jacqueroux E, Mercier C, Margelidon-Cozzolino V, Hodin S, Bertoletti L, Delavenne X. In vitro assessment of P-gp and BCRP transporter-mediated drug-drug interactions of riociguat with direct oral anticoagulants. Fundam Clin Pharmacol. 2020;34(1):109–19.
Zhang D, He K, Herbst JJ, Kolb J, Shou W, Wang L, et al. Characterization of efflux transporters involved in distribution and disposition of apixaban. Drug Metab Dispos. 2013;41(4):827–35.
Wu C-Y, Benet LZ. Predicting drug disposition via application of BCS: transport / absorption / elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm Res. 2005;22(1):11–23.
Benet LZ, Bowman CM, Koleske ML, Rinaldi CL, Sodhi JK. Understanding drug-drug interaction and pharmacogenomic changes in pharmacokinetics for metabolized drugs. J Pharmacokinet Pharmacodyn. 2019;46(2):155–63.
Sodhi JK, Huang CH, Benet LZ. Volume of distribution is unaffected by metabolic drug-drug interactions. Clin Pharmacokinet. [E-pub ahead of print, July 28, 2020].
Benet LZ, Bowman CM, Sodhi JK. How transporters have changed basic pharmacokinetic understanding. AAPS J. 2019;21(6):103.
Grover A, Benet LZ. Effects of drug transporters on volume of distribution. AAPS J. 2009;11(2):250–61.
Benet LZ, Galeazzi RL. Noncompartmental determinations of the steady-state volume of distribution. J Pharm Sci. 1979;68(8):1071–4.
U.S. Food and Drug Administration, Center for Drug Evaluation and Research. In vitro drug interaction studies – cytochrome P450 enzyme- and transporter- mediated drug interactions guidance for industry. Silver Spring, MD; 2020.
Tornio A, Filppula AM, Niemi M, Backman JT. Clinical studies on drug-drug interactions involving metabolism and transport: methodology, pitfalls and interpretation. Clin Pharmacol Ther. 2019;105(6):1345–61.
Benet LZ, Bowman CM, Liu S, Sodhi JK. The extended clearance concept following oral and intravenous dosing: theory and critical analyses. Pharm Res. 2018;35(12):242.
Cheong J, Halladay JS, Plise E, Sodhi JK, Salphati L. The effects of drug metabolizing enzymes inhibitors on hepatic efflux and uptake transporters. Drug Metab Lett. 2017;11(2):111–8.
Kimoto E, Mathialagan S, Tylaska L, Niosi M, Lin J, Carlo AA, et al. Organic anion transporter 2-mediated hepatic uptake contributes to the clearance of high-permeability-low-molecular-weight acid and zwitterion drugs: evaluation using 25 drugs. J Pharmacol Exp Ther. 2018;367(2):322–34.
Sato T, Mishima E, Mano N, Abe T, Yamaguchi H. Potential drug interactions mediated by renal organic anion transporter OATP4C1. J Pharmacol Exp Ther. 2017;362(2):271–7.
Zamek-Gliszczynski MJ, Taub ME, Chothe PP, Chu X, Giacomini KM, Kim RB, et al. International transporter consortium. Transporters in drug development: 2018 ITC recommendations for transporters of emerging clinical importance. Clin Pharmacol Ther. 2018;104(5):890–9.
Alluri RV, Li R, Varma MVS. Transporter-enzyme interplay and the hepatic drug clearance: what have we learned so far? Expert Opin Drug Metab Toxicol. 2020;16(5):387–401.
Varma MV, El-Kattan AF. Transporter-enzyme interplay: deconvoluting effects of hepatic transporters and enzymes on drug disposition using static and dynamic mechanistic models. J Clin Pharmacol. 2016;56:S99–S109.
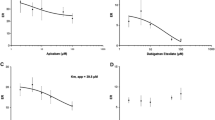
Sodhi JK, Benet LZ. A simple methodology to differentiate changes in bioavailability from changes in clearance following oral dosing of metabolized drugs. Clin Pharmacol Ther. 2020;108(2):306–15.
Sodhi JK, Benet LZ. The necessity of using changes in absorption time to implicate intestinal transporter involvement in oral drug-drug interactions. AAPS J. 2020;22:111.
Lau YY, Huang Y, Frassetto L, Benet LZ. Effect of OATP1B1 transporter inhibition on the pharmacokinetics of atorvastatin in healthy volunteers. Clin Pharmacol Ther. 2007;81(2):194–204.
Frost C, Song Y, Yu Z, Wang J, Lee LS, Schuster A, et al. The effect of apixaban on the pharmacokinetics of digoxin and atenolol in healthy subjects. Clin Pharmacol. 2017;9:19–28.
Bashir B, Stickle DF, Chervoneva I, Kraft WK. Drug-drug interaction study of apixaban with cyclosporine and tacrolimus in healthy volunteers. Clin Transl Sci. 2018;11(6):590–6.
Frost CE, Byon W, Song Y, Wang J, Schuster AE, Boyd RA, et al. Effect of ketoconazole and diltiazem on the pharmacokinetics of apixaban, an oral direct factor Xa inhibitor. Br J Clin Pharmacol. 2015;79(5):838–46.
Barrett YC, Wang J, Song Y, Pursley J, Wastall P, Wright R, et al. A randomized assessment of the pharmacokinetic, pharmacodynamic and safety interaction between apixaban and enoxaparin in healthy subjects. Thromb Haemost. 2012;107(5):916–24.
Upreti VV, Song Y, Wang J, Byon W, Boyd RA, Pursley JM, et al. Effect of famotidine on the pharmacokinetics of apixaban, an oral direct factor Xa inhibitor. Clin Pharmacol. 2013;5:59–66.
Mikus G, Foerster KI, Schaumaeker M, Lehmann M-L, Burhenne J, Haefeli WE. Microdosed cocktail of three oral factor Xa inhibitors to evaluate drug-drug interactions with potential perpetrator drugs. Clin Pharmacokinet. 2019;58(9):1155–63.
Frost C, Shenker A, Gandhi MD, Pursley J, Barrett YC, Wang J, et al. Evaluation of the effect of naproxen on the pharmacokinetics and pharmacodynamics of apixaban. Br J Clin Pharmacol. 2014;78(4):877–85.
Vakkalagadda B, Frost C, Byon W, Boyd RA, Wang J, Zhang D, et al. Effect of rifampin on the pharmacokinetics of apixaban, an oral direct inhibitor of factor Xa. Am J Cardiovasc Drugs. 2016;16(2):119–27.
Wang X, Mondal S, Wang J, Tirucherai G, Zhang D, Boyd RA, et al. Effect of activated charcoal on apixaban pharmacokinetics in healthy subjects. Am J Cardiovasc Drugs. 2014;14(2):147–54.
Kryukov AV, Sychev DA, Andreev DA, Ryzhikova KA, Grishina EA, Ryabova AV, et al. Influence of ABCB1 and CYP3A5 gene polymorphisms on pharmacokinetics of apixaban in patients with atrial fibrillation and acute stroke. Pharmgenomics Pers Med. 2018;11:43–9.
Ueshima S, Hira D, Fujii R, Kimura Y, Tomitsuka C, Yamane T, et al. Impact of ABCB1, ABCG2 and CYP3A5 polymorphisms on plasma trough concentrations of apixaban in Japanese patients with atrial fibrillation. Pharmacogenet Genomics. 2017;27(9):329–36.
Lombardo F, Berellini G, Obach RS. Trend analysis of a database of intravenous pharmacokinetic parameters in humans for 1352 drug compounds. Drug Metab Dispos. 2018;46(11):1466–77.
Maréchal J-D, Yu J, Brown S, Kapelioukh I, Rankin EM, Wolf CR, et al. In silico and in vitro screening for inhibition of cytochrome P450 CYP3A4 by comedications commonly used by patients with cancer. Drug Metab Dispos. 2006;34(4):534–8.
Hulskotte E, Gupta S, Xuan F, van Zutven M, O’Mara E, Feng H-P, et al. Pharmacokinetic interaction between the hepatitis C virus protease inhibitor boceprevir and cyclosporine and tacrolimus in healthy volunteers. Hepatology. 2012;56(5):1622–30.
Donato MT, Jiménez N, Castell JV, Gómez-Lechón MJ. Fluorescence-based assays for screening nine cytochrome P450 (P450) activities in intact cells expressing individual human P450 enzymes. Drug Metab Dispos. 2004;32(7):699–706.
Rautio J, Humphreys JE, Webster LO, Balakrishnan A, Keogh JP, Kunta JR, et al. In vitro p-glycoprotein inhibition assays for assessment of clinical drug interaction potential of new drug candidates: a recommendation for probe substrates. Drug Metab Dispos. 2006;34(5):786–92.
Miyata H, Takada T, Toyoda Y, Matsuo H, Ichida K, Suzuki H. Identification of febuxostat as a new strong ABCG2 inhibitor: potential applications and risks in clinical situations. Front Pharmacol. 2016;7:518.
Patel CG, Li L, Girgis S, Kornhauser DM, Frevert EU, Boulton DW. Two-way pharmacokinetic interaction studies between saxagliptin and cytochrome P450 substrates or inhibitors: simvastatin, diltiazem extended-release, and ketoconazole. Clin Pharmacol. 2011;3:13–25.
Burt HJ, Galetin A, Houston JB. IC50-based approaches as an alternative method for assessment of time-dependent inhibition of CYP3A4. Xenobiotica. 2010;40(5):331–43.
Ma B, Preuksaritanont T, Lin JH. Drug interactions with calcium channel blockers: possible involvement of metabolite-intermediate complexation with CYP3A. Drug Metab Dispos. 2000;28(2):125–30.
Wang J-S, Wen X, Backman JT, Taavitsainen P, Neuvonen PJ, Kivistö KT. Midazolam alpha-hydroxylation by human liver microsomes in vitro: inhibition by calcium channel blockers, itraconazole, and ketoconazole. Pharmacol Toxicol. 1999;85(4):157–61.
Ellens H, Deng S, Coleman J, Bentz J, Taub ME, Ragueneau-Majlessi I, Chung SP, Herédi-Szabó K, Neuhoff S, Palm J, Balimane P, Zhang L, Jamei M, Hanna I, O’Connor M, Bednarczyk D, Forsgard M, Chu X, Funk C, Guo A, Hillgren KM, Li L, Pak AY, Perloff ES, Rajaraman G, Salphati L, Taur J-S, Weitz D, Wortelboer HM, Xia CQ, Xiao G, Yamagata T, Lee CA. Application of receiver operating characteristic analysis to refine the prediction of potential digoxin drug interactions. Drug Metab Dispos. 2013;41(7):1367–74.
Zhang Y, Gupta A, Wang H, Zhou L, Vethanayagam RR, Unadkat JD, et al. BCRP transports dipyridamole and is inhibited by calcium channel blockers. Pharm Res. 2005;22(12):2023–34.
Isoherranen N, Lutz JD, Chung SP, Hachad H, Levy RH, Ragueneau-Majlessi I. Importance of multi-P450 inhibition in drug-drug interactions: evidence of incidence, inhibition magnitude, and prediction from in vitro data. Chem Res Toxicol. 2012;25(11):2285–300.
Frydman AM, Bara L, Le Roux Y, Woler M, Chauliac F, Samama MM. The antithrombotic activity and pharmacokinetics of enoxaparine, a low molecular weight heparin in humans given single subcutaneous doses of 20 to 80 mg. J Clin Pharmacol. 1988;28(7):609–18.
Lin JH, Chremos AN, Kanovsky SM, Schwartz S, Yeh KC, Kann J. Effects of antacids and food on absorption of famotidine. Br J Clin Pharmacol. 1987;24(4):551–3.
Moody DE, Liu F, Fang WB. In vitro inhibition of methadone and oxycodone cytochrome P450-dependent metabolism: reversible inhibition by H2-receptor agonists and proton-pump inhibitors. J Anal Toxicol. 2013;37(8):476–85.
Brown HS, Galetin A, Hallifax D, Houston JB. Prediction of in vivo drug-drug interactions from in vitro data: factors affecting prototypic drug-drug interactions involving CYP2C9, CYP2D6 and CYP3A4. Clin Pharmacokinet. 2006;45(10):1035–50.
Badri PS, Dutta S, Wang H, Podsadecki TJ, Polepally AR, Khatri A, et al. Drug interactions with the direct-acting antiviral combination of ombitasvir and paritaprevir-ritonavir. Antimicrob Agents Chemother. 2015;60(1):105–14.
Vermeer LMM, Isringhausen CD, Ogilvie BW, Buckley DB. Evaluation of ketoconazole and its alternative clinical CYP3A4/5 inhibitors as inhibitors of drug transporters: the in vitro effects of ketoconazole, ritonavir, clarithromycin, and itraconazole on 13 clinically relevant drug transporters. Drug Metab Dispos. 2016;44(3):453–9.
Kajbaf M, Longhi R, Montanari D, Vinco F, Rigo M, Fontana S, et al. A comparative study of the CYP450 inhibition potential of marketed drugs using two fluorescence based assay platforms routinely used in the pharmaceutical industry. Drug Metab Lett. 2011;5(1):30–9.
Saito H, Hirano H, Nakagawa H, Fukami T, Oosumi K, Murakami K, et al. A new strategy of high-speed screening and quantitative structure activity relationship analysis to evaluate human ATP-binding cassette transporter ABCG2-drug interactions. J Pharmacol Exp Ther. 2006;317(3):1114–24.
Polk RE, Brophy DF, Israel DS, Patron R, Sadler BM, Chittick GE, et al. Pharmacokinetic interaction between amprenavir and rifabutin or rifampin in healthy males. Antimicrob Agents Chemother. 2001;45(2):502–8.
Niemi M, Backman JT, Fromm MF, Neuvonen PJ, Kivistö KT. Pharmacokinetic interactions with rifampicin. Clin Pharmacokinet. 2003;42(9):819–50.
Lemmen J, Tozakidis IEP, Galla H-J. Pregnane X receptor upregulates ABC-transporter Abcg2 and Abcb1 at the blood-brain barrier. Brain Res. 2013;1491:1–13.
Goreczyca L, Aleksunes LM. Transcription factor-mediated regulation of the BCRP/ABCG2 efflux transporter: a review across tissues and species. Expert Opin Drug Metab Toxicol. 2020;16(3):239–53.
Bekersky I, Dressler D, Colburn W, Mekki Q. Bioequivalaence of 1 and 5 mg tacrolimus capsules using a replicate study design. J Clin Pharmacol. 1999;39:1032–7.
Amundsen R, Åsberg A, Ohm IK, Christensen H. Cyclosporine A- and tacrolimus-mediated inhibition of CYP3A4 and CYP3A5 in vitro. Drug Metab Dispos. 2012;40(4):655–61.
Kishimoto W, Ishiguro N, Ludwig-Schwellinger E, Ebner T, Schaefer O. In vitro predictability of drug-drug interaction likelihood of p-glycoprotein-mediated efflux of dabigatran etexilate based on [I]2/IC50 threshold. Drug Metab Dispos. 2014;42(2):257–63.
Patil AG, D’Souza R, Dixit N, Damre A. Validation of quinidine as a probe substrate for the in vitro P-gp inhibition assay in Caco-2 cell monolayer. Eur J Drug Metab Pharmacokinet. 2011;36(3):115–9.
Gupta A, Dai Y, Vethanayagam RR, Hebert MF, Thummel KE, Unadkat JD, et al. Cyclosporine A, tacrolimus and sirolimus are potent inhibitors of the human breast cancer resistance protein (ABCG2) and reverse resistance to mitoxantrone and topotecan. Cancer Chemother Pharmacol. 2006;58(3):374–83.
Frost C, Nepal S, Wang J, Schuster A, Byon W, Boyd RA, et al. Safety, pharmacokinetics and pharmacodynamics of multiple oral doses of apixaban, a factor Xa inhibitor, in healthy subjects. Br J Clin Pharmacol. 2013;76(5):776–86.
Yavorski RT, Hallgren SE, Blue PW. Effects of verapamil and diltiazem on gastric emptying in normal subjects. Dig Dis Sci. 1991;36(9):1274–6.
Raghavan N, Frost CE, Yu Z, He K, Zhang H, Humphreys WG, et al. Apixaban metabolism and pharmacokinetics after oral administration to humans. Drug Metab Dispos. 2009;37(1):74–81.
Byon W, Garonzik S, Boyd RA, Frost CE. Apixaban: a clinical pharmacokinetic and pharmacodynamic review. Clin Pharmacokinet. 2019;58(10):1265–79.
Prom R, Spinler SA. The role of apixaban for venous and arterial thromboembolic disease. Ann Pharmacother. 2011;45(10):1262–83.
Budovich A, Zargarova O, Nogid A. Role of apixaban (eliquis) in the treatment and prevention of thromboembolic disease. Pharm Ther. 2013;38(4):206–31.
Gong IY, Kim RB. Important of pharmacokinetic profile and variability as determinants of dose and response to dabigatran, rivaroxaban, and apixaban. Can J Cardiol. 2013;29:S24–33.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sodhi, J.K., Liu, S. & Benet, L.Z. Intestinal Efflux Transporters P-gp and BCRP Are Not Clinically Relevant in Apixaban Disposition. Pharm Res 37, 208 (2020). https://doi.org/10.1007/s11095-020-02927-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-02927-4