Abstract
Background
Invasive fungal infection is a major source of morbidity and mortality. The usage of microbial cell-free DNA for the detection and identification of invasive fungal infection has been considered as a potential alternative to invasive procedures allowing for rapid results.
Objective
This analysis aimed to assess the budget implications of using the Karius® Test in patients suspected of invasive fungal infection in an average state in the USA from a healthcare payer perspective.
Methods
The analysis used a decision tree to capture key stages of the patient pathway, from suspected invasive fungal infection to either receiving treatment for invasive fungal infection or being confirmed as having no invasive fungal infection. The analysis used published costs and resource use from a targeted review of the literature. Because of the paucity of published evidence on the reduction of diagnostic tests displaced by the Karius Test, the analysis used a 50% reduction in the use of bronchoscopy and/or bronchoalveolar lavage. The impact of this reduction was tested in a scenario analysis.
Results
The results of the analysis show that the introduction of the Karius Test is associated with a cost saving of US$2277 per patient; when multiplied by the estimated number of cases per year, the cost saving is US$17,039,666. The scenario analysis showed that the Karius Test only had an incremental cost of US$87 per patient when there was no reduction in bronchoscopy and bronchoalveolar lavage.
Conclusions
The Karius Test may offer a valuable and timely option for the diagnosis of invasive fungal infection through its non-invasive approach and subsequent cost savings.
Similar content being viewed by others
Usage of microbial cell-free DNA via the Karius® Test is a non-invasive means for the detection and identification of invasive fungal infections. |
Cost savings were estimated through reduced expenditures related to bronchoscopy/bronchoalveolar lavage, adverse events, and a shorter hospitalization. |
1 Introduction
Invasive fungal infection (IFI) is a major source of morbidity and mortality, with a rising prevalence owing, in part, to the increased use of aggressive chemotherapy and immunosuppressive treatments [1, 2]. Whilst there is continued research in IFI, the current diagnostic ‘gold standard’ of IFI remains culture of fluid or tissue obtained by bronchoalveolar lavage and/or biopsy [1, 3]. The Karius® Test offers a non-invasive approach to provide species-level identification of IFI as well as other bacterial, DNA viral, fungal, and parasitic organisms. The Karius Test uses proprietary molecular biology and next-generation sequencing to detect trace amounts of microbial DNA from a single blood sample while using data analytics to identify pathogens, with results typically available within 1 business day from sample receipt.
Usage of the Karius Test for the detection and identification of invasive fungal infections has been considered as a potential alternative to invasive procedures allowing for rapid results [4, 5]. Invasive procedures may be associated with added costs and adverse events. Additionally, careful consideration of infection control risks associated with certain procedures that may be aerosol generating, such as bronchoscopy, supports the evaluation of non-invasive means for diagnosing infections. As noted in the Centers for Disease Control and Prevention guidance for individuals with suspected or confirmed Coronavirus Disease 2019 (SARS-CoV-2 or COVID-19), aerosol generating procedures “should be performed cautiously and avoided if possible” [6].
Budget impact analysis is an essential part of a comprehensive economic assessment of a healthcare technology and is increasingly required before formulary approval or reimbursement. The purpose of a budget impact model (BIM) is to estimate the financial consequences of adoption and uptake of a new healthcare intervention within a specific healthcare setting or across a specific population given inevitable resource constraints [7]. The aim of this project was to develop a BIM to assess the impact of incorporating the Karius Test as part of the diagnostic pathway for patients suspected of IFI vs standard of care (SoC).
2 Methods
2.1 Model Design
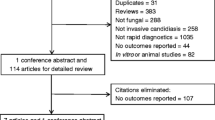
The budget impact of the Karius Test was assessed by a decision-tree BIM for patients suspected of IFI. To inform the conceptualization of the BIM, a review of existing health economic models was conducted. The review of literature identified 19 studies, consisting of 13 decision-tree models and six hybrid model structures [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26].
Based on the clinical pathway, existing economic models, and understanding of where the Karius Test would fit into the diagnostic pathway, a decision-tree structure was used as shown in Fig. 1. The decision tree is used for both the case with the Karius Test and without the Karius Test. The model considers four key points of the treatment pathway: (1) the decision to place patients on diagnostic-driven therapy for IFI or not; (2) the diagnostic test and its associated morbidity; (3) the outcomes of the diagnostic test, specifically three possible outcomes (proven IFI, probable IFI, and possible IFI); and (4) the implications of the diagnostic test (does this lead to treatment, additional testing, or no treatment). Within Fig. 1, the Karius Test is a diagnostic test that may be available within the “order diagnostic tests” box. Other or additional diagnostic tests that may be considered at the same timepoint or later in the flow of Fig. 1, are shown in Table 2.
The BIM was developed using Microsoft Excel® 2010 to calculate the financial impact of using the Karius Test compared with SoC. The model focused on the diagnosis and treatment of patients with IFI in hospital. To estimate the total costs in the reference and anticipated scenario, the total number of patients receiving each treatment was estimated using the total patient population per state, incidence of suspected IFI, and prevalence of patients who are immunocompromised over a year. The definition of immunocompromised within the model included a healthcare professional assessment, recently prescribed medication and/or evidence of cancer, as aligned with the definition used within a cross-sectional analysis [27].
The model used definitions of IFI in line with the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium definitions [28, 29]. As compared to its previous iteration, the recently published guidelines further consider tests for detecting fungal nucleic acid in the determination of probable invasive pulmonary mold diseases and other invasive diseases.
2.2 Model Perspective, Time Horizon
The BIM was constructed from a US healthcare payer perspective for the purposes of this article though the model can be adjusted to address a discrete hospital or health-system population. The duration of the diagnostic tests and duration of IFI treatment are expected to be less than 1 year; therefore, a 1-year time horizon was utilized. The cost per patient was based on the time to diagnosis and the duration of IFI treatment. The model considered how many patients would be included in the model over a 1-year time frame.
2.3 Patient Population
The patient population considered in the model are patients who present to hospital who are immunocompromised with a fever. To estimate the number of patients eligible for the model, a top-down approach based on published values was used as shown in Table 1. Based on the published estimates shown in Table 1, the number of patients undergoing diagnostic testing would be 7484. Results from the analysis will be presented per population and per patient.
The proportion of patients who are immunocompromised was taken from a review of the literature and was deemed as the most appropriate data source. However, to tackle uncertainty, results per patient will be reported. As there were limited data, it was not possible to draw major differences between private healthcare and Medicare/Medicaid; therefore, no split was applied to the patients undergoing diagnostic testing. Similarly, uninsured patients were not removed from the analysis; however, the results per patient could be used to scale the results to a specific population of interest.
2.4 Clinical Inputs
Empiric therapy is defined within the model as therapy assigned prior to or without diagnostic test results. The use of empiric therapy was reported as 30% of patients by Mao et al. [33] utilizing data from Europe and felt to be in line with expert opinion in the USA; this has been used to separate patients receiving empiric and diagnostic-driven therapy in the reference scenario. For the scenario with the Karius Test, it is assumed all patients receive diagnostic test-guided therapy. While the diagram shows the diagnostic tests (including the Karius Test) to be downstream of the decision for empiric and diagnostic test-guided therapy, in reality the decision regarding therapy and diagnostic tests would be taken in quick succession. Additionally, the decision for initial therapy may be impacted by the turnaround time of the diagnostic tests available.
After the initial decision regarding the use of empiric therapy, the diagnostic tests are ordered. The diagnostic tests incorporated into the model are based on the published estimates by Barnes et al. and Rossoff et al. as shown in Table 2 [4, 34]. The same diagnostic tests were used for both the SoC arm and the Karius Test arm, with the exception of a reduction in bronchoscopy and bronchoalveolar lavage.
The base-case settings for the model assume there would be a 50% reduction in bronchoscopy or bronchoalveolar lavage in the Karius Test arm. However, a range of values have been tested in scenario analyses and the reduction in bronchoscopy or bronchoalveolar lavage can be greater depending on regional practice patterns.
The model has the functionality to permit for the outcomes of the diagnostic tests to vary depending on usage of the Karius Test vs SoC. However, currently, because of limited published data, the outcomes of the diagnostic tests were assumed to be the same. The results of the diagnostic tests are based on published trial data [35] (1.1% proven, 6.6% probable, 19.0% possible, and 73.3% no IFI) and the model assumes no difference in results between the two arms of the BIM.
The model allows additional tests to be undertaken and these are programmed in the model as the proportion of patients in each health state (definite, probable, possible IFI). The model assumed 50% of patients in the probable IFI or possible IFI would receive further testing, which is shown in the diagram as the diagnostic tests following on from the probable and possible IFI states. Patients who are probable or possible will receive treatment if they do not receive additional testing.
Adverse events are captured in the model in two parts: first, those adverse events associated with the diagnostic tests and, second, those adverse events associated with the empiric treatment. The adverse event rates were identified by a targeted review of the literature. Those adverse events of grade 3 or 4 severity that impacted more than 5% of patients were considered in the model. The adverse events associated with the treatments are shown in Table 3 and the adverse events associated with the diagnostic tests are shown in Table 4.
2.5 Cost and Resource Inputs
Drug acquisition costs including average wholesale price were taken from the Redbook 2018. Wholesale acquisition cost was tested within the model. Dosing is based on product information for the individual treatments. The drug acquisition cost is incurred by the patients who receive empiric therapy and those who require IFI treatment. The cost of the Karius Test is US$2000 [41]. The cost per administration of IFI treatment is incorporated into the model for the treatments, with an administration cost of US$74.16 [36]. The model assumes that oral IFI treatments do not require an administration cost.
Resource use (Table 2) and adverse events (Tables 3 and 4), which are associated with a cost, have been identified from the literature and are considered in the model [4, 34]. The cost year in the analysis was 2018–19 and costs were inflated where necessary.
To consider the cost of treatment upon confirmation of IFI, market share data from Fung et al. have been used to create an average cost per treatment of IFI [63]. The data from Fung et al. also provided data for empiric therapy and diagnostic-driven therapy. The cost per treatment and the market share are shown in the “Appendix”.
The model assumes SoC has a total length of stay of 24 days in hospital [64, 65]. Based on the faster time to results for the Karius Test and potentially an earlier consequent assignment of appropriate treatment compared with SoC [66], the Karius Test was assumed to reduce the relative length of stay by 20%. This parameter is base tested in the scenario analysis. An inpatient stay in hospital had a cost of US$1746.00 per day [67].
2.6 Model Output
The financial impact of use of the Karius Test on the healthcare budget is presented for the total estimated population per state and per patient. A breakdown of the total cost is presented showing how the total cost is based on different model aspects. The breakdown separates IFI treatment and the initial empiric therapy costs. The initial empiric therapy costs only cover the first 2 days until the diagnostic tests are returned and an informed decision is made [68, 69].
Two scenario analyses have been conducted to understand the sensitivity of the model output to two key parameters; the first being the reduction in hospital length of stay and the second being the reduction in bronchoscopy/bronchoalveolar lavage. The scenario analysis tested 0–100% to understand the full range of impact.
3 Results
3.1 Base-Case Results
The base-case results show usage of the Karius Test as cost saving compared with SoC. For the total population per state, a saving of US$17,039,666 (shown in Table 5) was achieved, which relates to -US$2277 per patient (shown in Table 5). The saving is based on a reduction in diagnostic costs, administration costs, adverse event costs, and IFI treatment costs. The saving related to hospitalization is captured within IFI treatment within the model, hence seen within the IFI treatment in the table below. The Karius test is expected to reduce hospitalization length of stay because of a quicker turnaround time and the assignment of directed treatment. The cost breakdown is shown in Table 6. As the BIM made no assumption regarding clinical outcomes, the outcomes were equal between the two treatment arms.
3.2 Scenario Analysis
Figure 2 shows that with a 0% reduction in hospitalization, the Karius Test is still associated with a cost saving of US$572 per patient. With a 10% reduction in hospitalization, the Karius Test is associated with a cost saving of $1486. Figure 3 shows how a reduction in bronchoscopy/bronchoalveolar lavage correlates with the budget impact. A 0% reduction in bronchoscopy/bronchoalveolar lavage results in a US$87 incremental cost per patient. The breakeven point for this analysis is 1.84%. A 10% reduction in bronchoscopy/bronchoalveolar lavage results in a cost saving of US$386.
An additional scenario analysis has been conducted to test the proportion of patients receiving empiric therapy, assuming the same use of empiric treatment in the Karius Test arm as used for the SoC arm. The results of this analysis showed the cost saving per patient to be US$2000, a reduction of US$277 per patient from the base case.
To understand the implications of using average wholesale price, a scenario analysis tested the use of wholesale acquisition cost. The results of this analysis showed the cost saving per patient to be US$2267, a reduction of US$10 from the base analysis.
4 Discussion
The Karius Test was shown to provide a non-invasive cost-saving alternative for the diagnosis of IFI compared with SoC. These cost savings were realized through a reduced expenditure related to bronchoscopy/bronchoalveolar lavage as well as a reduction in adverse events and a shorter hospitalization. When testing key uncertainty in the model in the scenario analysis, the results were shown to be robust, with only one result showing the Karius Test as increasing expenditure (when testing a 0% reduction in bronchoscopy/bronchoalveolar lavage the model showed an incremental cost of US$87 per patient). When testing the uncertainty around hospitalization, in all cases, the Karius Test was cost saving.
This analysis has the advantage of using a clear model structure to capture the diagnostic pathway aligned with existing economic models. During model conceptualization, we considered the use of sensitivity and specificity in the diagnostic tests. However, this approach was not possible given the limited data regarding the efficacy of many novel diagnostics in infectious diseases. Consequently, the model’s clinical and cost inputs were aligned with the published literature. To test the impact these informed assumptions had on the outcome of the model, they were included in the sensitivity analysis.
The conducted analysis encountered several challenges while populating the model. A key theme to these challenges was limited published data to populate the model. For example, the consistency of reporting of adverse events and the sample size of studies used for diagnostic tests meant assumptions were required to either conclude adverse events were not incurred or that adverse events that were reported were grade 3 or 4. Another example of the impact of limited published data includes the informed need to consider the cost of the adverse event of confusion as equivalent to the cost to migraine for the purposes of this analysis. An additional limitation of the current analysis is the total population considered within the analysis. Study values were based on a calculated number per state based on published estimates; however, there is potential for uncertainty in the key estimates as some published studies have a small sample size. This limitation was considered acceptable as the result per patient is reported and can be scaled up to find a total population result. Similarly, the proportion of patients presenting for fever was based on an older reference but was deemed the most applicable to this model as there is a lack of studies to our knowledge that offer a clearly different value. These data sources do not impact the per patient results. Similar limitations were seen within the inputs used for the disease pathway where limited data were available and expert opinion or data from other geographic populations were considered. Generalizability of the findings noted in the analysis may be a limitation in our current study, particularly in light of varied practice patterns within and outside of the USA. While it is debatable whether a one-way sensitivity analysis is required for a budget impact analysis, the key parameters that have uncertainty in the model have been tested in the scenario analysis. These parameters do not have confidence intervals or measures of uncertainty; therefore, a one-way sensitivity analysis would provide similar results to our findings.
This research is based on our approach to quantify the individual aspects of the patient pathway to understand the value of novel diagnostics. While reimbursement for healthcare services may be based on diagnosis-related groups in many countries, such reimbursement mechanisms are limited in allowing for the evaluation of the potential impact of individual aspects of diagnosis or care as such costs would be grouped together. Further study into this impact would be warranted.
The model conservatively assumed no difference in clinical outcomes in both the empiric and diagnostic-driven Karius Test arms. Further research would help inform how the use of the Karius Test would alter IFI treatment, in terms of both speed to diagnosis and selection of therapies as well as the number of cases identified. Research into how the Karius Test may translate into cost avoidance for other diagnostic methods in infectious diseases beyond IFI is also warranted. The potential additive diagnostic value of the Karius Test in simultaneously allowing for the identification of not just fungi but other bacteria, DNA viruses, and parasitic organisms that may not be captured by conventional diagnostics is also not fully appreciated in the current model. Finally, the model does not account for other potential costs associated with bronchoscopy/bronchoalveolar lavage more recently appreciated in the SARS-CoV-2 pandemic including the transmission of infectious disease via aerosolization and the need for personal protective equipment. In summary, the Karius Test may offer a valuable and timely option for the diagnosis of IFI through its non-invasive approach and subsequent cost savings.
5 Conclusions
The Karius Test may offer a valuable and timely option for the diagnosis of invasive fungal infection through its non-invasive approach and subsequent cost savings.
References
Donnelly JP, Chen SC, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciz1008.
Menzin J, Meyers JL, Friedman M, et al. Mortality, length of hospitalization, and costs associated with invasive fungal infections in high-risk patients. Am J Health Syst Pharm. 2009;66:1711–7.
Knox KS, Meinke L. Role of bronchoalveolar lavage diagnostics in fungal infections. Clin Chest Med. 2009;30:355–65.
Rossoff J, Locke M, Helenowski IB, Batra S, Katz BZ, Hijiya N. Cost analysis of bronchoalveolar lavage and respiratory tract biopsies in the diagnosis and management of suspected invasive fungal infection in children with cancer or who have undergone stem cell transplant. Pediatr Blood Cancer. 2019;66(5):e27598.
Steinbrink JM, Hong DK, Bergin SP, Al-Rohil RN, Perfect JR, Maziarz EK. The robust and rapid role of molecular testing in precision fungal diagnostics: a case report. Med Mycol Case Rep. 2020;27:77–80.
CDC. Interim infection prevention and control recommendations for patients with suspected or confirmed Coronavirus Disease 2019 (COVID-19) in healthcare settings. 2020. www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed 18 May 2020.
Mauskopf JA, Sullivan SD, Annemans L, et al. Principles of good practice for budget impact analysis: report of the ISPOR Task Force on good research practices: budget impact analysis. Value Health. 2007;10(5):336–47.
Al-Badriyeh D, Slavin M, Liew D, et al. Pharmacoeconomic evaluation of voriconazole versus posaconazole for antifungal prophylaxis in acute myeloid leukaemia. J Antimicrob Chemother. 2010;65(5):1052–61.
Ament AJ, Hubben MW, Verweij PE, et al. Economic evaluation of targeted treatments of invasive aspergillosis in adult haematopoietic stem cell transplant recipients in the Netherlands: a modelling approach. J Antimicrob Chemother. 2007;60(2):385–93.
de la Camara R, Jarque I, Sanz MA, et al. Economic evaluation of posaconazole vs fluconazole in the prevention of invasive fungal infections in patients with GVHD following haematopoietic SCT. Bone Marrow Transplant. 2010;45(5):925–32.
Dranitsaris G, Khoury H. Posaconazole versus fluconazole or itraconazole for prevention of invasive fungal infections in patients undergoing intensive cytotoxic therapy for acute myeloid leukemia or myelodysplasia: a cost effectiveness analysis. Support Care Cancer. 2011;19(11):1807–13.
Garbino J, Schnetzler G, Roberts C. Invasive aspergillosis: is treatment with "inexpensive" amphotericin B cost saving if "expensive" voriconazole is only used on demand? Swiss Med Wkly. 2006;136(39–40):624–30.
Grau S, de la Camara R, Sabater FJ, et al. Cost-effectiveness of posaconazole versus fluconazole or itraconazole in the prevention of invasive fungal infections among high-risk neutropenic patients in Spain. BMC Infect Dis. 2012;12:83.
Harrison D, Muskett H, Harvey S, et al. Development and validation of a risk model for identification of non-neutropenic, critically ill adult patients at high risk of invasive Candida infection: the Fungal Infection Risk Evaluation (FIRE) Study. Health Technol Assess. 2013;17(3):1–156.
Heng SC, Slavin MA, Al-Badriyeh D, et al. Pharmacoeconomic evaluation of fluconazole, posaconazole and voriconazole for antifungal prophylaxis in patients with acute myeloid leukaemia undergoing first consolidation chemotherapy. J Antimicrob Chemother. 2013;68(7):1669–788.
Jansen JP, Kern WV, Cornely OA, et al. Economic evaluation of voriconazole versus conventional amphotericin B in the treatment of invasive aspergillosis in Germany. Value Health. 2006;9(1):12–23.
Kimura SI, Murata T, Akahoshi Y, et al. Economic evaluation of a preemptive treatment strategy for invasive fungal infection in neutropenic patients with hematological diseases. Eur J Clin Microbiol Infect Dis. 2015;34(5):951–61.
Lundberg J, Hoglund M, Bjorkholm M, Akerborg O. Economic evaluation of posaconazole versus fluconazole or itraconazole in the prevention of invasive fungal infection in high-risk neutropenic patients in Sweden. Clin Drug Investig. 2014;34(7):483–9.
Mauskopf J, Chirila C, Graham J, et al. Comparative cost-effectiveness analysis of voriconazole and fluconazole for prevention of invasive fungal infection in patients receiving allogeneic hematopoietic cell transplants. Am J Health Syst Pharm. 2013;70(17):1518–27.
Neoh CF, Liew D, Slavin M, et al. Cost-effectiveness analysis of anidulafungin versus fluconazole for the treatment of invasive candidiasis. J Antimicrob Chemother. 2011;66(8):1906–15.
O'Sullivan AK, Pandya A, Papadopoulos G, et al. Cost-effectiveness of posaconazole versus fluconazole or itraconazole in the prevention of invasive fungal infections among neutropenic patients in the United States. Value Health. 2009;12(5):666–73.
Rotstein C, Laverdiere M, Marciniak A, Ali F. An economic evaluation of voriconazole versus amphotericin B for the treatment of invasive aspergillosis in Canada. Can J Infect Dis Med Microbiol. 2004;15(5):277–84.
Sadique Z, Grieve R, Harrison DA, et al. An integrated approach to evaluating alternative risk prediction strategies: a case study comparing alternative approaches for preventing invasive fungal disease. Value Health. 2013;16(8):1111–22.
Tahami Monfared AA, O'Sullivan AK, Rotstein C, Papadopoulos G. Economic evaluation of posaconazole versus standard azole therapy as prophylaxis against invasive fungal infections in patients with prolonged neutropenia in Canada. Can J Infect Dis Med Microbiol. 2012;23(2):59–64.
Turner SJ, Senol E, Kara A, Al-Badriyeh D, Dinleyici EC, Kong DC. Pharmacoeconomic evaluation of voriconazole vs. liposomal amphotericin B in empiric treatment of invasive fungal infections in Turkey. BMC Infect Dis. 2013;13:560.
Wenzel R, Del Favero A, Kibbler C, et al. Economic evaluation of voriconazole compared with conventional amphotericin B for the primary treatment of aspergillosis in immunocompromised patients. J Antimicrob Chemother. 2005;55(3):352–61.
Harpaz R, Dahl RM, Dooling KL. Prevalence of immunosuppression among US adults, 2013. JAMA. 2016;316(23):2547–8.
De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–21.
Donnelly JPCS, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 2019. https://doi.org/10.1093/cid/ciz1008.
Census.gov. QuickFacts: United States: population estimate July 2017. 2017. Available from: https://www.census.gov/quickfacts/fact/table/US/PST045217. Accessed 19 Feb 2019.
Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP). 2014. Available from: https://www.ahrq.gov/data/hcup/index.html. Accessed 19 Feb 2019.
Sternbach G, Varon J, Hunt S. Emergency department presentation and care of heart and heart/lung transplant recipients. Ann Emerg Med. 1992;21(9):1140–4.
Mao N, Lesher B, Liu Q, et al. Economic analysis of empiric versus diagnostic-driven strategies for immunocompromised patients with suspected fungal infections in the People's Republic of China. Clinicoecon Outcomes Res. 2016;8:275–85.
Barnes R, Earnshaw S, Herbrecht R, et al. Economic comparison of an empirical versus diagnostic-driven strategy for treating invasive fungal disease in immunocompromised patients. Clin Ther. 2015;37(6):1317–28.e2.
Sun Y, Meng F, Han M, et al. Epidemiology, management, and outcome of invasive fungal disease in patients undergoing hematopoietic stem cell transplantation in China: a multicenter prospective observational study. Biol Blood Marrow Transplant. 2015;21(6):1117–26.
Centers for Medicare & Medicaid services. Physician fee schedule. 2019. www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched. Accessed 17 November 2019.
Prasad P, Fishman JA. Impact and cost of the serum galactomannan assay at a tertiary care facility. Transplantation. 2014;98:773–80.
Silva B. RT-PCR usage expands as preferred method of infection detection. 2020. Available from: https://www.mlo-online.com/diagnostics/article/21125872/rtpcr-usage-expands-as-preferred-method-of-infection-detection. Accessed 10 Sept 2020.
Poslusny C. How much does a PET scan cost? 2019. Available from: https://www.newchoicehealth.com/pet-scan/cost. Accessed 10 Sept 2020.
Lokhandwala T, Dann R, Johnson M, D’Souza AO. Costs of the diagnostic workup for lung cancer. In: Medicare Claims Analysis Multidisiplinary Symposium in Thoracic Oncolocy; 30 October–1 November 2014; Chicago (IL).
Karius, Inc. Company communication. 11 May 2020.
Wong W, Yim YM, Kim A, et al. Assessment of costs associated with adverse events in patients with cancer. PLoS ONE. 2018;13(4):e0196007.
Elgilani F, Glorioso JM, Hathcock MA, Kremers WK, Nyberg SL. Economic impact of liver transplantation for acute liver failure. J Liver: Dis Transplant. 2016;5:1. https://doi.org/10.4172/2325-9612.1000132.
Carlton R, Lunacsek O, Regan T, Carroll C. Healthcare costs among patients with excessive sleepiness associated with obstructive sleep apnea, shift work disorder, or narcolepsy. Am Health Drug Benefits. 2014;7(6):334–40.
MDsave. MDsave: how much does an electrocardiogram (EKG/ECG) cost near me? 2019. Available from: https://www.mdsave.com/procedures/electrocardiogram-ekg-with-interpretation/d182ff. Accessed 10 Sept 2020.
Stokes M, Becker WJ, Lipton RB, et al. Cost of health care among patients with chronic and episodic migraine in Canada and the USA: results from the International Burden of Migraine Study (IBMS). Headache. 2011;51(7):1058–77.
Silver SA, Long J, Zheng Y, Chertow G. Cost of acute kidney injury in hospitalized patients. J Hosp Med. 2017;12(2):70–6.
Wingard JR, Carter SL, Walsh TJ, et al. Randomized, double-blind trial of fluconazole versus voriconazole for prevention of invasive fungal infection after allogeneic hematopoietic cell transplantation. Blood. 2010;116(24):5111–8.
EMA. Cancidas (previously caspofungin MSD). 2019. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/cancidas-previously-caspofungin-msd. Accessed 10 Sept 2020.
Walsh TJ, Finberg RW, Arndt C, et al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. N Engl J Med. 1999;340(10):764–71.
Saliba F, Pascher A, Cointault O, et al. Randomized trial of micafungin for the prevention of invasive fungal infection in high-risk liver transplant recipients. Clin Infect Dis. 2015;60(7):997–1006.
Raad II, Graybill JR, Bustamante A, Cornely OA, Gaona-Flores V, Afif C, et al. Safety of long-term oral posaconazole use in the treatment of refractory invasive fungal infections. Clin Infect Dis. 2006;42(1726):1726–34.
Sabol K, Gumbo T. Anidulafungin in the treatment of invasive fungal infections. Ther Clin Risk Manag. 2008;4(1):71–8.
Kim MH, Johnston SS, Chu BC, Dalal MR, Schulman KL. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4(3):313–20.
Welch BT, Brinjikji W, Schmit GD, et al. A national analysis of the complications, cost, and mortality of percutaneous lung ablation. J Vasc Interv Radiol. 2015;26(6):787–91.
Wilson L, Devine EB, So K. Direct medical costs of chronic obstructive pulmonary disease: chronic bronchitis and emphysema. Respir Med. 2000;94(3):204–13.
Oba Y, Zaza T. Abandoning daily routine chest radiography in the intensive care unit: meta-analysis. Radiology. 2010;255(2):386–95.
Kobayashi D, Takahashi O, Ueda T, et al. Risk factors for adverse reactions from contrast agents for computed tomography. BMC Med Inform Decis Mak. 2013;13:18.
Carr IM, Koegelenberg CFN, von Groote-Bidlingmaier F, et al. Blood loss during flexible bronchoscopy: a prospective observational study. Respiration. 2012;84(4):312–8.
Herth FJ, Becker HD, Ernst A. Aspirin does not increase bleeding complications after transbronchial biopsy. Chest. 2002;122(4):1461–4.
Elston WJ, Whittaker AJ, Khan LN, et al. Safety of research bronchoscopy, biopsy and bronchoalveolar lavage in asthma. Eur Respir J. 2004;24(3):375–7.
Hue SH. Complications in transbronchial lung biopsy. Korean J Intern Med. 1987;2(2):209–13.
Fung M, Kim J, Marty FM, Schwarzinger M, Koo S. Meta-analysis and cost comparison of empirical versus pre-emptive antifungal strategies in hematologic malignancy patients with high-risk febrile neutropenia. PLoS ONE. 2015;10(11):e0140930.
Zilberberg MD, Shorr AF, Huang H, Chaudhari P, Paly V, Menzin J. Hospital days, hospitalization costs, and inpatient mortality among patients with mucormycosis: a retrospective analysis of US hospital discharge data. BMC Infect Dis. 2014;14:310.
Muss HB, Case LD, Capizzi RL, et al. High- versus standard-dose megestrol acetate in women with advanced breast cancer: a phase III trial of the Piedmont Oncology Association. J Clin Oncol. 1990;8(11):1797–805.
Armstrong AE, Rossoff J, Hollemon D, Hong DK, Muller WJ, Chaudhury S. Cell-free DNA next-generation sequencing successfully detects infectious pathogens in pediatric oncology and hematopoietic stem cell transplant patients at risk for invasive fungal disease. Pediatr Blood Cancer. 2019;66(7):e27734.
MacVane SH, Tuttle LO, Nicolau DP. Impact of extended-spectrum β-lactamase-producing organisms on clinical and economic outcomes in patients with urinary tract infection. J Hosp Med. 2014;9(4):232–8.
Hahn-Ast C, Glasmacher A, Muckter S, et al. Overall survival and fungal infection-related mortality in patients with invasive fungal infection and neutropenia after myelosuppressive chemotherapy in a tertiary care centre from 1995 to 2006. J Antimicrob Chemother. 2010;65(4):761–8.
Ibanez-Martinez E, Ruiz-Gaitan A, Peman-Garcia J. Update on the diagnosis of invasive fungal infection. Rev Esp Quimioter. 2017;30(Suppl. 1):16–211.
Heresi GA, Platt DM, Wang W, et al. Healthcare burden of pulmonary hypertension owing to lung disease and/or hypoxia. BMC Pulm Med. 2017;17(1):58.
US FDA. Sporanoz (itraconazole) capsules. 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022484s000lbl.pdf. Accessed 19 Sept 2019.
US FDA. Vfend (voriconazole) i.v., tablets and suspension label. Reference ID: 2866932. 2010. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021266s032lbl.pdf. Accessed 19 Sept 2019.
US FDA. AmBisome (amphotericin B) liposome for injection. 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/050740s016lbl.pdf. Accessed 19 Sept 2019.
US FDA. Mycamine (micafungin sodium) for injection. 2007. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021506s011s012lbl.pdf. Accessed 19 Sept 2019.
US FDA. Noxafil (posaconazole). Reference ID: 3847805. 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022003s018s020,0205053s002s004,0205596s001s003lbl.pdf. Accessed 19 Sept 2019.
Acknowledgements
The authors thank Marc Watrous for assistance with the preparation of the manuscript. The model used in this study was provided to the journal’s peer reviewers for their reference when reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Karius, Inc. provided funding for the preparation of this article.
Conflict of interest
Ann T. MacIntyre, Radha Duttagupta, Desiree Hollemon, David K. Hong, and Timothy A. Blauwkamp are current or former employees of Karius, Inc. Alex Hirst is an employee of ICON plc.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data that support the findings of this article are available from the corresponding author on request.
Code availability
Not applicable.
Author contributions
ATM, AH, RD, DH, DKH, and TAB developed the theoretical framework, discussed results, and contributed equally to the final version of the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
MacIntyre, A.T., Hirst, A., Duttagupta, R. et al. Budget Impact of Microbial Cell-Free DNA Testing Using the Karius® Test as an Alternative to Invasive Procedures in Immunocompromised Patients with Suspected Invasive Fungal Infections. Appl Health Econ Health Policy 19, 231–241 (2021). https://doi.org/10.1007/s40258-020-00611-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-020-00611-7