Abstract
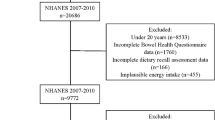
The associations between copper and zinc intake with the risk of inflammatory bowel disease (IBD) and fecal incontinence symptoms in the general population are not well understood. This study aims to evaluate the associations of zinc and copper intake with the risk of IBD and fecal incontinence symptoms in adults aged ≥ 20 years using data from the 2009–2010 National Health and Nutritional Examination Surveys (NHANES) (N = 5593). The presence of IBD was analyzed from the NHANES data, directly querying the presence or absence of ulcerative colitis (UC) and Crohn’s disease (CD). Fecal incontinence symptoms including accidental bowel leakage of gas, mucus, liquid, or solid stool were determined by using the bowel health questionnaire. Multivariable logistic regressions models were performed controlling for confounding factors (dietary, lifestyle, psychological, and health conditions). No associations between either zinc or copper intake with IBD were found. However, zinc intake was independently associated with increased risk of bowel leakage of gas or liquid. Compared with quartile 1, the multivariate-adjusted ORs (95%CI) of bowel leakage of gas across quartiles 2–4 of zinc intake were 1.41 (1.15–1.71), 1.30 (1.00–1.68), and 1.61 (1.16–2.23). Likewise, there was a trend for higher odds of bowel leakage of liquid among participants in the higher zinc intake. Compared with quartile 1, the multivariate-adjusted ORs (95%CI) of bowel leakage of liquid across quartiles 2–4 of zinc intake were 3.55 (0.94–13.41), 3.65 (1.27–10.47), and 5.06 (1.25–20.50). Future prospective studies are warranted to confirm these findings.
Similar content being viewed by others
References
Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema HW, Kaplan GG (2012) Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 142:46–54 e30
Zand A, van Deen WK, Inserra EK, Hall L, Kane E, Centeno A, Choi JM, Ha CY, Esrailian E, D’Haens GR, Hommes DW (2015) Presenteeism in inflammatory bowel diseases: a hidden problem with significant economic impact. Inflamm Bowel Dis 21:1623–1630
Clara Abraham MD, Judy H. Cho MD (2009) Inflammatory bowel disease. N Engl J Med 2066–2078
Kaplan GG, Ng SC (2017) Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology 152:313–321
Phillips CM, Chen LW, Heude B, Bernard JY, Harvey NC, Duijts L, Mensink-Bout SM, Polanska K, Mancano G, Suderman M, Shivappa N, Hébert JR (2019) Dietary inflammatory index and non-communicable disease risk: a narrative review. Nutrients 11
Gammoh NZ, Rink L (2017) Zinc in infection and inflammation. Nutrients 9
Lewandowski Ł, Kepinska M, Milnerowicz H (2019) The copper-zinc superoxide dismutase activity in selected diseases. Eur J Clin Invest 49:e13036
Mohammadi E, Qujeq D, Taheri H, Hajian-Tilaki K (2017) Evaluation of serum trace element levels and superoxide dismutase activity in patients with inflammatory bowel disease: translating basic research into clinical application. Biol Trace Elem Res 177:235–240
Stochel-Gaudyn A, Fyderek K, Kościelniak P (2019) Serum trace elements profile in the pediatric inflammatory bowel disease progress evaluation. J Trace Elem Med Biol 55:121–126
Weng YJ, Gan HY, Li X, Huang Y, Li ZC, Deng HM, Chen SZ, Zhou Y, Wang LS, Han YP, Tan YF, Song YJ, du ZM, Liu YY, Wang Y, Qin N, Bai Y, Yang RF, Bi YJ, Zhi FC (2019) Correlation of diet, microbiota and metabolite networks in inflammatory bowel disease. J Dig Dis 20:447–459
Rogler G, Vavricka S, (2015) Exposome in IBD: recent insights in environmental factors that influence the onset and course of IBD. Inflamm Bowel Dis 21:400–408
Bhandari S, Larson ME, Kumar N, Stein D (2017) Association of inflammatory bowel disease (ibd) with depressive symptoms in the united states population and independent predictors of depressive symptoms in an ibd population: a NHANES study. Gut Liver 11:512–519
de Silva PS, Yang X, Korzenik JR, Goldman RH, Arheart KL, Caban-Martinez AJ (2017) Association of urinary phenolic compounds, inflammatory bowel disease and chronic diarrheal symptoms: Evidence from the National Health and Nutrition Examination Survey. Environ Pollut 229:621–626
Opstelten JL, Leenders M, Dik VK, Chan SS, van Schaik FD, Khaw KT, Luben R, Hallmans G, Karling P, Lindgren S, et al (2016) Dairy products, dietary calcium, and risk of inflammatory bowel disease: results from a european prospective cohort investigation. Inflamm Bowel Dis 22:1403–1411
International Diabetes Federation Guideline Development Group. (2014) Global guideline for type 2 diabetes. Diabetes Res Clin Pract 104:1–52
Whelton PK, Carey RM, Aronow WS, Casey DJ, Collins KJ, Dennison HC, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 71:2199–2269
Ballou S, Singh P, Rangan V, Iturrino J, Nee J, Lembo A (2019) Obesity is associated with significantly increased risk for diarrhoea after controlling for demographic, dietary and medical factors: a cross-sectional analysis of the 2009-2010 National Health and Nutrition Examination Survey. Aliment Pharmacol Ther 50:1019–1024
Chasapis CT, Ntoupa PA, Spiliopoulou CA, Stefanidou ME (2020) Recent aspects of the effects of zinc on human health. Arch Toxicol 94:1443–1460
Ringstad J, Kildebo S, Thomassen Y (1993) Serum selenium, copper, and zinc concentrations in Crohn's disease and ulcerative colitis. Scand J Gastroenterol 28:605–608
Scrimgeour AG, Lukaski HC (2008) Zinc and diarrheal disease: current status and future perspectives. Curr Opin Clin Nutr Metab Care 11:711–717
Acknowledgments
The authors thank the National Center for Health Statistics of the Centers for Disease Control and Prevention for sharing the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None
Ethical Approval
NHANES was approved by the National Center for Health Statistics Research Ethics Review Board.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 43 kb)
Rights and permissions
About this article
Cite this article
Zhang, L., Shao, F. & Li, L. Association of Copper and Zinc Intake with Inflammatory Bowel Disease and Fecal Incontinence Symptoms: Evidence from the National Health and Nutrition Examination Survey. Biol Trace Elem Res 199, 2543–2551 (2021). https://doi.org/10.1007/s12011-020-02390-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-020-02390-7