Abstract
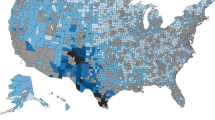
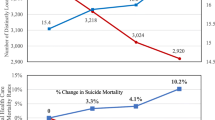
There is an elevated risk of suicide among people living in rural areas, and the rural–urban disparity in death by suicide is growing in the general United States population. The department of Veterans Affairs (VA) implemented programs targeting rural health in 2007 and suicide prevention in 2008. Rural–urban differences in suicide rates among VA users have not been examined since 2010. We sought to understand whether the rural–urban disparity in suicide risk among VA users decreased during a time of contemporaneous VA efforts to improve access to mental health care for rural Veterans and to improve the effectiveness of mental health services at preventing suicide. We performed a retrospective cohort study examining differences in the raw and adjusted annual suicide rate among rural and urban VA users between 2003 and 2017. All VHA users 2003–2017. Descriptive statistics are presented for all VHA users in 2017. This includes 6,120,355 unique VA users, 32.0% (n = 1,955,935) of whom lived at a rural address. Raw rates of death by suicide were higher in rural VA users than urban VA users overall (33.3 vs. 29.1 deaths per 100,000 population) and across years, but the age, sex, and race-adjusted rates converged in 2005. White VA users had over triple the rate of death by suicide as black VA users, and lived disproportionally in rural areas. The rural–urban suicide disparity among VA users persists. However, the disparity appears to be driven by differences in the racial composition of rural and urban patients, which were not accounted for in prior studies.



Similar content being viewed by others
References
Adams, S. V., Mader, M. J., Bollinger, M. J., Wong, E. S., Hudson, T. J., & Littman, A. J. (2019). Utilization of interactive clinical video telemedicine by rural and urban Veterans in the Veterans Health Administration Health Care System. The Journal of Rural Health, 35, 308–318. https://doi.org/10.1111/jrh.12343
Alonso, J., Codony, M., Kovess, V., Angermeyer, M. C., Katz, S. J., Haro, J. M., et al. (2007). Population level of unmet need for mental healthcare in Europe. British Journal of Psychiatry, 190, 299–306. https://doi.org/10.1192/bjp.bp.106.022004
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: fifth edition (DSM-5). Washington, DC: American Psychiatric Association.
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10.
Bohnert, A. S., McCarthy, J. F., Ignacio, R. V., Ilgen, M. A., Eisenberg, A., & Blow, F. C. (2013). Misclassification of suicide deaths: Examining the psychiatric history of overdose decedents. Injury Prevention, 19, 326–330. https://doi.org/10.1136/injuryprev-2012-040631
Bossarte, R., Claassen, C. A., & Knox, K. (2010). Veteran suicide prevention: Emerging priorities and opportunities for intervention. Military Medicine, 175, 461–462.
Breiman, L. (2001). Random forests. Machine Learning, 45, 5–32.
Breiman, L., Cutler, A., Liaw, A., & Wiener, M. (2018). Breiman and Cutler’s random forests for classification and regression (Package ‘randomForest’). CRAN: The Comprehensive R Archive Network. Retrieved September 9, 2020 from https://cran.r-project.org/web/packages/randomForest/randomForest.pdf
Britton, P. C., Bohnert, K. M., Ilgen, M. A., Kane, C., Stephens, B., & Pigeon, W. R. (2017). Suicide mortality among male veterans discharged from Veterans Health Administration acute psychiatric units from 2005 to 2010. Social Psychiatry and Psychiatric Epidemiology, 52, 1081–1087. https://doi.org/10.1007/s00127-017-1377-x
Bumgarner, D. J., Polinsky, E. J., Herman, K. G., Fordiani, J. M., Lewis, C. P., Hansen, S. K., et al. (2017). Mental health care for rural veterans: A systematic literature review, descriptive analysis, and future directions. Journal of Rural Mental Health, 41, 222–233.
Carey, K., Montez-Rath, M. E., Rosen, A. K., Christiansen, C. L., Loveland, S., & Ettner, S. L. (2008). Use of VA and Medicare services by dually eligible veterans with psychiatric problems. Health Services Research, 43, 1164–1183. https://doi.org/10.1111/j.1475-6773.2008.00840.x
Conner, K. R., Bohnert, A. S., McCarthy, J. F., Valenstein, M., Bossarte, R., Ignacio, R., et al. (2013). Mental disorder comorbidity and suicide among 2.96 million men receiving care in the Veterans Health Administration Health System. Journal of Abnormal Psychology, 122, 256–263. https://doi.org/10.1037/a0030163
Conner, K. R., Bossarte, R. M., He, H., Arora, J., Lu, N., Tu, X. M., et al. (2014). Posttraumatic stress disorder and suicide in 5.9 million individuals receiving care in the Veterans Health Administration Health System. Journal of Affective Disorders, 166, 1–5. https://doi.org/10.1016/j.jad.2014.04.067
Crnek-Georgeson, K. T., Wilson, L. A., & Page, A. (2017). Factors influencing suicide in older rural males: A review of Australian studies. Rural and Remote Health, 17, 4020. https://doi.org/10.22605/RRH4020
Fontanella, C. A., Hiance-Steelesmith, D. L., Phillips, G. S., Bridge, J. A., Lester, N., Sweeney, H. A., et al. (2015). Widening rural–urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatrics, 169, 466–473. https://doi.org/10.1001/jamapediatrics.2014.3561
Franklin, K. (2019). National suicide strategy. Federal Practitioner, 36, 107–109.
Gibbs, J. T. (1997). African–American suicide: A cultural paradox. Suicide and Lifethreatening Behavior, 27, 68–79.
Giles-Sims, J., & Lockhart, C. (2006). Explaining cross-state differences in elderly suicide rates and identifying state-level public policy responses that reduce rates. Suicide and Lifethreatening Behavior, 36, 694–708. https://doi.org/10.1521/suli.2006.36.6.694
Goss, C. W., Richardson, W. J., Jr., & Shore, J. H. (2019). Outcomes and lessons learned from the tribal Veterans representative program: A model for system engagement. Journal of Community Health, 44, 1076–1085. https://doi.org/10.1007/s10900-019-00683-0
Hirsch, J. K. (2006). A review of the literature on rural suicide: Risk and protective factors, incidence, and prevention. Crisis, 27, 189–199. https://doi.org/10.1027/0227-5910.27.4.189
Hoffmire, C. A., Kemp, J. E., & Bossarte, R. M. (2015). Changes in suicide mortality for veterans and nonveterans by gender and history of VHA service use, 2000–2010. Psychiatric Services (Washington, D. C.), 66, 959–965. https://doi.org/10.1176/appi.ps.201400031
Holder, K. A. (2016). Veterans in Rural America: 2011–2015. Washington, DC: American Community Survey Reports, ACS-36, U.S. Census Bureau.
Howren, M. B., Kazmerzak, D., Kemp, R. W., Boesen, T. J., Capra, G., & Abrams, T. E. (2020). Identification of military veterans upon implementation of a standardized screening process in a Federally Qualified Health Center. Journal of Community Health, 45, 465–468. https://doi.org/10.1007/s10900-019-00761-3
Ivey-Stephenson, A. Z., Crosby, A. E., Jack, S. P. D., Haileyesus, T., & Kresnow-Sedacca, M. J. (2017). Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death—United States, 2001–2015. MMWR Surveillance Summaries, 66, 1–16. https://doi.org/10.15585/mmwr.ss6618a1
Jacobs, J. C., Blonigen, D. M., Kimerling, R., Slightam, C., Gregory, A. J., Gurmessa, T., et al. (2019). Increasing mental health care access, continuity, and efficiency for veterans through telehealth with video tablets. Psychiatric Services (Washington, D. C.), 70, 976–982. https://doi.org/10.1176/appi.ps.201900104
Judd, F., Cooper, A. M., Fraser, C., & Davis, J. (2006). Rural suicide–people or place effects? Australian and New Zealand Journal of Psychiatry, 40, 208–216. https://doi.org/10.1080/j.1440-1614.2006.01776.x
Kaslow, N. J., Sherry, A., Bethea, K., Wyckoff, S., Compton, M. T., Grall, M. B., et al. (2005). Social risk and protective factors for suicide attempts in low income African American men and women. Suicide and Lifethreatening Behavior, 35, 400–412. https://doi.org/10.1521/suli.2005.35.4.400
Kessler, R. C., Hwang, I., Hoffmire, C. A., McCarthy, J. F., Petukhova, M. V., Rosellini, A. J., et al. (2017). Developing a practical suicide risk prediction model for targeting high-risk patients in the Veterans health Administration. International Journal of Methods in Psychiatric Research. https://doi.org/10.1002/mpr.1575
Kim, H. J., Fay, M. P., Feuer, E. J., & Midthune, D. N. (2000). Permutation tests for joinpoint regression with applications to cancer rates. Statistics in Medicine, 19, 335–351. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3%3c335:aid-sim336%3e3.0.co;2-z
Kizer, K. W., & Dudley, R. A. (2009). Extreme makeover: Transformation of the Veterans Health Care System. Annual Review of Public Health, 30, 313–339. https://doi.org/10.1146/annurev.publhealth.29.020907.090940
Klugman, J., Condran, G., & Wray, M. (2013). The role of medicolegal systems in producing geographic variation in suicide rates. Social Science Quarterly, 94, 462–489.
Kubrin, C. E., & Wadsworth, T. (2009). Explaining suicide among blacks and whites: How socioeconomic factors and gun availability affect race-specific suicide rates. Social Science Quarterly, 90, 1203–1227.
Kudler, H., Straits-Troster, K., & Brancu, M. (2011). Initiatives to improve access to behavioral health services in the Veterans Affairs Health System. North Carolina Medical Journal, 72, 40–42.
Levis, M., Leonard Westgate, C., Gui, J., Watts, B. V., & Shiner, B. (2020). Natural language processing of clinical mental health notes may add predictive value to existing suicide risk models. Psychological Medicine. https://doi.org/10.1017/S0033291720000173
Li, M., & Katikireddi, S. V. (2019). Urban-rural inequalities in suicide among elderly people in China: A systematic review and meta-analysis. International Journal for Equity in Health, 18, 2. https://doi.org/10.1186/s12939-018-0881-2
McCarthy, J. F., Blow, F. C., Ignacio, R. V., Ilgen, M. A., Austin, K. L., & Valenstein, M. (2012). Suicide among patients in the Veterans Affairs Health System: Rural–urban differences in rates, risks, and methods. American Journal of Public Health, 102, S111–S117. https://doi.org/10.2105/AJPH.2011.300463
McCarthy, J. F., Bossarte, R. M., Katz, I. R., Thompson, C., Kemp, J., Hannemann, C. M., et al. (2015). Predictive modeling and concentration of the risk of suicide: Implications for preventive interventions in the US Department of Veterans Affairs. American Journal of Public Health, 105, 1935–1942. https://doi.org/10.2105/AJPH.2015.302737
Mohatt, N. V., Billera, M., Demers, N., Monteith, L. L., & Bahraini, N. H. (2018). A menu of options: Resources for preventing veteran suicide in rural communities. Psychological Services, 15, 262–269. https://doi.org/10.1037/ser0000203
Monteith, L. L., Smith, N. B., Holliday, R., Dorsey Holliman, B. A., LoFaro, C. T., & Mohatt, N. V. (2020a). “We’re Afraid to Say Suicide”: Stigma as a barrier to implementing a community-based suicide prevention program for rural veterans. The Journal of Nervous and Mental Disease, 208, 371–376. https://doi.org/10.1097/NMD.0000000000001139
Monteith, L. L., Wendleton, L., Bahraini, N. H., Matarazzo, B. B., Brimner, G., & Mohatt, N. V. (2020b). Together with veterans: VA national strategy alignment and lessons learned from community-based suicide prevention for rural veterans. Suicide and Lifethreatening Behavior, 50, 588–600. https://doi.org/10.1111/sltb.12613
Mott, J. M., Grubbs, K. M., Sansgiry, S., Fortney, J. C., & Cully, J. A. (2015). Psychotherapy utilization among rural and urban veterans from 2007 to 2010. The Journal of Rural Health, 31, 235–243. https://doi.org/10.1111/jrh.12099
Muggeo, V. M. R. (2019). Regression models with break-points/change-points estimation (Package ‘segmented’). CRAN: The Comprehensive R Archive Network. Retrieved September 9, 2020 from https://cran.r-project.org/web/packages/segmented/segmented.pdf
Oh, H., Stickley, A., Koyanagi, A., Yau, R., & DeVylder, J. E. (2019). Discrimination and suicidality among racial and ethnic minorities in the United States. Journal of Affective Disorders, 245, 517–523. https://doi.org/10.1016/j.jad.2018.11.059
Quan, H., Sundararajan, V., Halfon, P., Fong, A., Burnand, B., Luthi, J. C., et al. (2005). Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care, 43, 1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Riblet, N., Shiner, B., Watts, B. V., Mills, P., Rusch, B., & Hemphill, R. R. (2017a). Death by suicide within 1 week of hospital discharge: A retrospective study of root cause analysis reports. The Journal of Nervous and Mental Disease, 205, 436–442. https://doi.org/10.1097/NMD.0000000000000687
Riblet, N. B. V., Shiner, B., Young-Xu, Y., & Watts, B. V. (2017b). Strategies to prevent death by suicide: Meta-analysis of randomised controlled trials. British Journal of Psychiatry, 210, 396–402. https://doi.org/10.1192/bjp.bp.116.187799
Rockett, I. R. H., & Caine, E. D. (2020). Reconciling suicides with “accidental” drug-intoxication deaths: A behaviorally based definition of self-injury mortality. American Journal of Public Health, 110, 73–74. https://doi.org/10.2105/AJPH.2019.305422
Steelesmith, D. L., Fontanella, C. A., Campo, J. V., Bridge, J. A., Warren, K. L., & Root, E. D. (2019). Contextual factors associated with county-level suicide rates in the United States, 1999 to 2016. JAMA Network Open, 2, e1910936. https://doi.org/10.1001/jamanetworkopen.2019.10936
United States Department of Veterans Affairs. (2019). 2019 National Veteran suicide prevention annual report. Washington, DC.
VA Office of Rural Health. (2015). VHA and ORH Adopt New System to Define “Rural”. Retrieved September 9, 2020 from https://www.ruralhealth.va.gov/rural-definition.asp
Wang, Z., Yu, C., Wang, J., Bao, J., Gao, X., & Xiang, H. (2016). Age-period-cohort analysis of suicide mortality by gender among white and black Americans, 1983–2012. International Journal for Equity in Health, 15, 107. https://doi.org/10.1186/s12939-016-0400-2
West, A. N., Lee, R. E., Shambaugh-Miller, M. D., Bair, B. D., Mueller, K. J., Lilly, R. S., et al. (2010). Defining “rural” for veterans’ health care planning. The Journal of Rural Health, 26, 301–309. https://doi.org/10.1111/j.1748-0361.2010.00298.x
West, A. N., & Weeks, W. B. (2009). Health care expenditures for urban and rural veterans in Veterans Health Administration Care. Health Services Research, 44, 1718–1734. https://doi.org/10.1111/j.1475-6773.2009.00988.x
Funding
This work was sponsored by the Department of Veteran’s Affairs Office of Rural Health (ORH15533) and the National Center for Patient Safety Center of Inquiry Program (PSCI-WRJ-SHINER). Opinions are those of the authors and not necessarily those of the Department of Veterans Affairs, the Office of Rural Health, or the National Center for Patient Safety.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Human and animal rights
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national VA research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Veterans IRB of Northern New England (VINNE) approved this study. The VA National Data Systems approved the use of VA data for this study.
Informed consent
A waiver of informed consent was obtained for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
See Table 3.
Appendix 2
See Table 4.
Appendix 3
See Table 5.
Rights and permissions
About this article
Cite this article
Shiner, B., Peltzman, T., Cornelius, S.L. et al. Recent trends in the rural–urban suicide disparity among veterans using VA health care. J Behav Med 44, 492–506 (2021). https://doi.org/10.1007/s10865-020-00176-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-020-00176-9