Abstract
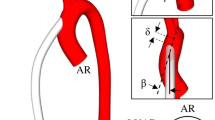
This article investigates a specific type of cardiac assist device, its functional performance, and its effects on the hemodynamic patterns of blood flow through the aortic network. The aforementioned assist device can be implanted in a given patient suffering from left ventricular failure. Our previous study focused on multi-balloons device. The current cardiac assist device is composed of two semi-cylindrical double-layer balloons surrounding the ascending aorta, thereby increasing the force with which blood will be pumped into the circulatory system with its inflation and deflation mechanism. The inflation and deflation of the balloon take place during the diastolic and systolic phases of the heart, respectively, by pumping and suctioning a specific gas coming from a micropump into or out of the space between the two layers of the balloons. A three-dimensional model of the aortic network assisted by the cardiac device is constructed based on the patient’s individual anatomical and physiological conditions and simulated within two complete cardiac cycles using the fluid–structure interaction analysis. The simulation is performed using the assumptions of linear elastic materials for the balloon and the aorta, and Newtonian and incompressible fluid for the blood. Result shows that the maximum outflow of the descending aorta increases by 20 ml/s and 10 ml/s in the brachiocephalic artery at time 0.4 s (maximum inflation). This increase is equal to 5 ml/s in the carotid and subclavian arteries. During the time period of 0.4–0.5 s (constant applied pressure), the balloon has no considerable movement. The outflow experiences a nearly uniform flow with slight oscillations within this interval in the presence of the assist device. The net energy of the blood flow is decreased if the Young’s modulus of the balloon part of the assist device increases. Furthermore, the stress generated at the outer curvature of the aorta is higher than that of inner curvature in case of using cardiac assist device. This study demonstrates the relevance of the three-dimensional model in clinical practice. Such simulation can provide clinicians and surgeons with relevant information in order to select the most patient-centered and clinically appropriate cardiac assist device addressing the pathological conditions of a specific patient. Furthermore, this study can be a source of comparison with the previous study on multi-balloons device.
Similar content being viewed by others
References
Alagheband M, Rahmani S, Alizadeh M, Karimi A, Navidbakhsh M (2015) Hemodynamic investigation of intraluminal thrombus effect on the wall stress in a stented three-layered aortic aneurysm model under pulsatile flow. Artery Res 10:11–19
Alizadeh M, Tehrani P, Rahmani S (2014) Hemodynamic simulation of blood flow in a new type of cardiac assist device named AVICENA. Proc Inst Mech Eng Part H J Eng Med 228:824–832
Arefin MS, Morsi YS (2014) Fluid structure interaction (FSI) simulation of the left ventricle (LV) during the early filling wave (E-wave), diastasis and atrial contraction wave (A-wave). Australas Phys Eng Sci Med 37:413–423
Bazilevs Y, Gohean JR, Hughes TJR, Moser RD, Zhang Y (2009) Patient-specific isogeometric fluid–structure interaction analysis of thoracic aortic blood flow due to implantation of the Jarvik 2000 left ventricular assist device. Comput Methods Appl Mech Eng 198:3534–3550
Caballero AD, Laín S (2013) A review on computational fluid dynamics modelling in human thoracic aorta. Cardiovasc Eng Technol 4:103–130
Caruso MV, Gramigna V, Rossi M, Serraino GF, Renzulli A, Fragomeni G (2015) A computational fluid dynamics comparison between different outflow graft anastomosis locations of Left Ventricular Assist Device (LVAD) in a patient-specific aortic model. Int J Numer Method Biomed Eng 31:e02700
Chi JWH (1973) An analysis and design of implantable blood heat exchangers for artificial hearts. Int J Eng Sci 1973(11):637IN5639–638IN6648
El Baroudi A, Razafimahery F, Rakotomanana L (2014) Fluid–structure interaction within three-dimensional models of an idealized arterial wall. Int J Eng Sci 84:113–126
Fendler TJ, Spertus JA, Gosch KL, Jones PG, Bruce JM, Nassif ME et al (2015) Incidence and predictors of cognitive decline in patients with left ventricular assist devices. Circ Cardiovasc Qual Outcomes 8:285–291
Fraser KH, Taskin ME, Griffith BP, Wu ZJ (2011) The use of computational fluid dynamics in the development of ventricular assist devices. Med Eng Phys 33:263–280
Gasser TC, Ogden RW, Holzapfel GA (2005) Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J R Soc Interface 3:15–35
Givertz MM (2011) Ventricular assist devices: important information for patients and families. Circulation 124:e305–e311
Good BC, Deutsch S, Manning KB (2016) Continuous and pulsatile pediatric ventricular assist device hemodynamics with a viscoelastic blood model. Cardiovasc Eng Technol 7:23–43
Hanson BM, Levesley MC, Watterson K, Walker PG (2006) Simulation of the human cardiovascular system for real-time physical interaction with an assist device. In: 2005 IEEE engineering medicine biology 27th annual conference. IEEE, pp 409–412
Hsu M-C, Kamensky D, Xu F, Kiendl J, Wang C, Wu MCH et al (2015) Dynamic and fluid–structure interaction simulations of bioprosthetic heart valves using parametric design with T-splines and Fung-type material models. Comput Mech 55:1211–1225
Humphrey JD, Holzapfel GA (2012) Mechanics, mechanobiology, and modeling of human abdominal aorta and aneurysms. J Biomech 45:805–814
Hutchison SJ, Thaker KB, Anthony P, Chandraratna N (1994) Effects of intraaortic balloon counterpulsation on flow velocity in stenotic left main coronary arteries from transesophageal echocardiography. Am J Cardiol 74:1063–1065
Kamensky D, Hsu M-C, Schillinger D, Evans JA, Aggarwal A, Bazilevs Y et al (2015) An immersogeometric variational framework for fluid–structure interaction: application to bioprosthetic heart valves. Comput Methods Appl Mech Eng 284:1005–1053
Katz ES, Tunick PA, Kronzon I (1992) Observations of coronary flow augmentation and balloon function during intraaortic balloon counterpulsation using transesophageal echocardiography. Am J Cardiol 69:1635–1639
Khaghani A, Andrews GT, Bowles C, Smith NG (2006) Blood circulation assistance device
Legget ME, Peters WS, Milsom FP, Clark JS, West TM, French RL et al (2005) Extra-aortic balloon counterpulsation an intraoperative feasibility study. Circulation 2005(112):I-26
Long CC, Marsden AL, Bazilevs Y (2013) Fluid–structure interaction simulation of pulsatile ventricular assist devices. Comput Mech 52:971–981
Maul TM, Kocyildirim E, Johnson CA, Daly AR, Olia SE, Woolley JR et al (2011) In vitro and in vivo performance evaluation of the second developmental version of the pediaflow pediatric ventricular assist device. Cardiovasc Eng Technol 2:253–262
McCabe JC, Abel RM, Subramanian VA, Guy WA (1978) Complications of intra-aortic balloon insertion and counterpulsation. Circulation 57:769–773
Oshima K, Morishita Y, Hinohara H, Kadoi Y, Hayashi Y, Tajima Y et al (2005) Prolonged use for at least 10 days of intraaortic balloon pumping (IABP) for heart failure. Int Heart J 46:1041–1047
Prondzinsky R, Lemm H, Swyter M, Wegener N, Unverzagt S, Carter JM et al (2010) Intra-aortic balloon counterpulsation in patients with acute myocardial infarction complicated by cardiogenic shock: the prospective, randomized IABP SHOCK Trial for attenuation of multiorgan dysfunction syndrome. Crit Care Med 38:152–160
Rahmani S, Alagheband M, Karimi A, Alizadeh M, Navidbakhsh M (2015) Wall stress in media layer of stented three-layered aortic aneurysm at different intraluminal thrombus locations with pulsatile heart cycle. J Med Eng Technol. https://doi.org/10.3109/03091902.2015.1040173
Rahmani S, Navidbakhsh M, Alizadeh M (2018) Investigation of a new prototype of multi-balloons LVAD using FSI. J Braz Soc Mech Sci Eng. https://doi.org/10.1007/s40430-017-0923-5
Rodriguez LE, Suarez EE, Loebe M, Bruckner BA (2013) Ventricular assist devices (VAD) therapy: new technology, new hope? Methodist Debakey Cardiovasc J 9:32–37
Rogers A, Morris LB, Williams KR (1972) Artificial heart ventricular design having space and performance characteristics comparable to the heart. Int J Eng Sci 10:1037–1047
Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W et al (2001) Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med 345:1435–1443
Samyn MM, Dholakia R, Wang H, Co-Vu J, Yan K, Widlansky ME et al (2015) Cardiovascular magnetic resonance imaging-based computational fluid dynamics/fluid–structure interaction pilot study to detect early vascular changes in pediatric patients with type 1 diabetes. Pediatr Cardiol 36:851–861
Slaughter MS, Sobieski MA II, Tamez D, Horrell T, Graham J, Pappas PS et al (2009) HeartWare miniature axial-flow ventricular assist device: design and initial feasibility test. Texas Hear Inst J 36:12
Taelman L, Degroote J, Swillens A, Vierendeels J, Segers P (2014) Fluid–structure interaction simulation of pulse propagation in arteries: numerical pitfalls and hemodynamic impact of a local stiffening. Int J Eng Sci 77:1–13
Tehrani P, Rahmani S, Karimi A, Alizadeh M, Navidbakhsh M (2014) Modeling of balloon part of a new cardiac assist device known as AVICENA. J Biomater Tissue Eng 4:772–777
Toungara M, Geindreau C (2013) Influence of a poro-mechanical modeling of the intra-luminal thrombus and the anisotropy of the arterial wall on the prediction of the abdominal aortic aneurysm rupture. Cardiovasc Eng Technol 4:192–208
Trachet B, Bols J, Degroote J, Verhegghe B, Stergiopulos N, Vierendeels J et al (2015) An animal-specific FSI model of the abdominal aorta in anesthetized mice. Ann Biomed Eng 43:1298–1309
Tuzun E, Roberts K, Cohn WE, Sargin M, Gemmato CJ, Radovancevic B et al (2007) In vivo evaluation of the HeartWare centrifugal ventricular assist device. Texas Hear Inst J 34:406
Wu Y, Allaire P, Tao G, Olsen D (2005) Modeling, estimation and control of cardiovascular systems with a left ventricular assist device. In: Proceedings 2005, American control conference 2005. IEEE, pp 3841–3846
Zehetgruber M, Mundigler G, Christ G, Merhaut C, Klaar U, Kratochwill C et al (1997) Relation of hemodynamic variables to augmentation of left anterior descending coronary flow by intraaortic balloon pulsation in coronary artery disease. Am J Cardiol 80:951–955
Acknowledgements
This study was supported by the Tehran Heart Center (THC), Professor Hossein Ahmadi, full professor at the Medical University of Tehran and cardiovascular surgeon at THC. We appreciate the collaboration of our colleagues from THC who provided insight and expertise that profoundly helped this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shahrokh Rahmani, Alireza Heidari, Behdad Saed, Adel Mahpour, Mahdi Navidbakhsh and Mansour Alizadeh declare that they have no conflict of interest.
Ethical Approval
This article used the data from a patient with the permission from the THC research laboratory.
Electronic supplementary material
Below is the link to the electronic supplementary material.


Rights and permissions
About this article
Cite this article
Rahmani, S., Heidari, A., Saed, B. et al. Biomechanical, Structural and Performance Analysis of a Specific Type of Cardiac Assist Device Used in Left Ventricular Failures. Iran J Sci Technol Trans Mech Eng 44, 1053–1064 (2020). https://doi.org/10.1007/s40997-019-00304-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40997-019-00304-0