Abstract
Background
Hypertension drives myocardial remodeling, leading to changes in structure, composition and mechanical behavior, including residual stress, which are linked to heart disease progression in a gender-specific manner. Emerging therapies are also targeting constituent-specific pathological features. All previous studies, however, have characterized remodeling in the intact tissue, rather than isolated tissue constituents, and did not include sex as a biological variable.
Objective
In this study we first identified the contribution of collagen fiber network and myocytes to the myocardial residual stress/strain in Dahl-Salt sensitive rats fed with high fat diet. Then, we quantified the effect of hypertension on the remodeling of the left ventricle (LV), as well as the existence of sex-specific remodeling features.
Methods
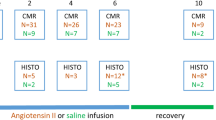
We performed mechanical tests (opening angle, ring-test) and histological analysis on isolated constituents and intact tissue of the LV. Based on the measurements from the tests, we performed a stress analysis to evaluate the residual stress distribution. Statistical analysis was performed to identify the effects of constituent isolation, elevated blood pressure, and sex of the animal on the experimental measurements and modeling results.
Results
Hypertension leads to reduced residual stress/strain in the intact tissue, isolated collagen fibers, and isolated myocytes in male and female rats. Collagen remains the largest contributor to myocardial residual stress in both normotensive and hypertensive animals. We identified sex-differences in both hypertensive and normotensive animals.
Conclusions
We observed both constituent- and sex-specific remodeling features in the LV of an animal model of hypertension.








Similar content being viewed by others
References
Rossi MA (1998) Pathologic fibrosis and connective tissue matrix in left ventricular hypertrophy due to chronic arterial hypertension in humans. J Hypertens 16(7):1031–1041
Omens JH, Milkes DE, Covell JW (1995) Effects of pressure overload on the passive mechanics of the rat left ventricle. Ann Biomed Eng 23(2):152–163
Oktay AA, Shah SJ (2014) Current perspectives on systemic hypertension in heart failure with preserved ejection fraction. Current cardiology reports 16(12):545
Teo LYL, Chan LL, Lam CSP (2016) Heart failure with preserved ejection fraction in hypertension. Curr Opin Cardiol 31(4):410–416
Omens JH, Rodriguez EK, McCulloch AD (1996) Transmural changes in stress-free myocyte morphology during pressure overload hypertrophy in the rat. J Mol Cell Cardiol 28(9):1975–1983
Taber LA, Chabert S (2002) Theoretical and experimental study of growth and remodeling in the developing heart. Biomech Model Mechanobiol 1(1):29–43
Rodriguez EK, Omens JH, Waldman LK, McCulloch AD (1993) Effect of residual stress on transmural sarcomere length distributions in rat left ventricle. Am J Phys Heart Circ Phys 264(4):H1048–H1056
de Tombe PP, ter Keurs HE (2016) Cardiac muscle mechanics: sarcomere length matters. J Mol Cell Cardiol 91:148–150
Zouein FA, de Castro Brás LE, Da Costa DV, Lindsey ML, Kurdi M, Booz GW (2013) Heart failure with preserved ejection fraction: emerging drug strategies. Journal of cardiovascular pharmacology 62(1):13
Krüger M, Kötter S, Grützner A, Lang P, Andresen C, Redfield MM, Butt E, Dos Remedios CG, Linke WA (2009) Protein kinase G modulates human myocardial passive stiffness by phosphorylation of the titin springs. Circ Res 104(1):87–94
Ramirez LA, Sullivan JC (2018) Sex differences in hypertension: where we have been and where we are going. Am J Hypertens 31(12):1247–1254
Grobbel MR, Shavik SM, Darios E, Watts SW, Lee LC, Roccabianca S (2018) Contribution of left ventricular residual stress by myocytes and collagen: existence of inter-constituent mechanical interaction. Biomech Model Mechanobiol 17(4):985–999
Hajjar RJ, Ingwall JS, Gwathmey JK (1994) Mechanism of action of 2, 3-butanedione monoxime on contracture during metabolic inhibition. Am J Phys Heart Circ Phys 267(1):H100–H108
Alula KM, Biltz R, Xu H, Garver H, Laimon-Thomson EL, Fink GD, Galligan JJ (2019) Effects of high-fat diet on sympathetic neurotransmission in mesenteric arteries from Dahl salt-sensitive rat. Auton Neurosci 222:102599
Demiray H (1972) A note on the elasticity of soft biological tissues. J Biomech 5(3):309–311
Delfino A, Stergiopulos N, Moore JE Jr, Meister JJ (1997) Residual strain effects on the stress field in a thick wall finite element model of the human carotid bifurcation. J Biomech 30(8):777–786
Chen S, Annaidh AN, Roccabianca S (2020) A microstructurally inspired constitutive model for skin mechanics. Biomech Model Mechanobiol 19(1):275–289
Nevo E, Lanir Y (1994) The effect of residual strain on the diastolic function of the left ventricle as predicted by a structural model. J Biomech 27(12):1433–1446
Omens JH, McCulloch AD, Criscione JC (2003) Complex distributions of residual stress and strain in the mouse left ventricle: experimental and theoretical models. Biomech Model Mechanobiol 1(4):267–277
Humphrey, J. D. and Delange, S.L., 2016. Introduction to biomechanics. Springer-Verlag New York
Fernandes R, Garver H, Harkema JR, Galligan JJ, Fink GD, Xu H (2018) Sex differences in renal inflammation and injury in high-fat diet–fed Dahl salt-sensitive rats. Hypertension 72(5):e43–e52
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ (2017) Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 71(6):1269–1324
Kandlikar SS, Fink GD (2011) Mild DOCA-salt hypertension: sympathetic system and role of renal nerves. Am J Phys Heart Circ Phys 300(5):H1781–H1787
Gillis EE, Williams JM, Garrett MR, Mooney JN, Sasser JM (2015) The Dahl salt-sensitive rat is a spontaneous model of superimposed preeclampsia. Am J Phys Regul Integr Comp Phys 309(1):R62–R70
Greene AS, Yu ZY, Roman RJ, Cowley AW Jr (1990) Role of blood volume expansion in Dahl rat model of hypertension. Am J Phys Heart Circ Phys 258(2):H508–H514
Omens JH, Vaplon SM, Fazeli B, McCulloch AD (1998) Left ventricular geometric remodeling and residual stress in the rat heart. J Biomech Eng 120(6):715–719
Genet M, Rausch MK, Lee LC, Choy S, Zhao X, Kassab GS, Kozerke S, Guccione JM, Kuhl E (2015) Heterogeneous growth-induced prestrain in the heart. J Biomech 48(10):2080–2089
Tam MC, Lee R, Cascino TM, Konerman MC, Hummel SL (2017) Current perspectives on systemic hypertension in heart failure with preserved ejection fraction. Current hypertension reports 19(2):12
Parikh JD, Hollingsworth KG, Wallace D, Blamire AM, MacGowan GA (2017) Left ventricular functional, structural and energetic effects of normal aging: comparison with hypertension. PloS one 12(5):e0177404
Duca F, Zotter-Tufaro C, Kammerlander AA, Aschauer S, Binder C, Mascherbauer J, Bonderman D (2018) Gender-related differences in heart failure with preserved ejection fraction. Sci Rep 8(1):1–9
Beale AL, Nanayakkara S, Segan L, Mariani JA, Maeder MT, van Empel V, Vizi D, Evans S, Lam CS, Kaye DM (2019) Sex differences in heart failure with preserved ejection fraction pathophysiology: a detailed invasive hemodynamic and echocardiographic analysis. JACC: Heart Failure 7(3):239–249
Gori M, Lam CS, Gupta DK, Santos AB, Cheng S, Shah AM, Claggett B, Zile MR, Kraigher-Krainer E, Pieske B, Voors AA (2014) Sex-specific cardiovascular structure and function in heart failure with preserved ejection fraction. Eur J Heart Fail 16(5):535–542
Omens JH, Fung YC (1990) Residual strain in rat left ventricle. Circ Res 66(1):37–45
Acknowledgments
This work was supported by NSF CMMI GRANT #1933768 and NIH GRANT #P01HL070687. We kindly acknowledge Kibrom M. Alula, Emma Darios Flood, and Ari Hollander for their help with animals and experiments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
In order to calculate the stress distribution across the wall given by equation (4), we used each sample’s individual geometry from the open configuration (Ri, Ro, Φ), along with their pooled material properties (cc, kc, cm, km) and constituent area fractions (ϕc, ϕm). It should be noted that when using equation (3) for intact tissue, ϕc and ϕm were equal to their experimental values. For each sample, the inner and outer radii and axial stretch of the closed, load-free configuration (ρi, ρo, Λz) were estimated by using the deformation gradient in equation (5) and allowing the closed configuration to reach radial and axial equilibrium (using the lsqnonlin function on Matlab)—i.e.,
Additionally, an assumption of incompressibility was made for equation (5), resulting in a third equation used to solve for the unknown geometry:
Finally, for each sample, we had individual geometry measurements (Ri, Ro, Φ, ρi, ρo, Λz), pooled material properties from their breed and sex (cc, kc, cm, km) and collagen and myocytes area fractions (ϕc, ϕm) for the intact tissue, measured for each breed, sex, and diet (i.e. HFD or CD). Using all of this information, we were able to calculate the radial, circumferential, and axial stresses for each group as functions of their non-dimensional radii.
Appendix 2
Transmural residual stretch distribution for one representative sample. Radial stretch (solid line), circumferential stretch (dashed line), and axial stretch (dashed dotted line). For each sample, after evaluating the principal stretches distribution, as shown, we identified values of interest to compare across groups. Specifically, we calculated the minimum and maximum values of the radial and circumferential stretches. Note: while the axial stretch assumes in most cases values close to 1, no plain strain assumption was made
Rights and permissions
About this article
Cite this article
Grobbel, M.R., Lee, L.C., Watts, S.W. et al. Left Ventricular Geometry, Tissue Composition, and Residual Stress in High Fat Diet Dahl-Salt Sensitive Rats. Exp Mech 61, 191–201 (2021). https://doi.org/10.1007/s11340-020-00664-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11340-020-00664-8