Abstract
Summary
We evaluated the fracture risk assessment tool (FRAX) without bone mineral density (BMD) in predicting treatment recommendations for patients with a recent low trauma fracture other than hip or vertebral. The concordance, sensitivity, and specificity were 75.6%, 67.3%, and 78.2%, respectively. FRAX without BMD can be used after a fracture to expedite treatment.
Introduction
The objective of this study was to evaluate the performance of the fracture risk assessment tool (FRAX) without bone mineral density (BMD) in predicting treatment recommendations for patients who recently sustained a low trauma fracture other than hip or vertebral.
Methods
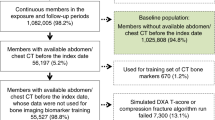
We utilized a clinical database established by the Fracture Liaison Service at the Durham Veterans Affairs Medical Center to identify male and female Veterans age ≥ 50 years who sustained a low trauma non-hip/non-vertebral fracture and underwent dual-energy x-ray absorptiometry (DXA) between October 2013 and April 2018. FRAX without BMD (FRAX-BMI) and FRAX with BMD (FRAX-BMD) were calculated for the 229 patients identified, and whether or not they met the National Osteoporosis Foundation (NOF) guideline treatment thresholds was compared.
Results
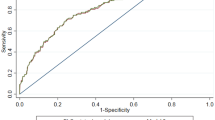
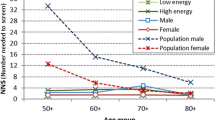
There were 55 (24.0%) patients that met criteria for treatment based on NOF guideline established FRAX-BMD thresholds including 27 (11.8%) patients with osteoporosis by DXA. The concordance of FRAX-BMI in predicting treatment recommendations was 75.6% with a sensitivity of 67.3% and a specificity of 78.2%. The area under the curve (AUC) of FRAX-BMI hip fracture risk was 0.79. Assessment/treatment thresholds for hip fracture risk of 1% < FRAX-BMI < 4% were proposed to maximize sensitivity and specificity.
Conclusion
Among patients who sustained a low trauma non-hip/non-vertebral fracture, FRAX-BMI can be used to stratify risk and identify high-risk patients who could be treated without DXA, low-risk patients who may not need treatment, and intermediate-risk patients to undergo DXA testing.

Similar content being viewed by others
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Banefelt J, Åkesson KE, Spångéus A, Ljunggren O, Karlsson L, Ström O, Ortsäter G, Libanati C, Toth E (2019) Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int 30(3):601–609
Watts NB, Adler RA, Bilezikian JP, Drake MT, Eastell R, Orwoll ES, Finkelstein JS, Endocrine Society (2012) Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 97(6):1802–1822
Cosman F, de Beur SJ, LeBoff M, Lewiecki EM, Tanner B, Randall S, Lindsay R, National Osteoporosis Foundation (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C, The Osteoporosis Methodology Group, The Osteoporosis Research Advisory Group (2002) Meta-analyses of therapies for postmenopausal osteoporosis. IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23(4):570–578
Kanis JA, Svedbom A, Harvey N, McCloskey EV (2014) The osteoporosis treatment gap. J Bone Miner Res 29(9):1926–1928
McKercher HG, Crilly RG, Kloseck M (2000) Osteoporosis management in long-term care. Survey of Ontario physicians. Can Fam Physician 46:2228–2235
Wall M, Lohfeld L, Giangregorio L, Ioannidis G, Kennedy CC, Moser A, Papaioannou A, Morin SN (2013) Fracture risk assessment in long-term care: a survey of long-term care physicians. BMC Geriatr 13:109
Compston J et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43
Colón-Emeric C et al (2013) Use of regional clinical data to identify veterans for a multi-center osteoporosis electronic consult quality improvement intervention. J Hosp Admin 2(1):8–14
Kanis JA, Oden A, Johnell O, Johansson H, de Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, Eisman JA, Fujiwara S, Glüer C, Goltzman D, Hans D, Krieg MA, la Croix A, McCloskey E, Mellstrom D, Melton LJ III, Pols H, Reeve J, Sanders K, Schott AM, Silman A, Torgerson D, van Staa T, Watts NB, Yoshimura N (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18(8):1033–1046
Leslie WD et al (2012) Fracture risk assessment without bone density measurement in routine clinical practice. Osteoporos Int 23(1):75–85
Bouxsein ML, Eastell R, Lui LY, Wu LA, de Papp AE, Grauer A, Marin F, Cauley JA, Bauer DC, Black DM, for the FNIH Bone Quality Project (2019) Change in bone density and reduction in fracture risk: a meta-regression of published trials. J Bone Miner Res 34(4):632–642
Malle O, Borgstroem F, Fahrleitner-Pammer A, Svedbom A, Dimai SV, Dimai HP (2019) Mind the gap: incidence of osteoporosis treatment after an osteoporotic fracture - results of the Austrian branch of the International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS). Bone:115071
Solomon DH et al (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res 29(9):1929–1937
Feldstein AC, Nichols G, Orwoll E, et al (2005) The near absence of osteoporosis treatment in older men with fractures. Osteoporos Int 16(8):953–962. https://doi.org/10.1007/s00198-005-1950-0
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, Curtis JR (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30(1):79–92
Alami S, Hervouet L, Poiraudeau S, Briot K, Roux C (2016) Barriers to effective postmenopausal osteoporosis treatment: a qualitative study of patients’ and practitioners’ views. PLoS One 11(6):e0158365
Lindsay BR, Olufade T, Bauer J, Babrowicz J, Hahn R (2016) Patient-reported barriers to osteoporosis therapy. Arch Osteoporos 11(1):19
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E, for the ASBMR Task Force on Secondary Fracture Prevention (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27(10):2039–2046
Funding
Research reported in this publication was supported by the National Institutes of Health under Award Number T32DK007012 (NS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Kenneth Lyles is a Trustee of the National Osteoporosis Foundation, a consultant for Health Stream, Viking, and founder and equity owner of Faculty Connection, LLC and BisCardia, Inc. Nicole Sagalla, Cathleen Colón-Emeric, Richard Sloane, Julie Vognsen, and Richard Lee declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sagalla, N., Colón-Emeric, C., Sloane, R. et al. FRAX without BMD can be used to risk-stratify Veterans who recently sustained a low trauma non-vertebral/non-hip fracture. Osteoporos Int 32, 467–472 (2021). https://doi.org/10.1007/s00198-020-05616-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05616-5