Abstract
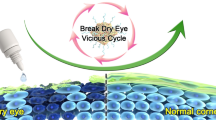
Pseudomonas aeruginosa (P. aeruginosa) keratitis is a sight-threatening and rapidly progressive corneal disease. Neutrophils and neutrophil extracellular traps (NETs) are widely thought to play a vital role in hosts’ immune defenses against bacteria, such as P. aeruginosa. The present study aimed to investigate the dynamics of the formation and the role of NETs in P. aeruginosa keratitis. First, scratched corneas of mice models were treated with 1 × 108 colony-forming units (CFU)/ml of P. aeruginosa suspension or normal saline (NS). Second, after 48 h postinfection, the infected corneas were treated with TobraDex, Tobrex, 0.1% dexamethasone, or NS four times a day, respectively. Clinical examination, hematoxylin and eosin (H&E) staining, immunofluorescence staining, scanning electron microscopy, and bacterial burden testing were performed on the corneas. Tobrex reduced neutrophil infiltration and corneal P. aeruginosa burden. Dexamethasone reduced NETs, bacterial burden, and severe neutrophil infiltration. TobraDex produced a greater reduction in the amount of neutrophils, NETs, and bacterial burden and the results of Tobrex-treated group were between them. These findings corresponded with the clinical findings that TobraDex- and Tobrex-treated mice exhibited slight corneal damage, while dexamethasone-treated mice exhibited very severe corneal damage. Cumulatively, our data suggest that NETs may play a dual role of infection control and corneal damage in P. aeruginosa keratitis. Furthermore, combination treatment targeting NET formation and bacteria may serve as a way of improving the clinical outcomes of bacterial keratitis.








Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CFU:
-
colony-forming units
- H&E:
-
hematoxylin and eosin
- MPO:
-
myeloperoxidase
- NETs:
-
neutrophil extracellular traps
- NS:
-
normal saline
- P. aeruginosa :
-
Pseudomonas aeruginosa
- PBS:
-
phosphate-buffered saline
- PFA:
-
paraformaldehyde
- SEM:
-
scanning electron microscope
References
Pilsczek FH, Salina D, Poon KK et al (2010) A novel mechanism of rapid nuclear neutrophil extracellular trap formation in response to Staphylococcus aureus. J Immunol 185(12):7413–7425
Mori Y, Yamaguchi M, Terao Y et al (2012) alpha-Enolase of Streptococcus pneumoniae induces formation of neutrophil extracellular traps. J Biol Chem 287(13):10472–10481
Pieterse E, Rother N, Yanginlar C et al (2016) Neutrophils discriminate between lipopolysaccharides of different bacterial sources and selectively release neutrophil extracellular traps. Front Immunol 7
Mollerherm H, Neumann A, Schilcher K et al (2015) Yersinia enterocolitica-mediated degradation of neutrophil extracellular traps (NETs). Fems Microbiol Lett 362(23)
Brinkmann V, Reichard U, Goosmann C et al (2004) Neutrophil extracellular traps kill bacteria. Science. 303(5663):1532–1535
Pruchniak MP, Arazna M, Demkow U (2013) Life of neutrophil: from stem cell to neutrophil extracellular trap. Respir Physiol Neurobiol 187(1):68–73
Delgado-Rizo V, Martinez-Guzman MA, Iniguez-Gutierrez L et al (2017) Neutrophil extracellular traps and its implications in inflammation: an overview. Front Immunol 8
Halverson TWR, Wilton M, Poon KKH et al (2015) DNA is an antimicrobial component of neutrophil extracellular traps. Plos Pathogens 11(1):e1004593
Mesa MA, Vasquez G (2013) NETosis. Autoimmune Dis 2013:651497
Cole N, Willcox MD, Fleiszig SM et al (1998) Different strains of Pseudomonas aeruginosa isolated from ocular infections or inflammation display distinct corneal pathologies in an animal model. Curr Eye Res 17(7):730–735
Fleiszig SM, Lee EJ, Wu C et al (1998) Cytotoxic strains of Pseudomonas aeruginosa can damage the intact corneal surface in vitro. CLAO J 24(1):41–47
Borkar DS, Fleiszig SM, Leong C et al (2013) Association between cytotoxic and invasive Pseudomonas aeruginosa and clinical outcomes in bacterial keratitis. JAMA Ophthalmol 131(2):147–153
Murugan N, Malathi J, Umashankar V et al (2016) Unraveling genomic and phenotypic nature of multidrug-resistant (MDR) Pseudomonas aeruginosa VRFPA04 isolated from keratitis patient. Microbiol Res 193:140–149
Yang SS, Hung CT, Li SF et al (2018) Hepatitis B virus-related mortality in rheumatoid arthritis patients undergoing long-term low-dose glucocorticoid treatment: a population-based study. J Formos Med Assoc 117(7):566–571
Tallab RT, Stone DU (2016) Corticosteroids as a therapy for bacterial keratitis: an evidence-based review of ‘who, when and why’. Br J Ophthalmol 100(6):731–735
Czaikoski PG, Mota JM, Nascimento DC et al (2016) Neutrophil extracellular traps induce organ damage during experimental and clinical sepsis. PLoS One 11(2):e0148142
Seeley EJ, Matthay MA, Wolters PJ (2012) Inflection points in sepsis biology: from local defense to systemic organ injury. Am J Physiol Lung Cell Mol Physiol 303(5):L355–L363
Tanaka K, Koike Y, Shimura T et al (2014) In vivo characterization of neutrophil extracellular traps in various organs of a murine sepsis model. PLoS One 9(11):e111888
Wan T, Zhao Y, Fan F et al (2017) Dexamethasone inhibits S. aureus-induced neutrophil extracellular pathogen-killing mechanism, possibly through toll-like receptor regulation. Front Immunol 8:60
Wu TG, Wilhelmus KR, Mitchell BM (2003) Experimental keratomycosis in a mouse model. Invest Ophthalmol Vis Sci 44(1):210–216
Yin H, Qiu P, Wu F et al (2016) Construction of a corneal stromal equivalent with SMILE-derived lenticules and fibrin glue. Sci Rep 6:33848
Fan F, Huang X, Yuan K et al (2020) Glucocorticoids may exacerbate fungal keratitis by increasing fungal aggressivity and inhibiting the formation of neutrophil extracellular traps. Curr Eye Res 45(2):124–133
Jin X, Zhao Y, Zhang F et al (2016) Neutrophil extracellular traps involvement in corneal fungal infection. Mol Vis 22:944–952
Bhongir RK, Kasetty G, Papareddy P et al (2017) DNA-fragmentation is a source of bactericidal activity against Pseudomonas aeruginosa. Biochem J 474(3):411–425
Mulcahy H, Charron-Mazenod L, Lewenza S (2008) Extracellular DNA chelates cations and induces antibiotic resistance in Pseudomonas aeruginosa biofilms. PLoS Pathog 4(11):e1000213
Young RL, Malcolm KC, Kret JE et al (2011) Neutrophil extracellular trap (NET)-mediated killing of Pseudomonas aeruginosa: evidence of acquired resistance within the CF airway, independent of CFTR. PLoS One 6(9):e23637
Wilton M, Halverson TWR, Charron-Mazenod L et al (2018) Secreted phosphatase and deoxyribonuclease are required by Pseudomonas aeruginosa to defend against neutrophil extracellular traps. Infect Immun 86(9)
Jorch SK, Kubes P (2017) An emerging role for neutrophil extracellular traps in noninfectious disease. Nat Med 23(3):279–287
Cortjens B, van Woensel JB, Bem RA (2017) Neutrophil extracellular traps in respiratory disease: guided anti-microbial traps or toxic webs? Paediatr Respir Rev 21:54–61
Jerjomiceva N, Seri H, Vollger L et al (2014) Enrofloxacin enhances the formation of neutrophil extracellular traps in bovine granulocytes. J Innate Immun 6(5):706–712
Bystrzycka W, Manda-Handzlik A, Sieczkowska S et al (2017) Azithromycin and chloramphenicol diminish neutrophil extracellular traps (NETs) release. Int J Mol Sci 18(12)
Manda-Handzlik A, Bystrzycka W, Sieczkowska S et al (2017) Antibiotics modulate the ability of neutrophils to release neutrophil extracellular traps. Adv Exp Med Biol 944:47–52
Bystrzycka W, Moskalik A, Sieczkowska S et al (2016) The effect of clindamycin and amoxicillin on neutrophil extracellular trap (NET) release. Cent Eur J Immunol 41(1):1–5
Funding
This study was funded by the National Natural Science Foundation of China (Grant number: 81270974; 81870624) and major science and technology projects of Zhejiang province (Grant number: 2017C03046).
Author information
Authors and Affiliations
Contributions
BZ, XH, and XJ initially designed the concept of this work, BZ, LZ, YK, and RH collected and analyzed the data, BZ and XJ wrote the manuscript, and BZ and LZ revised the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval
This study was approved by the Ethics Committee of the Second Affiliated Hospital at the School of Medicine, Zhejiang University, China. Procedures involving animals were in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research.
Informed consent
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
Supplementary Figure: Purified human neutrophils were stained using SytoxGreen to label the DNA in vitro. A: Human neutrophils were stimulated by P. aeruginosa. B: Human neutrophils were pretreated with dexamethasone for 30 minutes and then stimulated with P. aeruginosa. C: As controls, human neutrophils were untreated with P. aeruginosa or dexamethasone. Magnification, ×200. (JPG 41 kb)
Rights and permissions
About this article
Cite this article
Zhu, B., Zhang, L., Yuan, K. et al. Neutrophil extracellular traps may have a dual role in Pseudomonas aeruginosa keratitis. Eur J Clin Microbiol Infect Dis 40, 169–180 (2021). https://doi.org/10.1007/s10096-020-04023-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-04023-2