Abstract
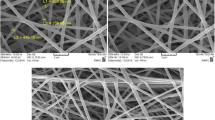
In this study, polycaprolactone (PCL) scaffolds were fabricated via the freeze-casting method. Moreover, the surface of prepared constructs was modified using an oxygen plasma treatment technique for grafting the gelatin in order to improve physicochemical and biological properties. Field emission scanning electron microscopy (FE-SEM) micrographs demonstrated interconnect and unidirectional pore channels. At the same time, the modification procedure showed slight effects on the lamellar microstructure of pores. Fourier transforms infrared (FTIR) spectroscopy determined chemical characterization, which evaluates the effect of the surface treatment on the chemical structure of scaffolds. The wettability of the constructs was investigated by a water drop contact angle and swelling ratio tests. The results illustrated an increment in hydrophilicity after oxygen plasma modification, while the immobilization of gelatin enhanced more the potential of interaction with water molecules. Moreover, the increase in the biodegradation ratio was observed after modification. The in-vitro performance of constructs before and after gelatin immobilization was investigated bt the cell culture assay. Accordingly, modified scaffolds with gelatin support cell attachment and filopodia formation compared with the PCL ones. Besides, the biocompatibility of polymeric matrixes was proved by MTT assay. The results suggest that gelatin grafting on oxygen plasma modified PCL scaffold can be useful in wound healing.

Graphical abstract







Similar content being viewed by others
References
Costa JB, Pereira H, Espregueira-Mendes J, Khang G, Oliveira JM, Reis RL (2017) Tissue engineering in orthopaedic sports medicine: current concepts. J ISAKOS Jt Disord Orthop Sport Med 2:60–66. https://doi.org/10.1136/jisakos-2016-000080
Bose S, Vahabzadeh S, Bandyopadhyay A (2013) Bone tissue engineering using 3D printing. Mater Today 16:496–504. https://doi.org/10.1016/j.mattod.2013.11.017
Zeng H, Huang Y (2018) Basic fibroblast growth factor released from fucoidan-modified chitosan/alginate scaffolds for promoting fibroblasts migration. J Polym Res 25:83. https://doi.org/10.1007/s10965-018-1476-8
Aljohani W, Ullah MW, Li W, Shi L, Zhang X, Yang G (2018) Three-dimensional printing of alginate-gelatin-agar scaffolds using free-form motor assisted microsyringe extrusion system. J Polym Res 25:25. https://doi.org/10.1007/s10965-018-1455-0
Liu L, Zhang Y, Li C, Cao J, He E, Wu X, Wang F, Wang L (2020) Facile preparation PCL/ modified nano ZnO organic-inorganic composite and its application in antibacterial materials. J Polym Res 27:78. https://doi.org/10.1007/s10965-020-02046-z
Deville S (2017) Freezing colloids: observations, principles, control, and use. Springer International Publishing, Cham
Deville S (2010) Freeze-casting of porous biomaterials: structure, properties and opportunities. Materials (Basel) 3:1913–1927. https://doi.org/10.3390/ma3031913
Pourhaghgouy M, Zamanian A (2015) Physical and mechanical properties of the fully interconnected chitosan ice-templated scaffolds. J Appl Polym Sci 132:n/a-n/a. doi: https://doi.org/10.1002/app.41476
Ghorbani F, Zamanian A, Shams A, Shamoosi A, Aidun A (2019) Fabrication and characterisation of super-paramagnetic responsive PLGA–gelatine–magnetite scaffolds with the unidirectional porous structure: a physicochemical, mechanical, and in vitro evaluation. IET Nanobiotechnology 13:860–867. https://doi.org/10.1049/iet-nbt.2018.5305
Ye F, Zhang J, Zhang H, Liu L (2010) Pore structure and mechanical properties in freeze cast porous Si 3N4 composites using polyacrylamide as an addition agent. J Alloys Compd 506:423–427. https://doi.org/10.1016/j.jallcom.2010.07.020
Lloyd C, Besse J, Boyce S (2015) Controlled-rate freezing to regulate the structure of collagen-glycosaminoglycan scaffolds in engineered skin substitutes. J Biomed Mater Res Part B Appl Biomater 103:832–840. https://doi.org/10.1002/jbm.b.33253
Jeong K-H, Park D, Lee Y-C (2017) Polymer-based hydrogel scaffolds for skin tissue engineering applications: a mini-review. J Polym Res 24:112. https://doi.org/10.1007/s10965-017-1278-4
Pattanashetti NA, Viana T, Alves N, Mitchell GR, Kariduraganavar MY (2020) Development of novel 3D scaffolds using BioExtruder by varying the content of hydroxyapatite and silica in PCL matrix for bone tissue engineering. J Polym Res 27:87. https://doi.org/10.1007/s10965-020-02053-0
Sharif S, Ai J, Azami M, Verdi J, Atlasi MA, Shirian S, Samadikuchaksaraei A (2018) Collagen-coated nano-electrospun PCL seeded with human endometrial stem cells for skin tissue engineering applications. J Biomed Mater Res - Part B Appl Biomater 106:1578–1586. https://doi.org/10.1002/jbm.b.33966
Ghosal K, Manakhov A, Zajíčková L, Thomas S (2017) Structural and surface compatibility study of modified electrospun poly(ε-caprolactone) (PCL) composites for skin tissue engineering. AAPS PharmSciTech 18:72–81. https://doi.org/10.1208/s12249-016-0500-8
Pappa AM, Karagkiozaki V, Krol S, Kassavetis S, Konstantinou D, Pitsalidis C, Tzounis L, Pliatsikas N, Logothetidis S (2015) Oxygen-plasma-modified biomimetic nanofibrous scaffolds for enhanced compatibility of cardiovascular implants. Beilstein J Nanotechnol 6:254–262. https://doi.org/10.3762/bjnano.6.24
Jeong L, Yeo IS, Kim HN, Yoon YI, Jang DH, Jung SY, Min BM, Park WH (2009) Plasma-treated silk fibroin nanofibers for skin regeneration. Int J Biol Macromol 44:222–228. https://doi.org/10.1016/j.ijbiomac.2008.12.008
Chen J-P, Chiang Y (2010) Bioactive electrospun silver nanoparticles-containing polyurethane Nanofibers as wound dressings. J Nanosci Nanotechnol 10:7560–7564. https://doi.org/10.1166/jnn.2010.2829
Cheng YY, Du CH, Wu CJ et al (2018) Improving the hydrophilic and antifouling properties of poly(vinyl chloride) membranes by atom transfer radical polymerization grafting of poly(ionic liquid) brushes. Polym Adv Technol 29:623–631. https://doi.org/10.1002/pat.4172
Ghorbani F, Nojehdehyan H, Zamanian A, Gholipourmalekabadi M, Mozafari M (2016) Synthesis, Physico-chemical characteristics and cellular behavior of poly (lactic-co-glycolic acid)/ gelatin Nanofibrous scaffolds for engineering soft connective tissues. Adv Mater Lett 7:163–169. https://doi.org/10.5185/amlett.2016.6003
Ran J, Zeng H, Pathak JL, Jiang P, Bai Y, Yan P, Sun G, Shen X, Tong H, Shi B (2017) Constructing an anisotropic triple-pass tubular framework within a lyophilized porous gelatin scaffold using dexamethasone-loaded functionalized Whatman paper to reinforce its mechanical strength and promote Osteogenesis. Biomacromolecules 18:3788–3801. https://doi.org/10.1021/acs.biomac.7b00673
Ghorbani F, Li D, Ni S, Zhou Y, Yu B (2020) 3D printing of acellular scaffolds for bone defect regeneration: a review. Mater Today Commun 100979:100979. https://doi.org/10.1016/j.mtcomm.2020.100979
Ma Z, He W, Yong T, Ramakrishna S (2005) Grafting of gelatin on electrospun poly(caprolactone) Nanofibers to improve endothelial cell spreading and proliferation and to control cell orientation. Tissue Eng 11:1149–1158. https://doi.org/10.1089/ten.2005.11.1149
Li X, Xie J, Yuan X, Xia Y (2008) Coating electrospun poly (ε-caprolactone) fibers with gelatin and calcium phosphate and their use as biomimetic scaffolds for bone tissue engineering coating. Langmuir 24:14145–14150. https://doi.org/10.1021/la802984a
Tsai M-L, Chen RH (2017) Modifying the molecular weight of chitosan. In: Chitosan based biomaterials, vol 1. Elsevier, pp 135–158
Ghorbani F, Zamanian A, Aidun A (2020) Conductive electrospun polyurethane-polyaniline scaffolds coated with poly(vinyl alcohol)-GPTMS under oxygen plasma surface modification. Mater Today Commun 22:100752. https://doi.org/10.1016/j.mtcomm.2019.100752
Ghorbani F, Zamanian A, Sahranavard M (2019) Mussel-inspired polydopamine-mediated surface modification of freeze-cast poly (ε-caprolactone) scaffolds for bone tissue engineering applications. Biomed Eng / Biomed Tech 65:273–287. https://doi.org/10.1515/bmt-2019-0061
Hosseini Y, Emadi R, Kharaziha M (2017) Surface modification of PCL-diopside fibrous membrane via gelatin immobilization for bone tissue engineering. Mater Chem Phys 194:356–366. https://doi.org/10.1016/j.matchemphys.2017.03.051
Chen H, Xing X, Tan H, Jia Y, Zhou T, Chen Y, Ling Z, Hu X (2017) Covalently antibacterial alginate-chitosan hydrogel dressing integrated gelatin microspheres containing tetracycline hydrochloride for wound healing. Mater Sci Eng C 70:287–295. https://doi.org/10.1016/j.msec.2016.08.086
Sharifi F, Irani S, Zandi M, Soleimani M, Atyabi SM (2016) Comparative of fibroblast and osteoblast cells adhesion on surface modified nanofibrous substrates based on polycaprolactone. Prog Biomater 5:213–222. https://doi.org/10.1007/s40204-016-0059-1
Morro A, Catalina F, Pablos JL, Corrales T, Marin I, Abrusci C (2017) Surface modification of poly(ε-caprolactone) by oxygen plasma for antibacterial applications. Biocompatibility and monitoring of live cells. Eur Polym J 94:405–416. https://doi.org/10.1016/j.eurpolymj.2017.07.027
Sattary M, Khorasani MT, Rafienia M, Rozve HS (2018) Incorporation of nanohydroxyapatite and vitamin D3 into electrospun PCL/gelatin scaffolds: the influence on the physical and chemical properties and cell behavior for bone tissue engineering. Polym Adv Technol 29:451–462. https://doi.org/10.1002/pat.4134
Xia Z, Villa MM, Wei M (2014) A biomimetic collagen–apatite scaffold with a multi-level lamellar structure for bone tissue engineering. J Mater Chem B 2:1998–2007. https://doi.org/10.1039/c3tb21595d
He F, Chen Y, Li J, Lin B, Ouyang Y, Yu B, Xia Y, Yu B, Ye J (2015) Improving bone repair of femoral and radial defects in rabbit by incorporating PRP into PLGA/CPC composite scaffold with unidirectional pore structure. J Biomed Mater Res - Part A 103:1312–1324. https://doi.org/10.1002/jbm.a.35248
Abdullah E, Idris A, Saparon A (2017) Freeze-cast YSZ pore networks: effects of alcohol additives. ARPN J Eng Appl Sci 12:3218–3221. https://doi.org/10.1111/ijlh.12426
Yin K, Divakar P, Hong J, Moodie KL, Rosen JM, Sundback CA, Matthew MK, Wegst UGK (2018) Freeze-cast porous chitosan conduit for peripheral nerve repair. MRS Adv 3:1677–1683. https://doi.org/10.1557/adv.2018.194
Ghorbani F, Zamanian A, Kermanian F, Shamoosi A (2020) A bioinspired 3D shape olibanum-collagen-gelatin scaffolds with tunable porous microstructure for efficient neural tissue regeneration. Biotechnol Prog 36:btpr.2918. https://doi.org/10.1002/btpr.2918
Scotti KL, Dunand DC (2018) Freeze casting – a review of processing, microstructure and properties via the open data repository, FreezeCasting.net. Prog Mater Sci 94:243–305. https://doi.org/10.1016/j.pmatsci.2018.01.001
Stolze C, Janoschka T, Schubert US, Müller FA, Flauder S (2016) Directional solidification with constant ice front velocity in the ice-Templating process. Adv Eng Mater 18:111–120. https://doi.org/10.1002/adem.201500235
Wan Y, Qu X, Lu J, Zhu C, Wan L, Yang J, Bei J, Wang S (2004) Characterization of surface property of poly(lactide-co-glycolide) after oxygen plasma treatment. Biomaterials 25:4777–4783. https://doi.org/10.1016/j.biomaterials.2003.11.051
Shen H, Hu X, Yang F, Bei J, Wang S (2007) Combining oxygen plasma treatment with anchorage of cationized gelatin for enhancing cell affinity of poly(lactide-co-glycolide). Biomaterials 28:4219–4230. https://doi.org/10.1016/j.biomaterials.2007.06.004
Oh SH, Lee JH (2013) Hydrophilization of synthetic biodegradable polymer scaffolds for improved cell/tissue compatibility. Biomed Mater 8:014101. https://doi.org/10.1088/1748-6041/8/1/014101
Adipurnama I, Yang M-C, Ciach T, Butruk-Raszeja B (2017) Surface modification and endothelialization of polyurethane for vascular tissue engineering applications: a review. Biomater Sci 5:22–37. https://doi.org/10.1039/C6BM00618C
Ding Y, Li W, Correia A, Yang Y, Zheng K, Liu D, Schubert DW, Boccaccini AR, Santos HA, Roether JA (2018) Electrospun Polyhydroxybutyrate/poly(ε-caprolactone)/sol–gel-derived silica hybrid scaffolds with drug releasing function for bone tissue engineering applications. ACS Appl Mater Interfaces 10:14540–14548. https://doi.org/10.1021/acsami.8b02656
Park SA, Lee SJ, Seok JM, Lee JH, Kim WD, Kwon IK (2018) Fabrication of 3D printed PCL/PEG Polyblend scaffold using rapid prototyping system for bone tissue engineering application. J Bionic Eng 15:435–442. https://doi.org/10.1007/s42235-018-0034-8
Siri S, Wadbua P, Amornkitbamrung V, Kampa N, Maensiri S (2010) Surface modification of electrospun PCL scaffolds by plasma treatment and addition of adhesive protein to promote fibroblast cell adhesion. Mater Sci Technol 26:1292–1297. https://doi.org/10.1179/026708310x12798718274070
Park JU, Jeong SH, Song EH, Song J, Kim HE, Kim S (2018) Acceleration of the healing process of full-thickness wounds using hydrophilic chitosan–silica hybrid sponge in a porcine model. J Biomater Appl 32:1011–1023. https://doi.org/10.1177/0885328217751246
Oyane A, Uchida M, Yokoyama Y, Choong C, Triffitt J, Ito A (2005) Simple surface modification of poly(ε-caprolactone) to induce its apatite-forming ability. J Biomed Mater Res Part A 75A:138–145. https://doi.org/10.1002/jbm.a.30397
Aisenbrey EA, Tomaschke A, Kleinjan E, Muralidharan A, Pascual-Garrido C, McLeod RR, Ferguson VL, Bryant SJ (2018) A Stereolithography-based 3D printed hybrid scaffold for in situ cartilage defect repair. Macromol Biosci 18:1700267. https://doi.org/10.1002/mabi.201700267
Xiang P, Wang SS, He M, Han YH, Zhou ZH, Chen DL, Li M, Ma LQ (2018) The in vitro and in vivo biocompatibility evaluation of electrospun recombinant spider silk protein/PCL/gelatin for small caliber vascular tissue engineering scaffolds. Colloids Surfaces B Biointerfaces 163:19–28. https://doi.org/10.1016/j.colsurfb.2017.12.020
Ghorbani F, Zamanian A (2018) Oxygen-plasma treatment-induced surface engineering of biomimetic polyurethane nanofibrous scaffolds for gelatin-heparin immobilization. E-polymers 18:275–285. https://doi.org/10.1515/epoly-2017-0185
Liu Y, Ma L, Gao C (2012) Facile fabrication of the glutaraldehyde cross-linked collagen / chitosan porous scaffold for skin tissue engineering. Mater Sci Eng C 32:2361–2366. https://doi.org/10.1016/j.msec.2012.07.008
Deville S, Saiz E, Tomsia AP (2006) Freeze casting of hydroxyapatite scaffolds for bone tissue engineering. Biomaterials 27:5480–5489. https://doi.org/10.1016/j.biomaterials.2006.06.028
Zhu Y, Gao C, He T, Shen J (2004) Endothelium regeneration on luminal surface of polyurethane vascular scaffold modified with diamine and covalently grafted with gelatin. Biomaterials 25:423–430. https://doi.org/10.1016/S0142-9612(03)00549-0
Pedram Rad Z, Mokhtari J, Abbasi M (2018) Fabrication and characterization of PCL/zein/gum arabic electrospun nanocomposite scaffold for skin tissue engineering. Mater Sci Eng C 93:356–366. https://doi.org/10.1016/j.msec.2018.08.010
Ramanathan G, Singaravelu S, Muthukumar T, Thyagarajan S, Perumal PT, Sivagnanam UT (2017) Design and characterization of 3D hybrid collagen matrixes as a dermal substitute in skin tissue engineering. Mater Sci Eng C 72:359–370. https://doi.org/10.1016/j.msec.2016.11.095
Hajiali F, Tajbakhsh S, Shojaei A (2018) Fabrication and properties of polycaprolactone composites containing calcium phosphate-based ceramics and bioactive glasses in bone tissue engineering: A review. Polym Rev 58:164–207. https://doi.org/10.1080/15583724.2017.1332640
Shokrollahi P, Mehmanchi M, Atai M, Omidian H, Shokrolahi F (2014) Effect of interface on mechanical properties and biodegradation of PCL HAp supramolecular nano-composites. J Mater Sci Mater Med 25:23–35. https://doi.org/10.1007/s10856-013-5039-6
Mahmoud AA, Salama AH (2016) Norfloxacin-loaded collagen/chitosan scaffolds for skin reconstruction: preparation, evaluation and in-vivo wound healing assessment. Eur J Pharm Sci 83:155–165. https://doi.org/10.1016/j.ejps.2015.12.026
Kempf M, Miyamura Y, Liu PY, Chen ACH, Nakamura H, Shimizu H, Tabata Y, Kimble RM, McMillan JR (2011) A denatured collagen microfiber scaffold seeded with human fibroblasts and keratinocytes for skin grafting. Biomaterials 32:4782–4792. https://doi.org/10.1016/j.biomaterials.2011.03.023
Ma L (2003) Collagen/chitosan porous scaffolds with improved biostability for skin tissue engineering. Biomaterials 24:4833–4841. https://doi.org/10.1016/S0142-9612(03)00374-0
Adekogbe I, Ghanem A (2005) Fabrication and characterization of DTBP-crosslinked chitosan scaffolds for skin tissue engineering. Biomaterials 26:7241–7250. https://doi.org/10.1016/j.biomaterials.2005.05.043
Zhu T, Jiang J, Zhao J, Chen S, Yan X (2019) Regulating preparation of functional alginate-chitosan three-dimensional scaffold for skin tissue engineering. Int J Nanomedicine 14:8891–8903. https://doi.org/10.2147/IJN.S210329
Yan D, Jones J, Yuan XY, Xu XH, Sheng J, Lee JCM, Ma GQ, Yu QS (2013) Plasma treatment of electrospun PCL random nanofiber meshes (NFMs) for biological property improvement. J Biomed Mater Res - Part A 101 A:963–972. https://doi.org/10.1002/jbm.a.34398
Mahnama H, Dadbin S, Frounchi M, Rajabi S (2017) Preparation of biodegradable gelatin/PVA porous scaffolds for skin regeneration. Artif Cells, Nanomedicine Biotechnol 45:928–935. https://doi.org/10.1080/21691401.2016.1193025
Hosseini V, Mirrahimi M, Shakeri-Zadeh A, Koosha F, Ghalandari B, Maleki S, Komeili A, Kamrava SK (2018) Multimodal cancer cell therapy using au@Fe2O3 core–shell nanoparticles in combination with photo-thermo-radiotherapy. Photodiagn Photodyn Ther 24:129–135. https://doi.org/10.1016/j.pdpdt.2018.08.003
Palamà IE, Arcadio V, D’Amone S, Biasiucci M, Gigli G, Cortese B (2017) Therapeutic PCL scaffold for reparation of resected osteosarcoma defect. Sci Rep 7:1–12. https://doi.org/10.1038/s41598-017-12824-3
Zeinizade E, Tabei M, Shakeri-Zadeh A, Ghaznavi H, Attaran N, Komeili A, Ghalandari B, Maleki S, Kamrava SK (2018) Selective apoptosis induction in cancer cells using folate-conjugated gold nanoparticles and controlling the laser irradiation conditions. Artif Cells, Nanomedicine, Biotechnol 46:1026–1038. https://doi.org/10.1080/21691401.2018.1443116
Du H, Zheng Y, He W et al (2018) A novel expandable porous composite based on acetalized polyvinyl alcohol and calcium sulfate used for injectable bone repair materials. Compos Sci Technol 157:10–20. https://doi.org/10.1016/j.compscitech.2018.01.014
Ghorbani F, Zamanian A, Behnamghader A, Daliri-Joupari M (2019) Bone-like hydroxyapatite mineralization on the bio-inspired PDA nanoparticles using microwave irradiation. Surfaces and Interfaces 15:38–42. https://doi.org/10.1016/j.surfin.2019.01.007
Yildirim ED, Ayan H, Vasilets VN, Fridman A, Guceri S, Sun W (2008) Effect of dielectric barrier discharge plasma on the attachment and proliferation of osteoblasts cultured over poly(ε-caprolactone) scaffolds. Plasma Process Polym 5:58–66. https://doi.org/10.1002/ppap.200700041
Kuttappan S, Mathew D, Nair MB (2016) Biomimetic composite scaffolds containing bioceramics and collagen/gelatin for bone tissue engineering - a mini review. Int J Biol Macromol 93:1390–1401. https://doi.org/10.1016/j.ijbiomac.2016.06.043
Jiang YC, Jiang L, Huang A, Wang XF, Li Q, Turng LS (2017) Electrospun polycaprolactone/gelatin composites with enhanced cell–matrix interactions as blood vessel endothelial layer scaffolds. Mater Sci Eng C 71:901–908. https://doi.org/10.1016/j.msec.2016.10.083
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghorbani, F., Sahranavard, M. & Zamanian, A. Immobilization of gelatin on the oxygen plasma-modified surface of polycaprolactone scaffolds with tunable pore structure for skin tissue engineering. J Polym Res 27, 281 (2020). https://doi.org/10.1007/s10965-020-02263-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10965-020-02263-6