Abstract
Purpose
In patients with open growth plates, the direction of tunneling that avoids distal femoral physis (DFP) damage in anatomic reconstructions of the medial patellofemoral ligament (MPFL) has been a topic of discussion. The objective of this study was to determine the ideal orientation for anatomic reconstructions of MPFL tunneling that minimized DFP damage while avoiding breaching the intercondylar notch.
Methods
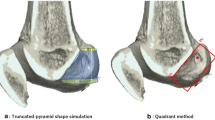
Eighty magnetic resonance images of patients aged 10 through 17 were obtained, randomly sampled from the institutional database. A de novo software was developed to obtain 3D models of the distal femur and DFP. In each model, the anatomical insertion point of the MPFL was determined as defined by Stephen. A 20-mm-depth drilling was simulated, starting from the insertion point at every possible angle within a 90° cone using 5-, 6- and 7-mm drills. Physeal damage for each pair of angles and each drill size was determined. Damage was expressed as a percentage of total physis volume. Statistical analysis was conducted using Student’s t test and one-way ANOVA.
Results
Maximum physeal damage (5.35% [4.47–6.24]) was obtained with the 7-mm drill when drilling 3° cephalic and 15° posterior from insertion without differences between sexes (n.s.). Minimal physeal damage (0.22% [0.07–0.37]) was obtained using the 5-mm drill aimed 45° distal and 0° anteroposterior, not affected by sex (n.s.). Considering intra-articular drilling avoidance, the safest zone was obtained when aiming 30°–40° distal and 5°–35° anterior, regardless of sex.
Conclusion
Ideal femoral tunnel orientation, avoiding physeal damage and breaching of the intercondylar notch, was obtained when aiming 30°–40° distal and 5°–35° anterior, regardless of sex. This area is a safe zone that allows anatomic MPFL reconstruction of patients with an open physis.






Similar content being viewed by others
References
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10(3):215–220
Askenberger M, Ekström W, Finnbogason T, Janarv PM (2014) Occult intra-articular knee injuries in children with hemarthrosis. Am J Sports Med 42(7):1600–1606
Arendt EA, Fithian DC, Cohen E (2002) Current concepts of lateral patella dislocation. Clin Sports Med 21(3):499–519
Bicos J, Fulkerson JP, Amis A (2007) Current concepts review: the medial patellofemoral ligament. Am J Sports Med 35(3):484–492
Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ (2010) Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med 38(11):2248–2254
Chouteau J, Benareau I, Testa R, Fessy MH, Lerat JL, Moyen B (2008) Comparative study of knee anterior cruciate ligament reconstruction with or without fluoroscopic assistance: a prospective study of 73 cases. Arch Orthop Trauma Surg 128(9):945–950
Elias JJ, Cosgarea AJ (2006) Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 34(9):1478–1485
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32(5):1114–1121
Ford LT, Key JA (1956) A study of experimental trauma to the distal femoral epiphysis in rabbits. J Bone Jt Surg A 38:84–92
Garcés GL, Mugica-Garay I, López-González Coviella N, Guerado E (1994) Growth-plate modifications after drilling. J Pediatr Orthop 14(2):225–228
Greenrod W, Cox J, Astori I, Baulch J, Williams J (2013) A magnetic resonance imaging study of the significance of the distal femoral physis during medial patellofemoral ligament reconstruction. Orthop J Sports Med 1(4):1–4
Hallgren KA (2012) Computing inter-rater reliability for observational data: an overview and tutorial. Tutor Quant Methods Psychol 8(1):23–34
Hennrikus W, Pylawka T (2013) Patellofemoral instability in skeletally immature athletes. Instr Course Lect 62:445–453
Hufner T, Geerling J, Oldag G, Richter M, Kfuri M Jr, Pohlemann T, Krettek C (2005) Accuracy study of computer-assisted drilling: the effect of bone density, drill bit characteristics, and use of a mechanical guide. J Orthop Trauma 19(5):317–322
Huston KL, Okoroafor UC, Kaar SG, Wentt CL, Saluan P, Farrow LD (2017) Evaluation of the Schöttle technique in the pediatric knee. Orthop J Sports Med 5(11):1–5
Janarv PM, Wikström B, Hirsch G (1998) The influence of transphyseal drilling and tendon grafting on bone growth: an experimental study in the rabbit. J Pediatr Orthop 18(2):149–154
Lewallen LW, McIntosh AL, Dahm DL (2013) Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 41(3):575–581
Liu RW, Armstrong DG, Levine AD, Gilmore A, Thompson GH, Cooperman DR (2013) An anatomic study of the distal femoral epiphysis. J Pediatr Orthop 33(7):743–749
Mäkelä EA, Vainionpää S, Vihtonen K, Mero M, Rokkanen P (1988) The effect of trauma to the lower femoral epiphyseal plate. An experimental study in rabbits. J Bone Jt Surg Br 70(2):187–191
Monllau JC, Masferrer-Pino À, Ginovart G, Pérez-Prieto D, Gelber PE, Sanchis-Alfonso V (2017) Clinical and radiological outcomes after a quasi-anatomical reconstruction of medial patellofemoral ligament with gracilis tendon autograft. Knee Surg Sports Traumatol Arthrosc 25(8):2453–2459
Nelitz M, Dreyhaupt J, Reichel H, Woelfle J, Lippacher S (2013) Anatomic reconstruction of the medial patellofemoral ligament in children and adolescents with open growth plates: surgical technique and clinical outcome. Am J Sports Med 41(1):58–63
Nguyen CV, Farrow LD, Liu RW, Gilmore A (2017) Safe drilling paths in the distal femoral epiphysis for pediatric medial patellofemoral ligament reconstruction. Am J Sports Med 45(5):1085–1089
Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14(4):513–515
Pérez-Prieto D, Capurro B, Gelber PE, Ginovart G, Reina F, Sanchis-Alfonso V, Monllau JC (2017) The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 25(8):2420–2423
Sallay PI, Poggi J, Speer KP, Garrett WE (1996) Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med 24(1):52–60
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35(5):801–804
Seil R, Pape D, Kohn D (2008) The risk of growth changes during transphyseal drilling in sheep with open physes. Arthroscopy 24(7):824–833
Seitlinger G, Moroder P, Fink C, Wierer G (2017) Acquired femoral flexion deformity due to physeal injury during medial patellofemoral ligament reconstruction. Knee 24(3):680–685
Shea KG, Martinson WD, Cannamela PC, Richmond CG, Fabricant PD, Anderson AF, Polousky JD, Ganley TJ (2018) Variation in the medial patellofemoral ligament origin in the skeletally immature knee: an anatomic study. Am J Sports Med 46(2):363–369
Shea KG, Polousky JD, Jacobs JC Jr, Ganley TJ, Aoki SK, Grimm NL, Parikh SN (2014) The relationship of the femoral physis and the medial patellofemoral ligament in children: a cadaveric study. J Pediatr Orthop 34(8):808–813
Smirk C, Morris H (2003) The anatomy and reconstruction of the medial patellofemoral ligament. Knee 10(3):221–227
Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA (2012) The medial patellofemoral ligament: location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med 40(8):1871–1879
Stupay KL, Swart E, Shubin Stein BE (2015) Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: a systematic review. Arthroscopy 31(7):1372–1380
Tscholl PM, Ernstbrunner L, Pedrazzoli L, Fucentese SF (2018) The relationship of femoral tunnel positioning in medial patellofemoral ligament reconstruction on clinical outcome and postoperative complications. Arthroscopy 34(8):2410–2416
Vavken P, Wimmer MD, Camathias C, Quidde J, Valderrabano V, Pagenstert G (2013) Treating patella instability in skeletally immature patients. Arthroscopy 29(8):1410–1422
Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, Bedi A (2016) An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Jt Surg Am 98(5):417–427
Weeks KD 3rd, Fabricant PD, Ladenhauf HN, Green DW (2012) Surgical options for patellar stabilization in the skeletally immature patient. Sports Med Arthrosc Rev 20(3):194–202
Acknowledgements
We would like to thank Fernando Marin, Anselmo Alegría, Matías Rojas, Jorge López, and José Tomás Ossa for their contribution in data recollection. We also thank Catalina Vidal for her contribution in statistical analysis and manuscript overview. Finally, we would like to thank Rafael Vega, Luis Irribarra, Julio Espinosa, and Raimundo Vial for their cooperation in our research team.
Funding
This study did not require funding.
Author information
Authors and Affiliations
Contributions
SI: conception and design, analysis and interpretation of data; drafting the manuscript and revising it critically for important intellectual content; final approval of the version to be published; agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; PB: conception and design, analysis and interpretation of data; drafting the manuscript and revising it critically for important intellectual content; final approval of the version to be published; agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; FF: acquisition of data, analysis and interpretation of data; revising the manuscript critically for important intellectual content; final approval of the version to be published; agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; TF: acquisition of data, analysis and interpretation of data; revising the manuscript critically for important intellectual content; final approval of the version to be published; agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; MJT: conception and design, analysis and interpretation of data; revising the manuscript critically for important intellectual content; final approval of the version to be published; agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; MJL: acquisition of data, analysis and interpretation of data; revising the manuscript critically for important intellectual content; final approval of the version to be published; agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; MO: conception and design, analysis and interpretation of data; revising the manuscript critically for important intellectual content; final approval of the version to be published; agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
There are no authors’ disclosures or conflicts of interest.
Ethical approval
Institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Irarrázaval, S., Besa, P., Fernández, F. et al. Anterior and distal tunnel orientation for anatomic reconstruction of the medial patellofemoral ligament is safer in patients with open growth plates. Knee Surg Sports Traumatol Arthrosc 29, 1822–1829 (2021). https://doi.org/10.1007/s00167-020-06229-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06229-5