Abstract
Nootropics are drugs used to either treat or benefit cognition deficits. Among this class, methylphenidate is a popular agent, which acts through indirect dopaminergic and noradrenergic agonism and, therefore, is proposed to enhance performance in catecholamine-dependent cognitive domains such as attention, memory and prefrontal cortex-dependent executive functions. However, investigation into the efficacy of methylphenidate as a cognitive enhancer has yielded variable results across all domains, leading to debate within the scientific community surrounding its off-label use in healthy individuals seeking scholaristic benefit or increased productivity. Through analysis of experimental data and methodological evaluation, it is apparent that there are dose-, task- and domain-dependent considerations surrounding the use of methylphenidate in healthy individuals, whereby tailored dose administration is likely to provide benefit on an individual basis dependent on the domain of cognition in which benefit is required. Additionally, it is apparent that there are subjective effects of methylphenidate, which may increase user productivity irrespective of cognitive benefit. Whilst there is not extensive study in healthy older adults, it is plausible that there are dose-dependent benefits to methylphenidate in older adults in selective cognitive domains that might improve quality of life and reduce fall risk. Methylphenidate appears to produce dose-dependent benefits to individuals with attention-deficit/hyperactivity disorder, but the evidence for benefit in Parkinson’s disease and schizophrenia is inconclusive. As with any off-label use of pharmacological agents, and especially regarding drugs with neuromodulatory effects, there are inherent safety concerns; epidemiological and experimental evidence suggests there are sympathomimetic, cardiovascular and addictive considerations, which might further restrict their use within certain demographics.
Similar content being viewed by others
References
Froestl W, Muhs A, Pfeifer A. Cognitive enhancers (nootropics). Part 1: drugs interacting with receptors. Update 2014. J Alzheimers Dis. 2014;41(4):961–1019. https://doi.org/10.3233/jad-140228.
Sahakian B, Morein-Zamir S. Professor’s little helper. Nature. 2007;450(7173):1157–9. https://doi.org/10.1038/4501157a.
Husain M, Mehta MA. Cognitive enhancement by drugs in health and disease. Trends Cogn Sci. 2011;15(1):28–36. https://doi.org/10.1016/j.tics.2010.11.002.
Fins JJ. Mind wars: brain research and national defense. JAMA. 2007;297(12):1379. https://doi.org/10.1001/jama.297.12.1382.
Greely H, Sahakian B, Harris J, et al. Towards responsible use of cognitive-enhancing drugs by the healthy. Nanotechnol Brain Future. 2013. https://doi.org/10.1007/978-94-007-1787-9_14.
Smith ME, Farah MJ. Are prescription stimulants “smart pills”? The epidemiology and cognitive neuroscience of prescription stimulant use by normal healthy individuals. Psychol Bull. 2011;137(5):717–41. https://doi.org/10.1037/a0023825.
Maher B. Poll results: look who’s doping. Nature. 2008;452(7188):674–5. https://doi.org/10.1038/452674a.
Ragan CI, Bard I, Singh I. What should we do about student use of cognitive enhancers? An analysis of current evidence. Neuropharmacology. 2013;64:588–95. https://doi.org/10.1016/j.neuropharm.2012.06.016.
McCabe SE, Knight JR, Teter CJ, Wechsler H. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100(1):96–106. https://doi.org/10.1111/j.1360-0443.2005.00944.x.
Ungerstedt U. Stereotaxic mapping of the monoamine pathways in the rat brain. Acta Physiol Scand Suppl. 1971;367:1–48. https://doi.org/10.1111/j.1365-201X.1971.tb10998.x.
Diamond A. Executive functions. Annu Rev Psychol. 2013;64(1):135–68. https://doi.org/10.1146/annurev-psych-113011-143750.
Goldman-Rakic PS. Cellular basis of working memory. Neuron. 1995;14(3):477–85. https://doi.org/10.1016/0896-6273(95)90304-6.
Sawaguchi T, Goldman-Rakic PS. D1 dopamine receptors in prefrontal cortex: involvement in working memory. Science. 1991;251(4996):947–50. https://doi.org/10.1126/science.1825731.
Brozoski T, Brown R, Rosvold H, Goldman P. Cognitive deficit caused by regional depletion of dopamine in prefrontal cortex of rhesus monkey. Science. 1979;205(4409):929–32. https://doi.org/10.1126/science.112679.
Murphy BL, Arnsten AFT, Goldman-Rakic PS, Roth RH. Increased dopamine turnover in the prefrontal cortex impairs spatial working memory performance in rats and monkeys. Proc Natl Acad Sci USA. 1996;3(3):1325–9. https://doi.org/10.1073/pnas.93.3.1325.
Zahrt J, Taylor JR, Mathew RG, Arnsten AF. Supranormal stimulation of D1 dopamine receptors in the rodent prefrontal cortex impairs spatial working memory performance. J Neurosci. 1997;17(21):8528–35.
Kroener S, Chandler JL, Phillips PEM, Seamans JK. Dopamine modulates persistent synaptic activity and enhances the signal-to-noise ratio in the prefrontal cortex. PLoS One. 2009;4(8):e6507. https://doi.org/10.1371/journal.pone.0006507.
Cools R, D’Esposito M. Inverted-U-shaped dopamine actions on human working memory and cognitive control. Biol Psychiatry. 2011;9(12):e113–25. https://doi.org/10.1016/j.biopsych.2011.03.028.
Solanto MV. Neuropsychopharmacological mechanisms of stimulant drug action in attention-deficit hyperactivity disorder: a review and integration. Behav Brain Res. 1998;94(1):127–52. https://doi.org/10.1016/S0166-4328(97)00175-7.
Foote SL, Aston-Jones G, Bloom FE. Impulse activity of locus coeruleus neurons in awake rats and monkeys is a function of sensory stimulation and arousal. Proc Natl Acad Sci USA. 1980;77(5):3033–7. https://doi.org/10.1073/pnas.77.5.3033.
Aston-Jones G, Bloom FE. Activity of norepinephrine-containing locus coeruleus neurons in behaving rats anticipates fluctuations in the sleep-waking cycle. J Neurosci. 1981;1(8):876–86. https://doi.org/10.1523/jneurosci.4553-14.2015.
Arnsten AF, Goldman-Rakic PS. Alpha 2-adrenergic mechanisms in prefrontal cortex associated with cognitive decline in aged nonhuman primates. Science. 1985;230(4731):1273–6. https://doi.org/10.1126/science.2999977.
Langer SZ. Presynaptic regulation of catecholamine release. Biochem Pharmacol. 1974;23(13):1793–800. https://doi.org/10.1016/0006-2952(74)90187-7.
Cai JX, Ma Y, Xu L, Hu X. Reserpine impairs spatial working memory performance in monkeys: reversal by the α2-adrenergic agonist clonidine. Brain Res. 1993;614(1–2):191–6. https://doi.org/10.1016/0006-8993(93)91034-p.
Birnbaum S, Gobeske KT, Auerbach J, Taylor JR, Arnsten AFT. A role for norepinephrine in stress-induced cognitive deficits: α-1-adrenoceptor mediation in the prefrontal cortex. Biol Psychiatry. 1999;46(9):1266–74. https://doi.org/10.1016/S0006-3223(99)00138-9.
Ramos BP, Colgan L, Nou E, Ovadia S, Wilson SR, Arnsten AFT. The beta-1 adrenergic antagonist, betaxolol, improves working memory performance in rats and monkeys. Biol Psychiatry. 2005;58(11):894–900. https://doi.org/10.1016/j.biopsych.2005.05.022.
Scahill L, Carroll D, Burke K. Methylphenidate: mechanism of action and clinical update. J Child Adolesc Psychiatr Nurs. 2004;17(2):85–6. https://doi.org/10.1111/j.1744-6171.2004.00085.x.
Volkow ND, Wang G, Fowler JS, et al. Therapeutic doses of oral methylphenidate significantly increase extracellular dopamine in the human brain. J Neurosci. 2001;21(2):RC121. https://doi.org/10.1523/jneurosci.21-02-j0001.2001.
Wall SC, Gu H, Rudnick G. Biogenic amine flux mediated by cloned transporters stably expressed in cultured cell lines: amphetamine specificity for inhibition and efflux. Mol Pharmacol. 1995;47:544–50.
Cahill L, McGaugh JL. A novel demonstration of enhanced memory associated with emotional arousal. Conscious Cogn. 1995;4(4):410–21. https://doi.org/10.1006/ccog.1995.1048.
Brignell CM, Rosenthal J, Curran HV. Pharmacological manipulations of arousal and memory for emotional material: effects of a single dose of methylphenidate or lorazepam. J Psychopharmacol. 2007;21(7):673–83. https://doi.org/10.1177/0269881107077351.
Camp-Bruno JA, Herting RL. Cognitive effects of milacemide and methylphenidate in healthy young adults. Psychopharmacology (Berl). 1994;115(1–2):46–52. https://doi.org/10.1007/BF02244750.
Linssen AMW, Sambeth A, Vuurman EFPM, Riedel WJ. Cognitive effects of methylphenidate in healthy volunteers: a review of single dose studies. Int J Neuropsychopharmacol. 2014;17(6):961–77. https://doi.org/10.1017/S1461145713001594.
Klinge C, Shuttleworth C, Muglia P, Nobre AC, Harmer CJ, Murphy SE. Methylphenidate enhances implicit learning in healthy adults. J Psychopharmacol. 2018;32(1):70–80. https://doi.org/10.1177/0269881117731472.
Dodds CM, Müller U, Clark L, Van Loon A, Cools R, Robbins TW. Methylphenidate has differential effects on blood oxygenation level-dependent signal related to cognitive subprocesses of reversal learning. J Neurosci. 2008;28(23):5976–82. https://doi.org/10.1523/JNEUROSCI.1153-08.2008.
Wetzel CD, Squire LR, Janowsky DS. Methylphenidate impairs learning and memory in normal adults. Behav Neural Biol. 1981;31(4):413–24. https://doi.org/10.1016/S0163-1047(81)91481-3.
Clatworthy PL, Lewis SJG, Brichard L, et al. Dopamine release in dissociable striatal subregions predicts the different effects of oral methylphenidate on reversal learning and spatial working memory. J Neurosci. 2009;29(15):4690–6. https://doi.org/10.1523/JNEUROSCI.3266-08.2009.
Divac I, Rosvold HE, Szwarcbart MK. Behavioral effects of selective ablation of the caudate nucleus. J Comp Physiol Psychol. 1967;63(2):184–90. https://doi.org/10.1037/h0024348.
Linssen AMW, Vuurman EFPM, Sambeth A, Riedel WJ. Methylphenidate produces selective enhancement of declarative memory consolidation in healthy volunteers. Psychopharmacology (Berl). 2012;221(4):611–9. https://doi.org/10.1007/s00213-011-2605-9.
Bray CL, Cahill KS, Oshier JT, et al. Methylphenidate does not improve cognitive function in healthy sleep-deprived young adults. J Investig Med. 2004;52(3):192–201.
Baddeley A. Working memory. Science. 1992;255(5044):556–9. https://doi.org/10.4249/scholarpedia.3015.
Mehta MA, Owen AM, Sahakian BJ, Mavaddat N, Pickard JD, Robbins TW. Methylphenidate enhances working memory by modulating discrete frontal and parietal lobe regions in the human brain. J Neurosci. 2000;20(6):RC65.
Ramasubbu R, Singh H, Zhu H, Dunn JF. Methylphenidate-mediated reduction in prefrontal hemodynamic responses to working memory task: a functional near-infrared spectroscopy study. Hum Psychopharmacol Clin Exp. 2012;27(6):615–21. https://doi.org/10.1002/hup.2258.
Cooper NJ, Keage H, Hermens D, et al. The dose-dependent effect of methylphenidate on performance, cognition and psychophysiology. J Integr Neurosci. 2005;4(1):123–44. https://doi.org/10.1142/S0219635205000744.
Strauss J, Lewis JL, Klorman R, Peloquin L-J, Perlmutter RA, Salzman LF. Effects of methylphenidate on young adults’ performance and event-related potentials in a vigilance and a paired-associates learning test. Psychophysiology. 1984;21(6):609–21. https://doi.org/10.1111/j.1469-8986.1984.tb00247.x.
Tomasi D, Volkow ND, Wang GJ, et al. Methylphenidate enhances brain activation and deactivation responses to visual attention and working memory tasks in healthy controls. NeuroImage. 2011;54(4):3101–10. https://doi.org/10.1016/j.neuroimage.2010.10.060.
Agay N, Yechiam E, Carmel Z, Levkovitz Y. Non-specific effects of methylphenidate (Ritalin) on cognitive ability and decision-making of ADHD and healthy adults. Psychopharmacology (Berl). 2010;210(4):511–9. https://doi.org/10.1007/s00213-010-1853-4.
Elliott R, Sahakian BJ, Matthews K, Bannerjea A, Rimmer J, Robbins TW. Effects of methylphenidate on spatial working memory and planning in healthy young adults. Psychopharmacology (Berl). 1997;131(2):196–206. https://doi.org/10.1007/s002130050284.
Drijgers RL, Verhey FRJ, Tissingh G, Van Domburg PHMF, Aalten P, Leentjens AFG. The role of the dopaminergic system in mood, motivation and cognition in Parkinson’s disease: a double blind randomized placebo-controlled experimental challenge with pramipexole and methylphenidate. J Neurol Sci. 2012;320(1–2):121–6. https://doi.org/10.1016/j.jns.2012.07.015.
Batistela S, Bueno OFA, Vaz LJ, Galduróz JCF. Methylphenidate as a cognitive enhancer in healthy young people. Dement Neuropsychol. 2016;10(2):134–42. https://doi.org/10.1590/s1980-5764-2016dn1002009.
Turner DC, Robbins TW, Clark L, Aron AR, Dowson J, Sahakian BJ. Relative lack of cognitive effects of methylphenidate in elderly male volunteers. Psychopharmacology (Berl). 2003;168(4):455–64. https://doi.org/10.1007/s00213-003-1457-.3.
Vossel S, Geng JJ, Fink GR. Dorsal and ventral attention systems: distinct neural circuits but collaborative roles. Neuroscientist. 2014;20(2):150–9. https://doi.org/10.1177/1073858413494269.
Ter Huurne N, Fallon SJ, Van Schouwenburg M, et al. Methylphenidate alters selective attention by amplifying salience. Psychopharmacology (Berl). 2015;232(23):4317–23. https://doi.org/10.1007/s00213-015-4059-y.
Oken BS, Kishiyama SS, Salinsky MC. Pharmacologically induced changes in arousal: effects on behavioral and electrophysiologic measures of alertness and attention. Electroencephalogr Clin Neurophysiol. 1995;95(5):359–71. https://doi.org/10.1016/0013-4694(95)00124-H.
Finke K, Dodds CM, Bublak P, et al. Effects of modafinil and methylphenidate on visual attention capacity: a TVA-based study. Psychopharmacology (Berl). 2010;210(3):317–29. https://doi.org/10.1007/s00213-010-1823-x.
Cools R, Gibbs SE, Miyakawa A, Jagust W, D’Esposito M. Working memory capacity predicts dopamine synthesis capacity in the human striatum. J Neurosci. 2008;28(5):1208–12. https://doi.org/10.1523/JNEUROSCI.4475-07.2008.
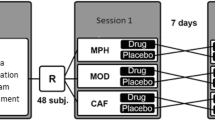
Franke AG, Gränsmark P, Agricola A, et al. Methylphenidate, modafinil, and caffeine for cognitive enhancement in chess: a double-blind, randomised controlled trial. Eur Neuropsychopharmacol. 2017;27(3):248–60. https://doi.org/10.1016/j.euroneuro.2017.01.006.
Volkow ND, Fowler JS, Wang GJ, et al. Methylphenidate decreased the amount of glucose needed by the brain to perform a cognitive task. PLoS One. 2008;3(4):e2017. https://doi.org/10.1371/journal.pone.0002017.
Baas M, Boot N, van Gaal S, de Dreu CKW, Cools R. Methylphenidate does not affect convergent and divergent creative processes in healthy adults. NeuroImage. 2020. https://doi.org/10.1016/j.neuroimage.2019.116279.
Babkoff H, Kelly TL, Matteson LT, et al. Pemoline and methylphenidate: interaction with mood, sleepiness, and cognitive performance during 64 hours of sleep deprivation. Mil Psychol. 1992. https://doi.org/10.1207/s15327876mp0404_3.
Roehrs T, Papineau K, Rosenthal L, Roth T. Sleepiness and the reinforcing and subjective effects of methylphenidate. Exp Clin Psychopharmacol. 1999;7(2):145–50. https://doi.org/10.1037/1064-1297.7.2.145.
Volkow ND, Wang GJ, Fowler JS, et al. Evidence that methylphenidate enhances the saliency of a mathematical task by increasing dopamine in the human brain. Am J Psychiatry. 2004. https://doi.org/10.1176/appi.ajp.161.7.1173.
Flatt T. A new definition of aging? Front Genet. 2012. https://doi.org/10.3389/fgene.2012.00148.
Harada CN, Natelson Love MC, Triebel KL. Normal cognitive aging. Clin Geriatr Med. 2013;29(4):737–52. https://doi.org/10.1016/j.cger.2013.07.002.
Carlson MC, Xue QL, Zhou J, Fried LP. Executive decline and dysfunction precedes declines in memory: the Women’s Health and Aging Study II. J Gerontol A Biol Sci Med Sci. 2009;64(1):110–7. https://doi.org/10.1093/gerona/gln008.
Salthouse TA. Selective review of cognitive aging. J Int Neuropsychol Soc. 2010;16(5):754–60. https://doi.org/10.1017/S1355617710000706.
Salthouse TA, Fristoe NM, Lineweaver TT, Coon VE. Aging of attention: does the ability to divide decline? Mem Cognit. 1995;23(1):59–71. https://doi.org/10.3758/BF03210557.
Carlson MC, Hasher L, Zacks RT, Connelly SL. Aging, distraction, and the benefits of predictable location. Psychol Aging. 1995;10(3):427–36. https://doi.org/10.1037//0882-7974.10.3.427.
Salthouse TA, Mitchell DR, Skovronek E, Babcock RL. Effects of adult age and working memory on reasoning and spatial abilities. J Exp Psychol Learn Mem Cogn. 1989;15(3):507–16. https://doi.org/10.1037/0278-7393.15.3.507.
Oosterman JM, Vogels RLC, Van Harten B, et al. Assessing mental flexibility: neuroanatomical and neuropsychological correlates of the trail making test in elderly people. Clin Neuropsychol. 2010;24(2):203–19. https://doi.org/10.1080/13854040903482848.
Wecker NS, Kramer JH, Wisniewski A, Delis DC, Kaplan E. Age effects on executive ability. Neuropsychology. 2000;14(3):409–14. https://doi.org/10.1037//0894-4105.14.3.409.
Svennerholm L, Boström K, Jungbjer B. Changes in weight and compositions of major membrane components of human brain during the span of adult human life of Swedes. Acta Neuropathol. 1997;94(4):345–52. https://doi.org/10.1007/s004010050717.
Raz N, Gunning FM, Head D, et al. Selective aging of the human cerebral cortex observed in vivo: differential vulnerability of the prefrontal gray matter. Cereb Cortex. 1997;7(May):268–82.
Resnick SM, Pham DL, Kraut MA, Zonderman AB, Davatzikos C. Longitudinal magnetic resonance imaging studies of older adults: a shrinking brain. J Neurosci. 2003;23(8):3295–301. https://doi.org/10.1523/JNEUROSCI.23-08-03295.2003.
Mukherjee J, Christian BT, Dunigan KA, et al. Brain imaging of 18F-fallypride in normal volunteers: blood analysis, distribution, test-retest studies, and preliminary assessment of sensitivity to aging effects on dopamine D-2/D-3 receptors. Synapse. 2002;46(3):170–88. https://doi.org/10.1002/syn.10128.
Nyberg L, Bäckman L. Cognitive aging: a view from brain imaging. In: Dixon R, Bäckman L, Nilsson LG, editors. New frontiers in cognitive aging. Oxford: Oxford University Press; 2004. p. 135–59. https://doi.org/10.1093/acprof:oso/9780198525691.003.0007.
Müller U, Suckling J, Zelaya F, et al. Plasma level-dependent effects of methylphenidate on task-related functional magnetic resonance imaging signal changes. Psychopharmacology (Berl). 2005. https://doi.org/10.1007/s00213-005-2264-9.
Ben-Itzhak R, Giladi N, Gruendlinger L, Hausdorff JM. Can methylphenidate reduce fall risk in community-living older adults? A double-blind, single-dose cross-over study. J Am Geriatr Soc. 2008. https://doi.org/10.1111/j.1532-5415.2007.01623.x.
Izquierdo I, Bevilaqua LR, Rossato JI, Lima RH, Medina JH, Cammarota M. Age-dependent and age-independent human memory persistence is enhanced by delayed posttraining methylphenidate administration. Proc Natl Acad Sci USA. 2008. https://doi.org/10.1073/pnas.0810650105.
Ble A, Volpato S, Zuliani G, et al. Executive function correlates with walking speed in older persons: the InCHIANTI study. J Am Geriatr Soc. 2005. https://doi.org/10.1111/j.1532-5415.2005.53157.x.
Springer S, Giladi N, Peretz C, Yogev G, Simon ES, Hausdorff JM. Dual-tasking effects on gait variability: het role of aging, falls, and executive function. Mov Disord. 2006. https://doi.org/10.1002/mds.20848.
Hausdorff JM, Yogev G, Springer S, Simon ES, Giladi N. Walking is more like catching than tapping: gait in the elderly as a complex cognitive task. Exp Brain Res. 2005. https://doi.org/10.1007/s00221-005-2280-3.
Verghese J, Buschke H, Viola L, et al. Validity of divided attention tasks in predicting falls in older individuals: a preliminary study. J Am Geriatr Soc. 2002. https://doi.org/10.1046/j.1532-5415.2002.50415.x.
Prendergast MA, Jackson WJ, Terry AV, et al. Age-related differences in distractibility and response to methylphenidate in monkeys. Cereb Cortex. 1998;8(2):164–72. https://doi.org/10.1093/cercor/8.2.164.
Bhattacharya SE, Shumsky JS, Waterhouse BD. Attention enhancing effects of methylphenidate are age-dependent. Exp Gerontol. 2015;61:1–7. https://doi.org/10.1016/j.exger.2014.11.006.
Sahakian BJ. What do experts think we should do to achieve brain health? Neurosci Biobehav Rev. 2014. https://doi.org/10.1016/j.neubiorev.2014.04.002.
Gustavsson A, Svensson M, Jacobi F, et al. Cost of disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011. https://doi.org/10.1016/j.euroneuro.2011.08.008.
Biederman J, Faraone S, Milberger S, et al. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry. 1996;53(5):437–46. https://doi.org/10.1001/archpsyc.1996.01830050073012.
Heiligenstein E, Guenther G, Levy A, Savino F, Fulwiler J. Psychological and academic functioning in college students with attention deficit hyperactivity disorder. J Am Coll Health. 1999;47(4):181–5. https://doi.org/10.1080/07448489909595644.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Cherkasova MV, Hechtman L. Neuroimaging in attention-deficit hyperactivity disorder: beyond the frontostriatal circuitry. Can J Psychiatry. 2009;54(10):651–64. https://doi.org/10.1177/070674370905401002.
Giedd JN, Rapoport JL. Structural MRI of pediatric brain development: what have we learned and where are we going? Neuron. 2010;67(5):728–34. https://doi.org/10.1016/j.neuron.2010.08.040.
Dickstein SG, Bannon K, Xavier Castellanos F, Milham MP. The neural correlates of attention deficit hyperactivity disorder: an ALE meta-analysis. J Child Psychol Psychiatry Allied Discip. 2006;47(10):1051–62. https://doi.org/10.1111/j.1469-7610.2006.01671.x.
Shaw P, Lerch J, Greenstein D, et al. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63(5):540–9. https://doi.org/10.1001/archpsyc.63.5.540.
Willcutt EG, Doyle AE, Nigg JT, Faraone S, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry. 2005;57(11):1336–46. https://doi.org/10.1016/j.biopsych.2005.02.006.
World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
Bradley C. The behavior of children receiving benzedrine. Am J Psychiatry. 1937;94(3):577–85. https://doi.org/10.1176/appi.ajp.94.3.577.
Elia J, Borcherding BG, Rapoport JL, Keysor CS. Methylphenidate and dextroamphetamine treatments of hyperactivity: are there true nonresponders? Psychiatry Res. 1991;36(2):141–55. https://doi.org/10.1016/0165-1781(91)90126-A.
Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA. 2016. https://doi.org/10.1001/jama.2016.5453.
Advokat C, Scheithauer M. Attention-deficit hyperactivity disorder (ADHD) stimulant medications as cognitive enhancers. Front Neurosci. 2013. https://doi.org/10.3389/fnins.2013.00082.
Kempton S, Vance A, Maruff P, Luk E, Costin J, Pantelis C. Executive function and attention deficit hyperactivity disorder: stimulant medication and better executive function performance in children. Psychol Med. 1999;29(3):527–38. https://doi.org/10.1017/S0033291799008338.
Mehta MA, Goodyer IM, Sahakian BJ. Methylphenidate improves working memory and set-shifting in AD/HD: relationships to baseline memory capacity. J Child Psychol Psychiatry Allied Discip. 2004;45(2):293–305. https://doi.org/10.1111/j.1469-7610.2004.00221.x.
Strand MT, Hawk LW, Bubnik M, Shiels K, Pelham WE, Waxmonsky JG. Improving working memory in children with attention-deficit/hyperactivity disorder: the separate and combined effects of incentives and stimulant medication. J Abnorm Child Psychol. 2012. https://doi.org/10.1007/s10802-012-9627-6.
Yarmolovsky J, Szwarc T, Schwartz M, Tirosh E, Geva R. Hot executive control and response to a stimulant in a double-blind randomized trial in children with ADHD. Eur Arch Psychiatry Clin Neurosci. 2017. https://doi.org/10.1007/s00406-016-0683-8.
Maul J, Advokat C. Stimulant medications for attention-deficit/hyperactivity disorder (ADHD) improve memory of emotional stimuli in ADHD-diagnosed college students. Pharmacol Biochem Behav. 2013. https://doi.org/10.1016/j.pbb.2013.01.021.
Bolfer C, Pacheco SP, Tsunemi MH, Carreira WS, Casella BB, Casella EB. Attention-deficit/hyperactivity disorder: the impact of methylphenidate on working memory, inhibition capacity and mental flexibility. Arq Neuropsiquiatr. 2017. https://doi.org/10.1590/0004-282x20170030.
Rubio Morell B, Hernández Expósito S. Differential long-term medication impact on executive function and delay aversion in ADHD. Appl Neuropsychol Child. 2019. https://doi.org/10.1080/21622965.2017.1407653.
Orban SA, Karamchandani TA, Tamm L, et al. Attention-deficit/hyperactivity disorder-related deficits and psychostimulant medication effects on comprehension of audiovisually presented educational material in children. J Child Adolesc Psychopharmacol. 2018. https://doi.org/10.1089/cap.2018.0006.
Hawk LW, Fosco WD, Colder CR, Waxmonsky JG, Pelham WE, Rosch KS. How do stimulant treatments for ADHD work? Evidence for mediation by improved cognition. J Child Psychol Psychiatry Allied Discip. 2018. https://doi.org/10.1111/jcpp.12917.
Kortekaas-Rijlaarsdam AF, Luman M, Sonuga-Barke E, Bet P, Oosterlaan J. Methylphenidate-related improvements in math performance cannot be explained by better cognitive functioning or higher academic motivation: evidence from a randomized controlled trial. J Atten Disord. 2017. https://doi.org/10.1177/1087054717713640.
Coghill DR, Seth S, Pedroso S, Usala T, Currie J, Gagliano A. Effects of methylphenidate on cognitive functions in children and adolescents with attention-deficit/hyperactivity disorder: evidence from a systematic review and a meta-analysis. Biol Psychiatry. 2014. https://doi.org/10.1016/j.biopsych.2013.10.005.
Rubia K, Alegria AA, Cubillo AI, Smith AB, Brammer MJ, Radua J. Effects of stimulants on brain function in attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Biol Psychiatry. 2014. https://doi.org/10.1016/j.biopsych.2013.10.016.
Abikoff H, Hechtman L, Klein RG, et al. Symptomatic improvement in children with ADHD treated with long-term methylphenidate and multimodal psychosocial treatment. J Am Acad Child Adolesc Psychiatry. 2004. https://doi.org/10.1097/01.chi.0000128791.10014.ac.
Turner DC, Blackwell AD, Dowson JH, McLean A, Sahakian BJ. Neurocognitive effects of methylphenidate in adult attention-deficit/hyperactivity disorder. Psychopharmacology (Berl). 2005;178(2–3):286–95. https://doi.org/10.1007/s00213-004-1993-5.
Aron AR, Dowson JH, Sahakian BJ, Robbins TW. Methylphenidate improves response inhibition in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2003;54(12):1465–8. https://doi.org/10.1016/S0006-3223(03)00609-7.
Tucha O, Mecklinger L, Laufkötter R, Klein HE, Walitza S, Lange KW. Methylphenidate-induced improvements of various measures of attention in adults with attention deficit hyperactivity disorder. J Neural Transm. 2006. https://doi.org/10.1007/s00702-005-0437-7.
Fuermaier ABM, Tucha L, Koerts J, et al. Effects of methylphenidate on memory functions of adults with ADHD. Appl Neuropsychol. 2017. https://doi.org/10.1080/23279095.2015.1124108.
Low AM, Le Sommer J, Vangkilde S, et al. Delay aversion and executive functioning in adults with attention-deficit/hyperactivity disorder: before and after stimulant treatment. Int J Neuropsychopharmacol. 2018. https://doi.org/10.1093/ijnp/pyy070.
Kubas HA, Backenson EM, Wilcox G, Piercy JC, Hale JB. The effects of methylphenidate on cognitive function in children with attention-deficit/hyperactivity disorder. Postgrad Med. 2012. https://doi.org/10.3810/pgm.2012.09.2592.
Fosco WD, Rosch KS, Waxmonsky JG, Pelham WE, Hawk LW. Baseline performance moderates stimulant effects on cognition in youth with ADHD. Exp Clin Psychopharmacol. 2020. https://doi.org/10.1037/pha0000374.
Boonstra AM, Kooij JJS, Oosterlaan J, Sergeant JA, Buitelaar JK. Does methylphenidate improve inhibition and other cognitive abilities in adults with childhood-onset ADHD? J Clin Exp Neuropsychol. 2005. https://doi.org/10.1080/13803390490515757.
Coghill DR, Rhodes SM, Matthews K. The neuropsychological effects of chronic methylphenidate on drug-naive boys with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007. https://doi.org/10.1016/j.biopsych.2006.12.030.
Bron TI, Bijlenga D, Marije Boonstra A, et al. OROS-methylphenidate efficacy on specific executive functioning deficits in adults with ADHD: a randomized, placebo-controlled cross-over study. Eur Neuropsychopharmacol. 2014. https://doi.org/10.1016/j.euroneuro.2014.01.007.
Coghill DR, Seth S, Matthews K. A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in attention deficit hyperactivity disorder: advancing beyond the three-pathway models. Psychol Med. 2014. https://doi.org/10.1017/S0033291713002547.
Hale JB, Reddy LA, Semrud-Clikeman M, et al. Executive impairment determines ADHD medication response: implications for academic achievement. J Learn Disabil. 2011. https://doi.org/10.1177/0022219410391191.
Meireles J, Massano J. Cognitive impairment and dementia in Parkinson’s disease: clinical features, diagnosis, and management. Front Neurol. 2012. https://doi.org/10.3389/fneur.2012.00088.
Galvan A, Wichmann T. Pathophysiology of Parkinsonism. Clin Neurophysiol. 2008;119(7):1459–74. https://doi.org/10.1016/j.clinph.2008.03.017.
Pillon B, Dubois B, Lhermitte F, Agid Y. Heterogeneity of cognitive impairment in progressive supranuclear palsy, Parkinson’s disease, and Alzheimer’s disease. Neurology. 1986;36(9):1179–85.
Pillon B, Dubois B, Agid Y. Severity and specificity of cognitive impairment in Alzheimer’s, Huntington’s, and Parkinson’s diseases and progressive supranuclear palsy. Ann N Y Acad Sci. 1991;640:224–7. https://doi.org/10.1212/WNL.41.5.634.
Litvan I, Mohr E, Williams J, Gomez C, Chase TN. Differential memory and executive functions in demented patients with Parkinson’s and Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 1991;54(1):25–9. https://doi.org/10.1136/jnnp.54.1.25.
Morris RG, Downes JJ, Sahakian BJ, Evenden JL, Heald A, Robbins TW. Planning and spatial working memory in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1988;51(6):757–66. https://doi.org/10.1136/jnnp.51.6.757.
Owen AM, James M, Leigh PN, et al. Fronto-striatal cognitive deficits at different stages of Parkinson’s disease. Brain. 1992;115(6):1727–51. https://doi.org/10.1093/brain/115.6.1727.
Weintraub D, Tröster AI, Marras C, Stebbins G. Initial cognitive changes in Parkinson’s disease. Mov Disord. 2018. https://doi.org/10.1002/mds.27330.
Lange KW, Robbins TW, Marsden CD, James M, Owen AM, Paul GM. l-Dopa withdrawal in Parkinson’s disease selectively impairs cognitive performance in tests sensitive to frontal lobe dysfunction. Psychopharmacology (Berl). 1992;107(2–3):394–404. https://doi.org/10.1007/BF02245167.
Murakami H, Momma Y, Nohara T, et al. Improvement in language function correlates with gait improvement in drug-naïve Parkinson’s disease patients taking dopaminergic medication. J Parkinsons Dis. 2016. https://doi.org/10.3233/JPD-150702.
Brusa L, Pavino V, Massimetti MC, Bove R, Iani C, Stanzion P. The effect of dopamine agonists on cognitive functions in non-demented early-mild Parkinson’s disease patients. Funct Neurol. 2013. https://doi.org/10.11138/FNeur/2013.28.1.007.
Morrish PK, Sawle GV, Brooks DJ. An [18F]dopa-PET and clinical study of the rate of progression in Parkinson’s disease. Brain. 1996;119(Pt 2):585–91. https://doi.org/10.1093/brain/119.2.585.
Cools R. Dopaminergic modulation of cognitive function-implications for l-DOPA treatment in Parkinson’s disease. Neurosci Biobehav Rev. 2006;30(1):1–23. https://doi.org/10.1016/j.neubiorev.2005.03.024.
Swainson R, Rogers RD, Sahakian BJ, Summers BA, Polkey CE, Robbins TW. Probabilistic learning and reversal deficits in patients with Parkinson’s disease or frontal or temporal lobe lesions: possible adverse effects of dopaminergic medication. Neuropsychologia. 2000;38(5):596–612. https://doi.org/10.1016/S0028-3932(99)00103-7.
Cools R, Barker RA, Sahakian BJ, Robbins TW. l-Dopa medication remediates cognitive inflexibility, but increases impulsivity in patients with Parkinson’s disease. Neuropsychologia. 2003;41(11):1431–41. https://doi.org/10.1016/S0028-3932(03)00117-9.
Cools R. Enhanced or impaired cognitive function in Parkinson’s disease as a function of dopaminergic medication and task demands. Cereb Cortex. 2001. https://doi.org/10.1093/cercor/11.12.1136.
Bohnen NI, Kaufer DI, Ivanco LS, et al. Cortical cholinergic function is more severely affected in parkinsonian dementia than in Alzheimer disease: an in vivo positron emission tomographic study. Arch Neurol. 2003. https://doi.org/10.1001/archneur.60.12.1745.
Tiraboschi P, Hansen LA, Alford M, et al. Cholinergic dysfunction in diseases with LEWY bodies. Neurology. 2000. https://doi.org/10.1212/wnl.54.2.407.
Wang HF, Yu JT, Tang SW, et al. Efficacy and safety of cholinesterase inhibitors and memantine in cognitive impairment in Parkinson’s disease, Parkinson’s disease dementia, and dementia with Lewy bodies: systematic review with meta-analysis and trial sequential analysis. J Neurol Neurosurg Psychiatry. 2015. https://doi.org/10.1136/jnnp-2014-307659.
Litvinenko IV, Odinak MM, Mogil’naya VI, Emelin AYU. Efficacy and safety of galantamine (reminyl) for dementia in patients with Parkinson’s disease (an open controlled trial). Neurosci Behav Physiol. 2008. https://doi.org/10.1007/s11055-008-9077-3.
Mamikonyan E, Xie SX, Melvin E, Weintraub D. Rivastigmine for mild cognitive impairment in Parkinson disease: a placebo-controlled study. Mov Disord. 2015. https://doi.org/10.1002/mds.26236.
Li Z, Yu Z, Zhang J, et al. Impact of rivastigmine on cognitive dysfunction and falling in Parkinson’s disease patients. Eur Neurol. 2015. https://doi.org/10.1159/000438824.
Litvinenko IV, Odinak MM, Mogil’naya VI, Perstnev SV. Use of memantine (akatinol) for the correction of cognitive impairments in Parkinson’s disease complicated by dementia. Neurosci Behav Physiol. 2010. https://doi.org/10.1007/s11055-009-9244-1.
Pillon B, Dubois B, Cusimano G, Bonnet AM, Lhermitte F, Agid Y. Does cognitive impairment in Parkinson’s disease result from non-dopaminergic lesions? J Neurol Neurosurg Psychiatry. 1989;52(2):201–6. https://doi.org/10.1136/jnnp.52.2.201.
Zarow C, Lyness SA, Mortimer JA, Chui HC. Neuronal loss is greater in the locus coeruleus than nucleus basalis and substantia nigra in Alzheimer and Parkinson diseases. Arch Neurol. 2003;60(3):337–41. https://doi.org/10.1001/archneur.60.3.337.
Marsh L, Biglan K, Gerstenhaber M, Williams JR. Atomoxetine for the treatment of executive dysfunction in Parkinson’s disease: a pilot open-label study. Mov Disord. 2009;24(2):277–82. https://doi.org/10.1002/mds.22307.
Devos D, Moreau C, Delval A, Dujardin K, Defebvre L, Bordet R. Methylphenidate: a treatment for Parkinson’s disease? CNS Drugs. 2013;27(1):1–14. https://doi.org/10.1007/s40263-012-0017-y.
Fox SH, Lang AE. Levodopa-related motor complications: phenomenology. Mov Disord. 2008;23(Suppl. 3):S509–14. https://doi.org/10.1002/mds.22021.
Camicioli R, Lea E, Nutt JG, Sexton G, Oken BS. Methylphenidate increases the motor effects of l-dopa in Parkinson’s disease: a pilot study. Clin Neuropharmacol. 2001;24(4):208–13. https://doi.org/10.1097/00002826-200107000-00003.
Auriel E, Hausdorff JM, Herman T, Simon ES, Giladi N. Effects of methylphenidate on cognitive function and gait in patients with Parkinson’s disease: a pilot study. Clin Neuropharmacol. 2006;29(1):15–7. https://doi.org/10.1097/00002826-200601000-00005.
Devos D, Krystkowiak P, Clement F, et al. Improvement of gait by chronic, high doses of methylphenidate in patients with advanced Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2007;78(5):470–5. https://doi.org/10.1136/jnnp.2006.100016.
Delval A, Moreau C, Bleuse S, et al. Gait and attentional performance in freezers under methylphenidate. Gait Posture. 2015;41(2):384–8. https://doi.org/10.1016/j.gaitpost.2014.10.022.
van Os J, Kapur S. Schizophrenia. Lancet. 2009. https://doi.org/10.1016/S0140-6736(09)60995-8.
Liddle PF. The symptoms of chronic schizophrenia: a re-examination of the positive-negative dichotomy. Br J Psychiatry. 1987. https://doi.org/10.1192/bjp.151.2.145.
Andreasen NC, Flashman L, Flaum M, et al. Regional brain abnormalities in schizophrenia measured with magnetic resonance imaging. JAMA. 1994. https://doi.org/10.1001/jama.1994.03520220057031.
Pogarell O, Koch W, Karch S, et al. Dopaminergic neurotransmission in patients with schizophrenia in relation to positive and negative symptoms. Pharmacopsychiatry. 2012. https://doi.org/10.1055/s-0032-1306313.
da Silva Alves F, Figee M, van Avamelsvoort T, Veltman D, de Haan L. The revised dopamine hypothesis of schizophrenia: evidence from pharmacological MRI studies with atypical antipsychotic medication. Psychopharmacol Bull. 2008. https://doi.org/10.1016/S0920-9964(08)70291-3.
Wright IC, Rabe-Hesketh S, Woodruff PWR, David AS, Murray RM, Bullmore ET. Meta-analysis of regional brain volumes in schizophrenia. Am J Psychiatry. 2000. https://doi.org/10.1176/ajp.157.1.16.
Andreasen NC. Linking mind and brain in the study of mental illnesses: a project for a scientific psychopathology. Science. 1997. https://doi.org/10.1126/science.275.5306.1586.
Buchsbaum MS, Someya T, Teng CY, et al. PET and MRI of the thalamus in never-medicated patients with schizophrenia. Am J Psychiatry. 1996. https://doi.org/10.1176/ajp.153.2.191.
Weinberger DR, Berman KF, Zec RF. Physiologic dysfunction of dorsolateral prefrontal cortex in schizophrenia: I. Regional cerebral blood flow evidence. Arch Gen Psychiatry. 1986. https://doi.org/10.1001/archpsyc.1986.01800020020004.
Barnett JH, Robbins TW, Leeson VC, Sahakian BJ, Joyce EM, Blackwell AD. Assessing cognitive function in clinical trials of schizophrenia. Neurosci Biobehav Rev. 2010. https://doi.org/10.1016/j.neubiorev.2010.01.012.
Bilder RM, Lieberman JA, Kim Y, Alvir JM, Reiter G. Methylphenidate and neuroleptic effects on oral word production in schizophrenia. Neuropsychiatry Neuropsychol Behav Neurol. 1992;5(4):262–71.
Szeszko PR, Bilder RM, Dunlop JA, Walder DJ, Lieberman JA. Longitudinal assessment of methylphenidate effects on oral word production and symptoms in first-episode schizophrenia at acute and stabilized phases. Biol Psychiatry. 1999. https://doi.org/10.1016/S0006-3223(98)00258-3.
Barch DM, Carter CS. Amphetamine improves cognitive function in medicated individuals with schizophrenia and in healthy volunteers. Schizophr Res. 2005. https://doi.org/10.1016/j.schres.2004.12.019.
Pietrzak RH, Snyder PJ, Maruff P. Use of an acute challenge with d-amphetamine to model cognitive improvement in chronic schizophrenia. Hum Psychopharmacol. 2010. https://doi.org/10.1002/hup.1118.
Solmi M, Fornaro M, Toyoshima K, et al. Systematic review and exploratory meta-analysis of the efficacy, safety, and biological effects of psychostimulants and atomoxetine in patients with schizophrenia or schizoaffective disorder. CNS Spectr. 2019. https://doi.org/10.1017/S1092852918001050.
Jody D, Lieberman JA, Geisler S, Szymanski S, Alvir JMJ. Behavioral response to methylphenidate and treatment outcome in first episode schizophrenia. Psychopharmacol Bull. 1990;26(2):224–30.
Koreen AR, Lieberman JA, Alvir J, Chakos M. The behavioral effect of m-chlorophenylpiperazine (mCPP) and methylphenidate in first-episode schizophrenia and normal controls. Neuropsychopharmacology. 1997. https://doi.org/10.1016/S0893-133X(96)00160-1.
Levy DL, Smith M, Robinson D, et al. Methylphenidate increases thought disorder in recent onset schizophrenics, but not in normal controls. Biol Psychiatry. 1993. https://doi.org/10.1016/0006-3223(93)90192-G.
Lieberman JA, Kane JM, Sarantakos S, et al. Prediction of relapse in schizophrenia. Arch Gen Psychiatry. 1987. https://doi.org/10.1001/archpsyc.1987.01800190013002.
Lieberman JA, Kane JM, Gadaleta D, Brenner R, Lesser MS, Kinon B. Methylphenidate challenge as a predictor of relapse in schizophrenia. Am J Psychiatry. 1984. https://doi.org/10.1176/ajp.141.5.633.
Carpenter MD, Winsberg BG, Camus LA. Methylphenidate augmentation therapy in schizophrenia. J Clin Psychopharmacol. 1992. https://doi.org/10.1097/00004714-199208000-00010.
Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. 2007;369(9566):1047–53. https://doi.org/10.1016/S0140-6736(07)60464-4.
Diller LH. The run on ritalin: attention deficit disorder and stimulant treatment in the 1990s. Hastings Cent Rep. 1996;26(2):12. https://doi.org/10.2307/3528571.
Klein-Schwartz W. Abuse and toxicity of methylphenidate. Curr Opin Pediatr. 2002;14(2):219–23. https://doi.org/10.1097/00008480-200204000-00013.
Repantis D, Schlattmann P, Laisney O, Heuser I. Modafinil and methylphenidate for neuroenhancement in healthy individuals: a systematic review. Pharmacol Res. 2010;62(3):187–206. https://doi.org/10.1016/j.phrs.2010.04.002.
White SR, Yadao CM. Characterization of methylphenidate exposures reported to a regional poison control center. Arch Pediatr Adolesc Med. 2000;154(12):1199–203.
Kimko HC, Cross JT, Abernethy DR. Pharmacokinetics and clinical effectiveness of methylphenidate. Clin Pharmacokinet. 1999;37(6):457–70. https://doi.org/10.2165/00003088-199937060-00002.
Pliszka S. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(7):894–921. https://doi.org/10.1097/chi.0b013e318054e724.
Lakhan SE, Kirchgessner A. Prescription stimulants in individuals with and without attention deficit hyperactivity disorder: misuse, cognitive impact, and adverse effects. Brain Behav. 2012;2(5):661–7. https://doi.org/10.1002/brb3.78.
Kelly KL, Rapport MD, DuPaul GJ. Attention deficit disorder and methylphenidate: a multi-step analysis of dose-response effects on children’s cardiovascular functioning. Int Clin Psychopharmacol. 1988;3:167–81.
Liang EF, Lim SZ, Tam WW, et al. The effect of methylphenidate and atomoxetine on heart rate and systolic blood pressure in young people and adults with attention-deficit hyperactivity disorder (ADHD): systematic review, meta-analysis, and meta-regression. Int J Environ Res Public Health. 2018. https://doi.org/10.3390/ijerph15081789.
Wilens TE, Biederman J, Lerner M. Effects of once-daily osmotic-release methylphenidate on blood pressure and heart rate in children with attention-deficit/hyperactivity disorder: results from a one-year follow-up study. J Clin Psychopharmacol. 2004. https://doi.org/10.1097/01.jcp.0000106223.36344.df.
Cooper WO, Habel LA, Sox CM, et al. ADHD medications and serious cardiovascular events in children and youth. N Engl J Med. 2011. https://doi.org/10.3109/10641955.2015.1046604.
Shin JY, Roughead EE, Park BJ, Pratt NL. Cardiovascular safety of methylphenidate among children and young people with attention-deficit/hyperactivity disorder (ADHD): nationwide self controlled case series study. BMJ. 2016. https://doi.org/10.1136/bmj.i2550.
Biederman J, Mick E, Surman C, et al. A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2006. https://doi.org/10.1016/j.biopsych.2005.09.011.
Rösler M, Fischer R, Ammer R, Ose C, Retz W. A randomised, placebo-controlled, 24-week, study of low-dose extended-release methylphenidate in adults with attention-deficit/hyperactivity disorder. Eur Arch Psychiatry Clin Neurosci. 2009. https://doi.org/10.1007/s00406-008-0845-4.
Adler LA, Zimmerman B, Starr HL, et al. Efficacy and safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, double-blind, parallel group, dose-escalation study. J Clin Psychopharmacol. 2009. https://doi.org/10.1097/JCP.0b013e3181a390ce.
Adler LA, Orman C, Starr HL, et al. Long-term safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: an open-label, dose-titration, 1-year study. J Clin Psychopharmacol. 2011. https://doi.org/10.1097/JCP.0b013e318203ea0a.
Hill SL, El-Khayat RH, Sandilands EA, Thomas SHL. Electrocardiographic effects of methylphenidate overdose. Clin Toxicol. 2010. https://doi.org/10.3109/15563651003720234.
Klampfl K, Quattländer A, Burger R, Pfuhlmann B, Warnke A, Gerlach M. Case report: intoxication with high dose of long-acting methylphenidate (Concerta®) in a suicidal 14-year-old girl. Atten Deficit Hyperact Disord. 2010. https://doi.org/10.1007/s12402-010-0032-0.
Ozdemir E, Karaman MG, Yurteri N, Erdogan A. A case of suicide attempt with long-acting methylphenidate (Concerta). Atten Deficit Hyperact Disord. 2010. https://doi.org/10.1007/s12402-010-0026-y.
Hammerness P, Wilens T, Mick E, et al. Cardiovascular effects of longer-term, high-dose OROS methylphenidate in adolescents with attention deficit hyperactivity disorder. J Pediatr. 2009. https://doi.org/10.1016/j.jpeds.2009.02.008.
Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011. https://doi.org/10.1001/jama.2011.1830.
Kraemer M, Uekermann J, Wiltfang J, Kis B. Methylphenidate-induced psychosis in adult attention-deficit/hyperactivity disorder: report of 3 new cases and review of the literature. Clin Neuropharmacol. 2010. https://doi.org/10.1097/WNF.0b013e3181e29174.
Barrett SP, Darredeau C, Bordy LE, Pihl RO. Characteristics of methylphenidate misuse in a university student sample. Can J Psychiatry. 2005. https://doi.org/10.1177/070674370505000805.
Ross R. Psychotic and manic-like symptoms during stimulant treatment of attention deficit hyperactivity disorder. Am J Psychiatry. 2006. https://doi.org/10.1176/appi.ajp.163.7.1149.
Eiland LS, Bell EA, Erramouspe J. Priapism associated with the use of stimulant medications and atomoxetine for attention-deficit/hyperactivity disorder in children. Ann Pharmacother. 2014. https://doi.org/10.1177/1060028014541791.
Tong HY, Díaz C, Collantes E, et al. Liver transplant in a patient under methylphenidate therapy: a case report and review of the literature. Case Rep Pediatr. 2015. https://doi.org/10.1155/2015/437298.
Storebø OJ, Pedersen N, Ramstad E, et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents: assessment of adverse events in non-randomised studies. Cochrane Database Syst Rev. 2018;5(5):CD012069. https://doi.org/10.1002/14651858.cd012069.pub2.
Volkow ND, Wang GJ, Fowler JS, et al. Reinforcing effects of psychostimulants in humans are associated with increases in brain dopamine and occupancy of D(2) receptors. J Pharmacol Exp Ther. 1999;291(1):409–15.
Musser CJ, Ahmann PA, Theye FW, Mundt P, Broste SK, Mueller-Rizner N. Stimulant use and the potential for abuse in Wisconsin as reported by school administrators and longitudinally followed children. J Dev Behav Pediatr. 1998;19(3):187–92. https://doi.org/10.1097/00004703-199806000-00006.
Brady JV, Griffiths RR, Hienz RD, Ator NA, Lukas SE, Lamb RJ. Assessing drugs for abuse liability and dependence potential in laboratory primates. In: Bozarth MA, editor. Methods of assessing the reinforcing properties of abused drugs. New York: Springer; 1987. p. 45–85. https://doi.org/10.1007/978-1-4612-4812-5_3.
Schuster CR. Testing and abuse liability of drugs in humans. NIDA Res Monogr. 1989;92:1–6.
Bergman J, Madras BK, Johnson SE, Spealman RD. Effects of cocaine and related drugs in nonhuman primates. III. Self-administration by squirrel monkeys. J Pharmacol Exp Ther. 1989;251(1):150–5.
Chait LD. Reinforcing and subjective effects of methylphenidate in humans. Behav Pharmacol. 1994;5(3):281–8. https://doi.org/10.1097/00008877-199406000-00005.
Emmett-Oglesby MW, Wurst M, Lal H. Discriminative stimulus properties of a small dose of cocaine. Neuropharmacology. 1983;22(1):97–101. https://doi.org/10.1016/0028-3908(83)90266-6.
Wood DM, Emmett-Oglesby MW. Substitution and cross-tolerance profiles of anorectic drugs in rats trained to detect the discriminative stimulus properties of cocaine. Psychopharmacology (Berl). 1988;95(3):364–8. https://doi.org/10.1007/BF00181948.
Evans SM, Johanson CE. Amphetamine-like effects of anorectics and related compounds in pigeons. J Pharmacol Exp Ther. 1987;241(3):817–25.
Huang JT, Ho BT. Discriminative stimulus properties of d-amphetamine and related compounds in rats. Pharmacol Biochem Behav. 1974;2(5):669–73. https://doi.org/10.1016/0091-3057(74)90036-7.
Heishman SJ, Henningfield JE. Discriminative stimulus effects of d-amphetamine, methylphenidate, and diazepam in humans. Psychopharmacology (Berl). 1991;103(4):436–42. https://doi.org/10.1007/BF02244241.
Rush CR, Kollins SH, Pazzaglia PJ. Discriminative-stimulus and participant-rated effects of methylphenidate, bupropion, and triazolam in d-amphetamine-trained humans. Exp Clin Psychopharmacol. 1998;6(1):32–44. https://doi.org/10.1037/1064-1297.6.1.32.
Sevak RJ, Stoops WW, Hays LR, Rush CR. Discriminative stimulus and subject-rated effects of methamphetamine, d-amphetamine, methylphenidate, and triazolam in methamphetamine-trained humans. J Pharmacol Exp Ther. 2009;328(3):1007–18. https://doi.org/10.1124/jpet.108.147124.
Arnsten AFT. Stress signalling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009. https://doi.org/10.1038/nrn2648.
Arnsten AFT. Development of the cerebral cortex: XIV. Stress impairs prefrontal cortical function. J Am Acad Child Adolesc Psychiatry. 1999. https://doi.org/10.1097/00004583-199902000-00024.
Urban KR, Waterhouse BD, Gao WJ. Distinct age-dependent effects of methylphenidate on developing and adult prefrontal neurons. Biol Psychiatry. 2012;72(10):880–8. https://doi.org/10.1016/j.biopsych.2012.04.018.
Urban KR, Li YC, Gao WJ. Treatment with a clinically-relevant dose of methylphenidate alters NMDA receptor composition and synaptic plasticity in the juvenile rat prefrontal cortex. Neurobiol Learn Mem. 2013;101:65–74. https://doi.org/10.1016/j.nlm.2013.01.004.
Urban KR, Gao W-J. Psychostimulants as cognitive enhancers in adolescents: more risk than reward? Front Public Health. 2017;5:260. https://doi.org/10.3389/fpubh.2017.00260.
Inglis SK, Carucci S, Garas P, et al. Prospective observational study protocol to investigate long-term adverse effects of methylphenidate in children and adolescents with ADHD: the Attention Deficit Hyperactivity Disorder Drugs Use Chronic Effects (ADDUCE) study. BMJ Open. 2016;6(4):e010433. https://doi.org/10.1136/bmjopen-2015-010433.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received to undertake this research.
Conflict of Interest
Ajay Kapur has no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kapur, A. Is Methylphenidate Beneficial and Safe in Pharmacological Cognitive Enhancement?. CNS Drugs 34, 1045–1062 (2020). https://doi.org/10.1007/s40263-020-00758-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00758-w